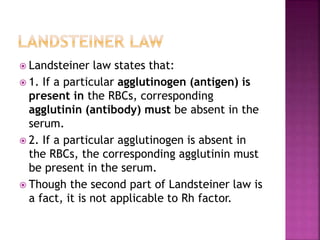
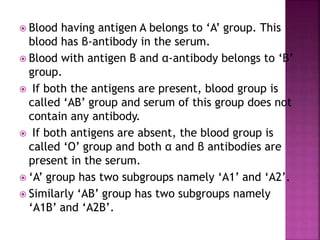
Karl Landsteiner discovered the ABO blood group system in 1901 by observing that mixing blood from different people sometimes caused clumping of red blood cells. He identified the A and B antigens on red blood cells and the corresponding anti-A and anti-B antibodies in plasma. Based on the presence or absence of these antigens and antibodies, he classified blood into the A, B, AB, and O groups. Landsteiner's discovery explained why blood transfusions were sometimes successful and sometimes caused fatal reactions.