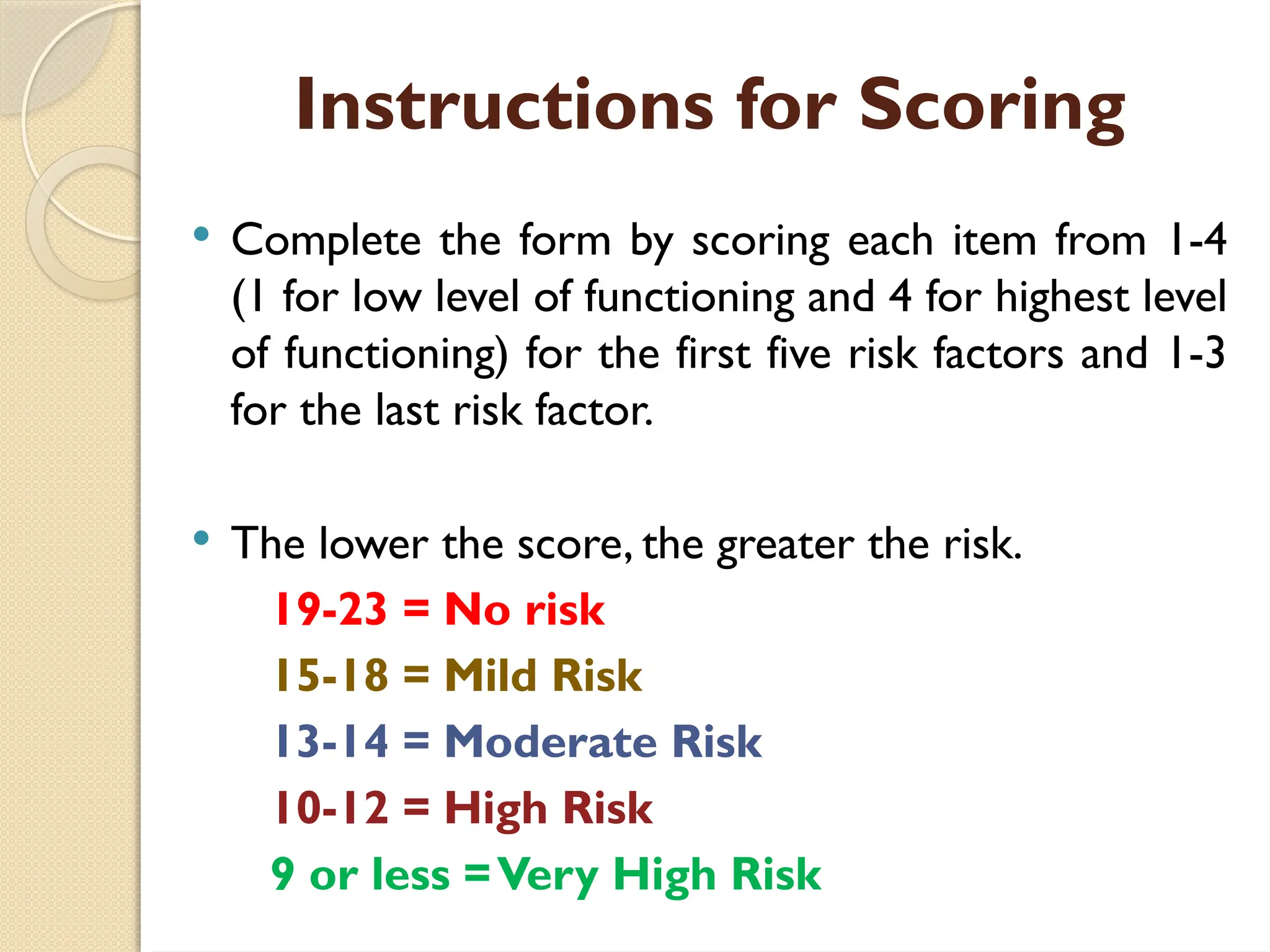
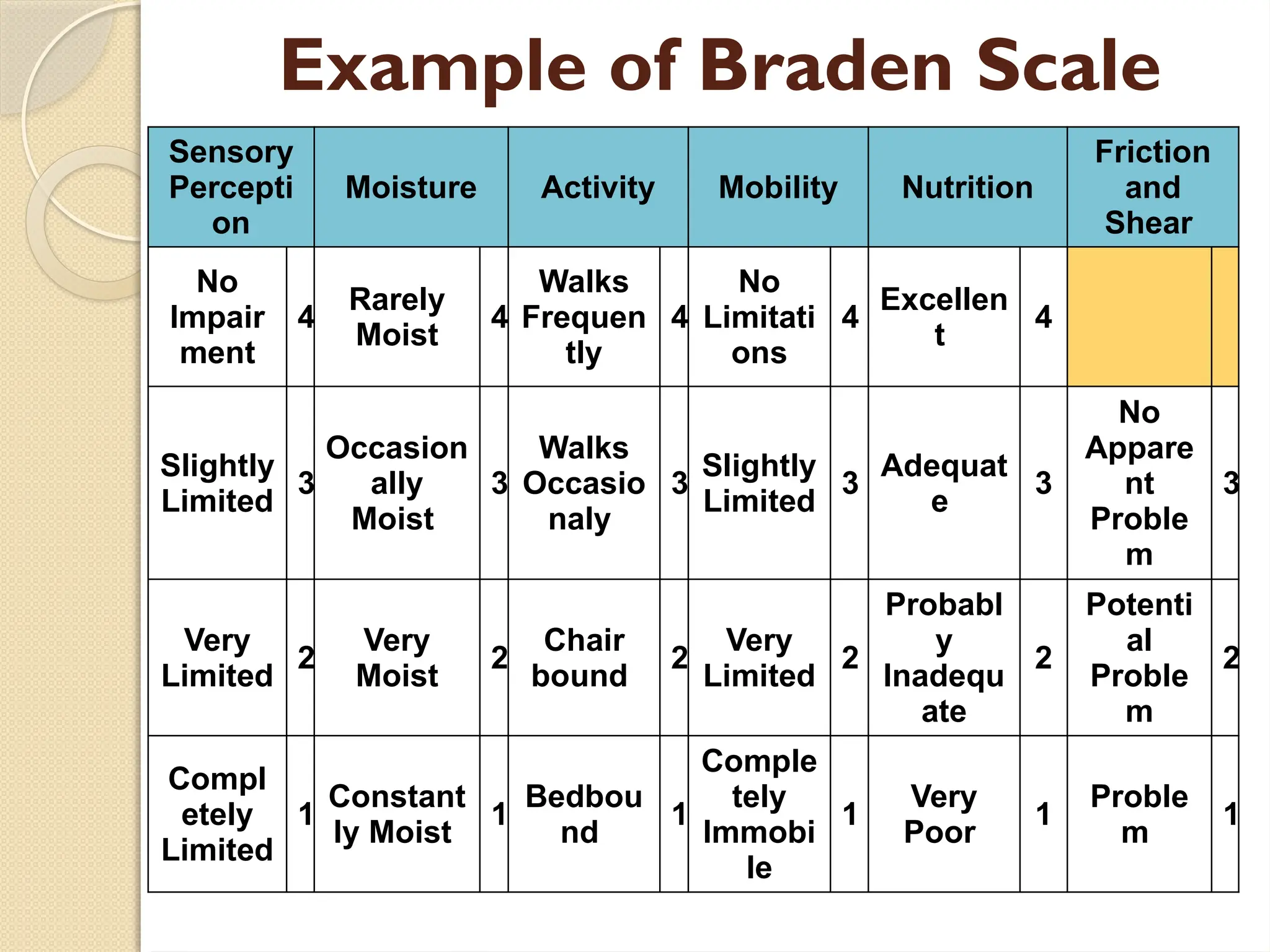
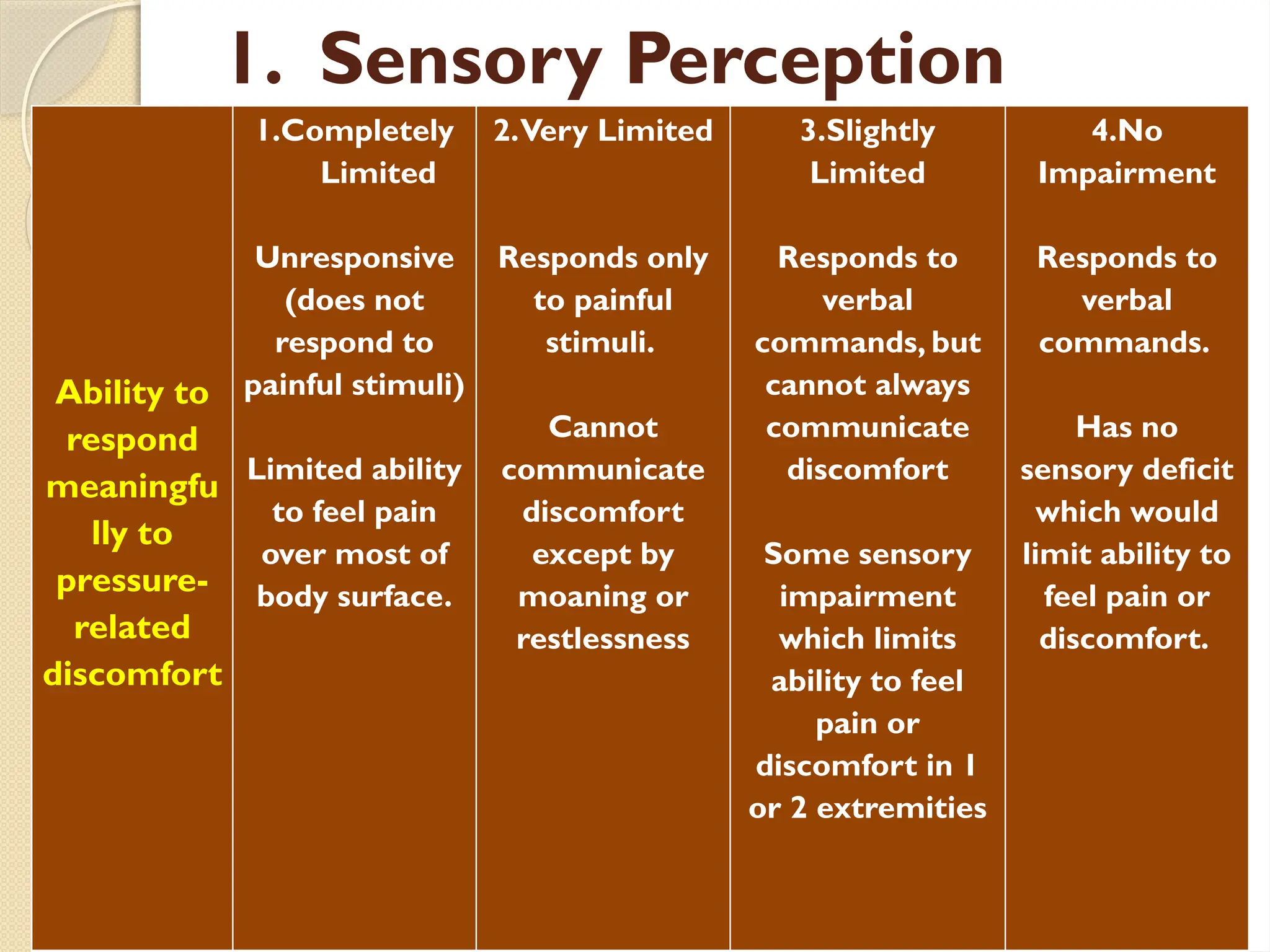
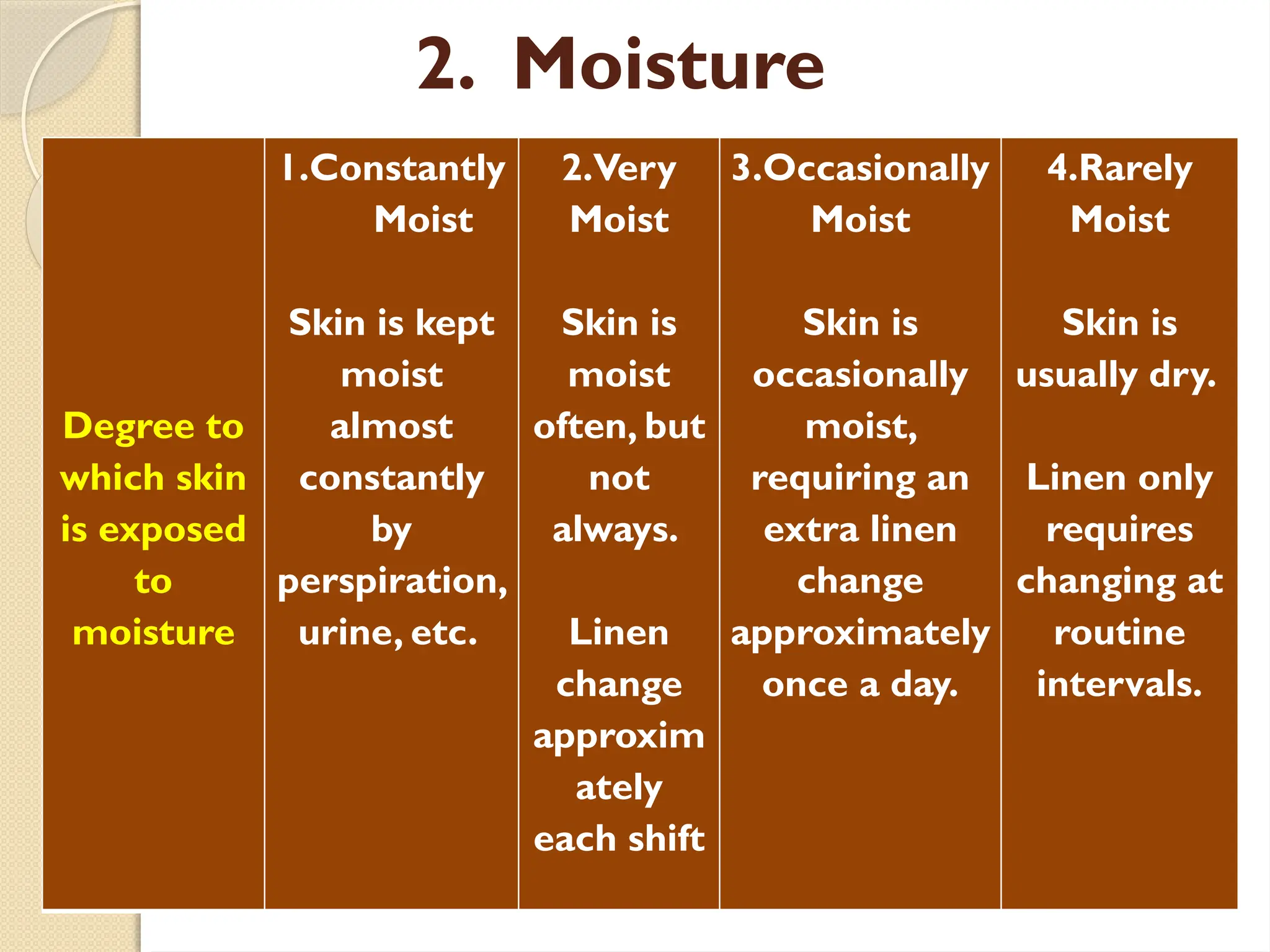
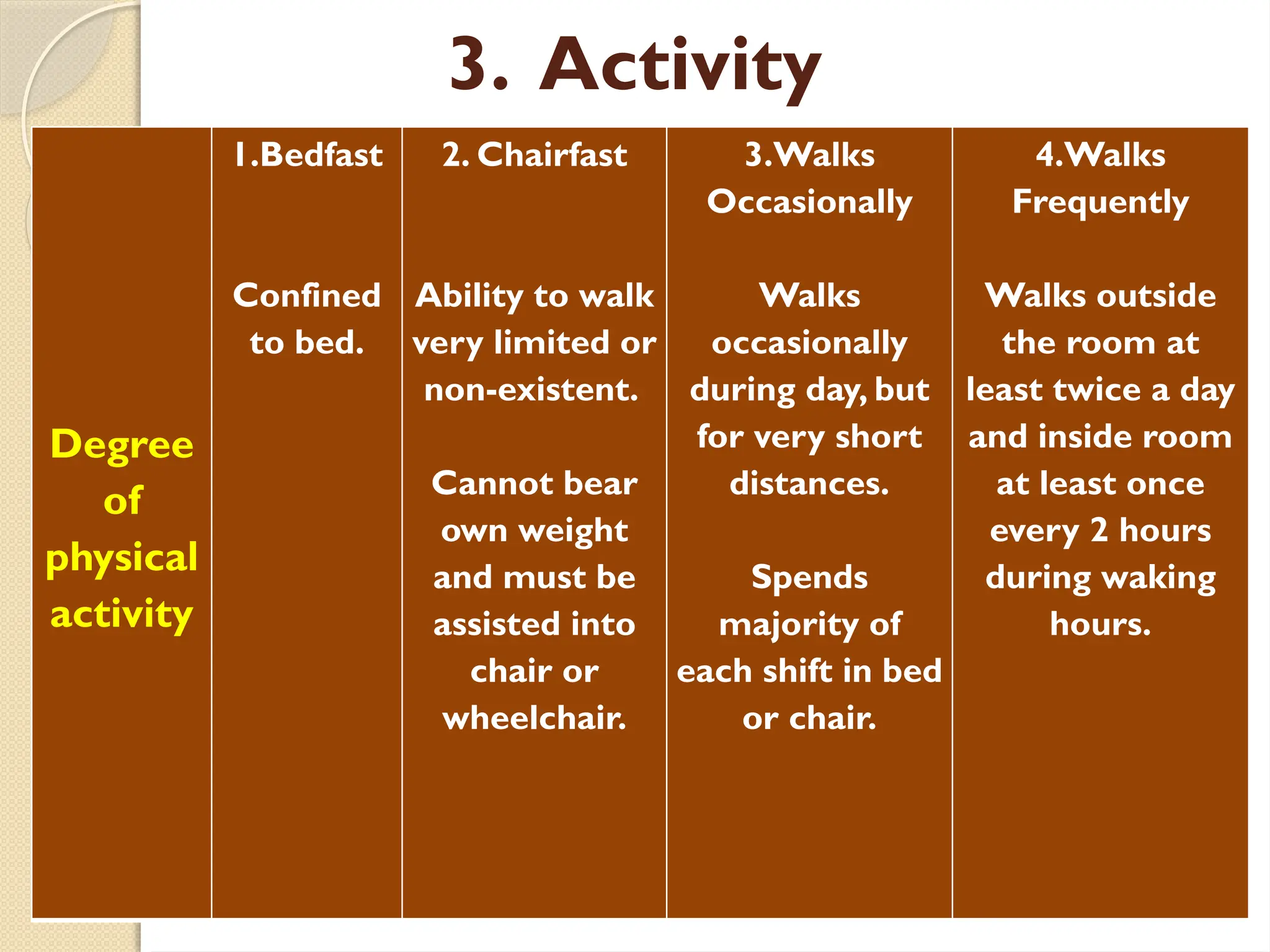
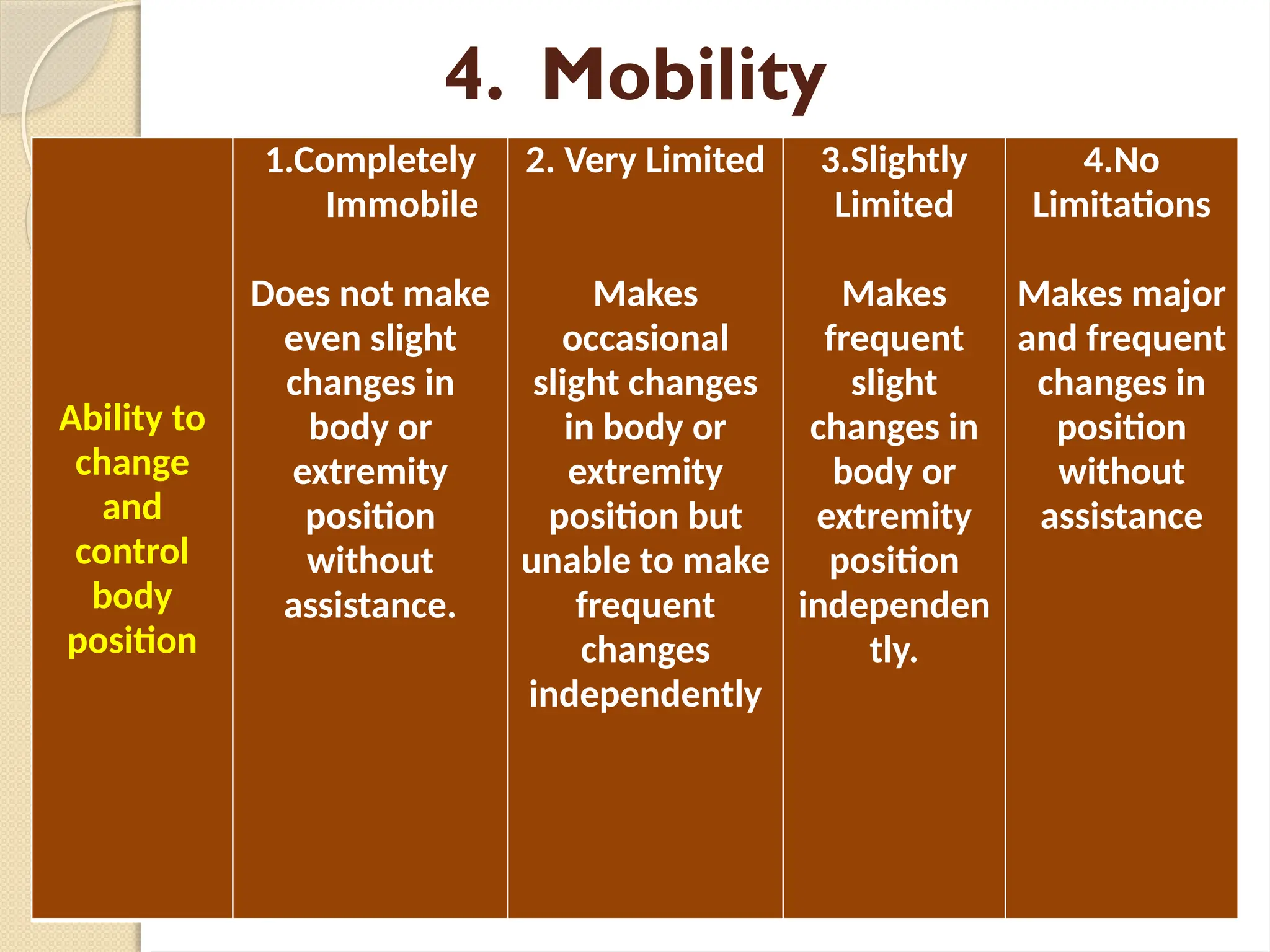
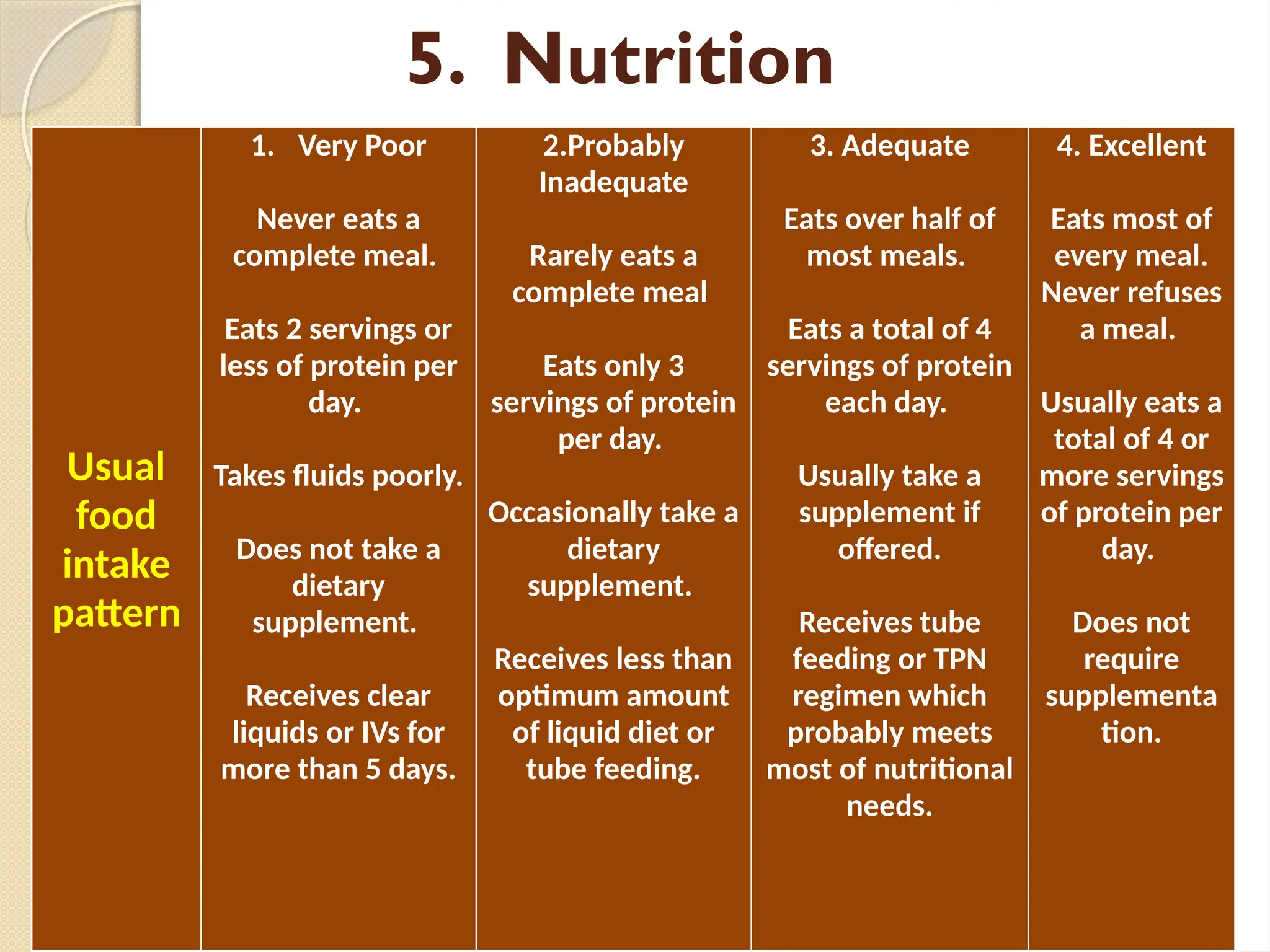
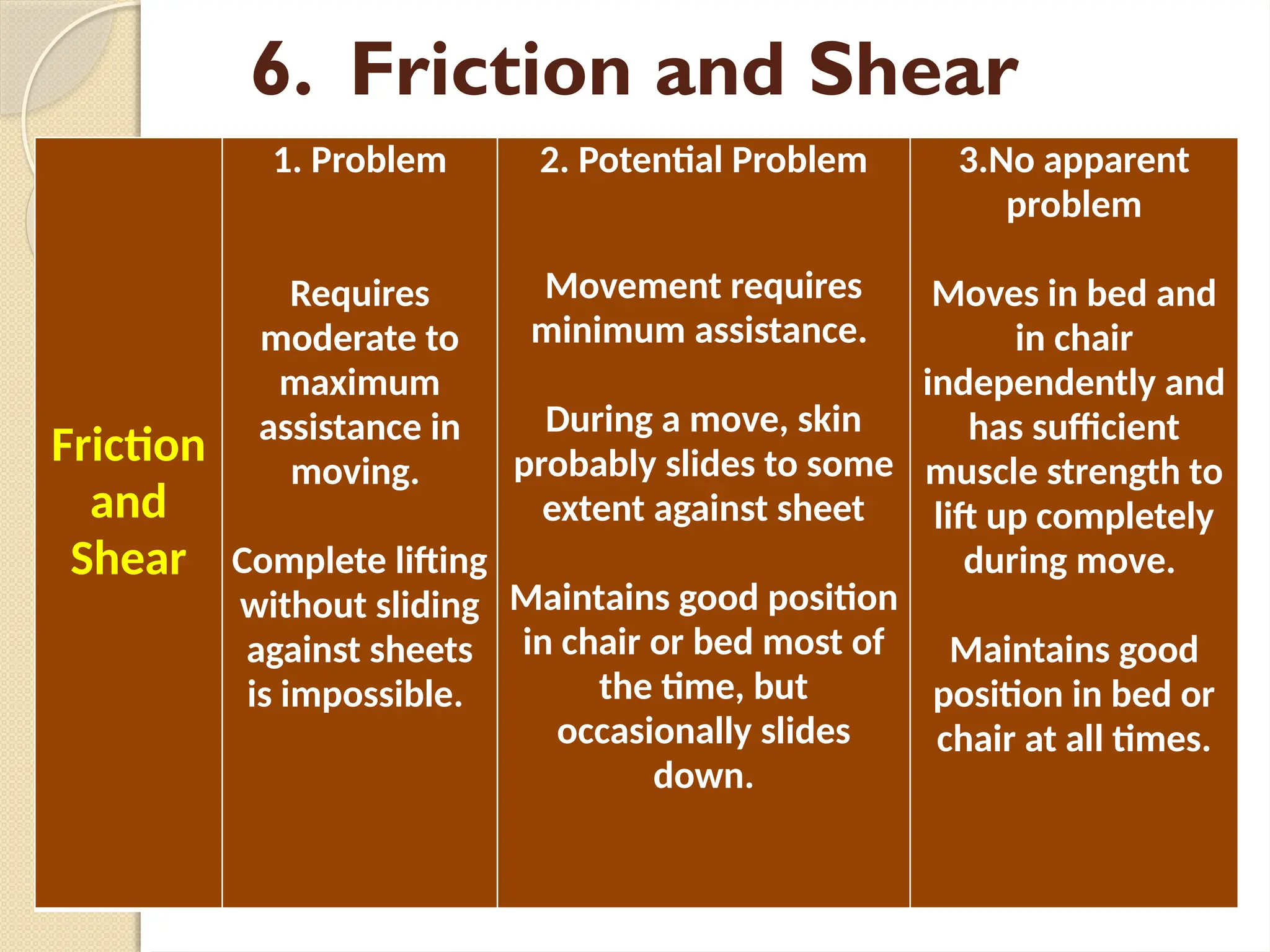
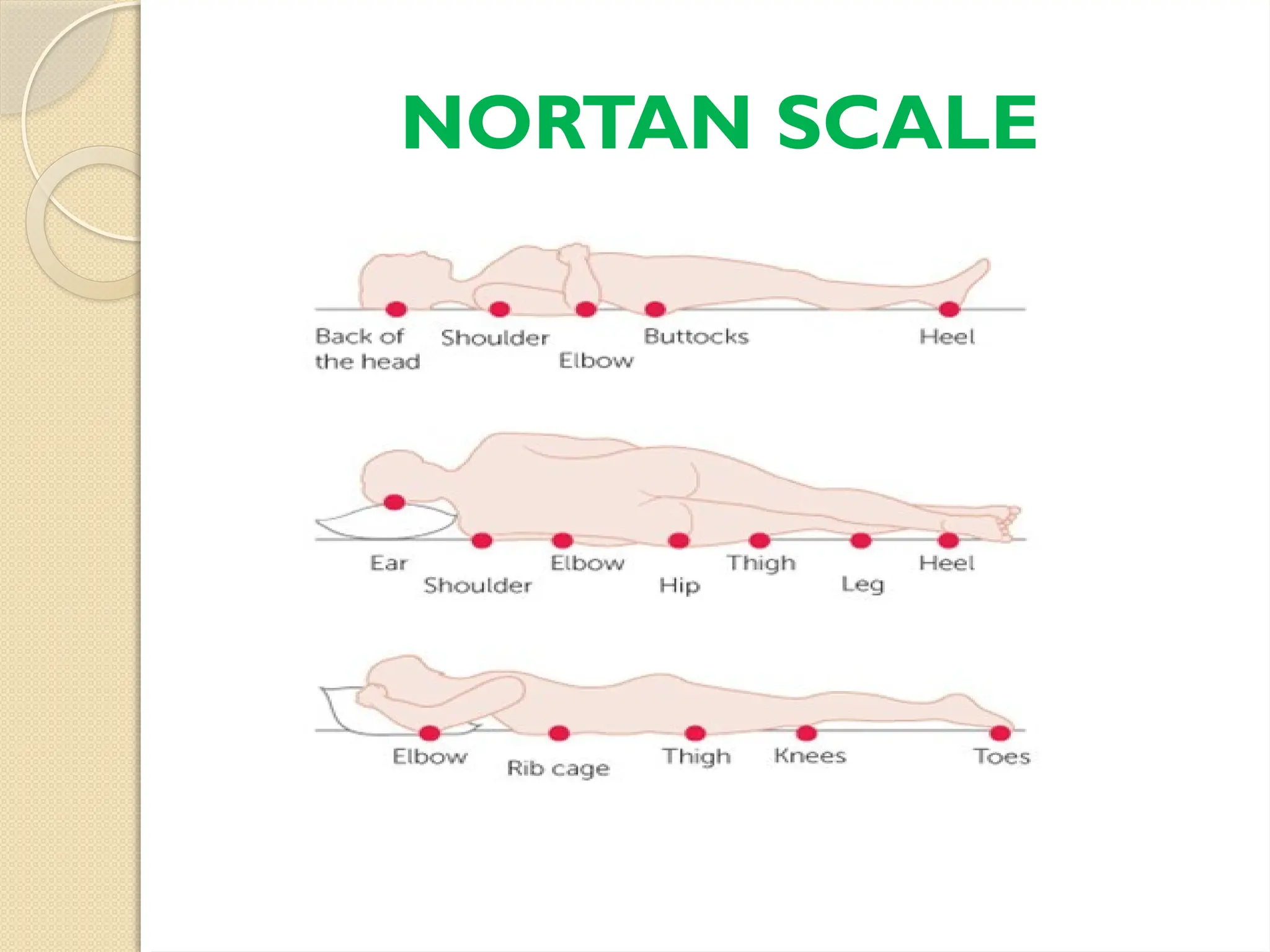
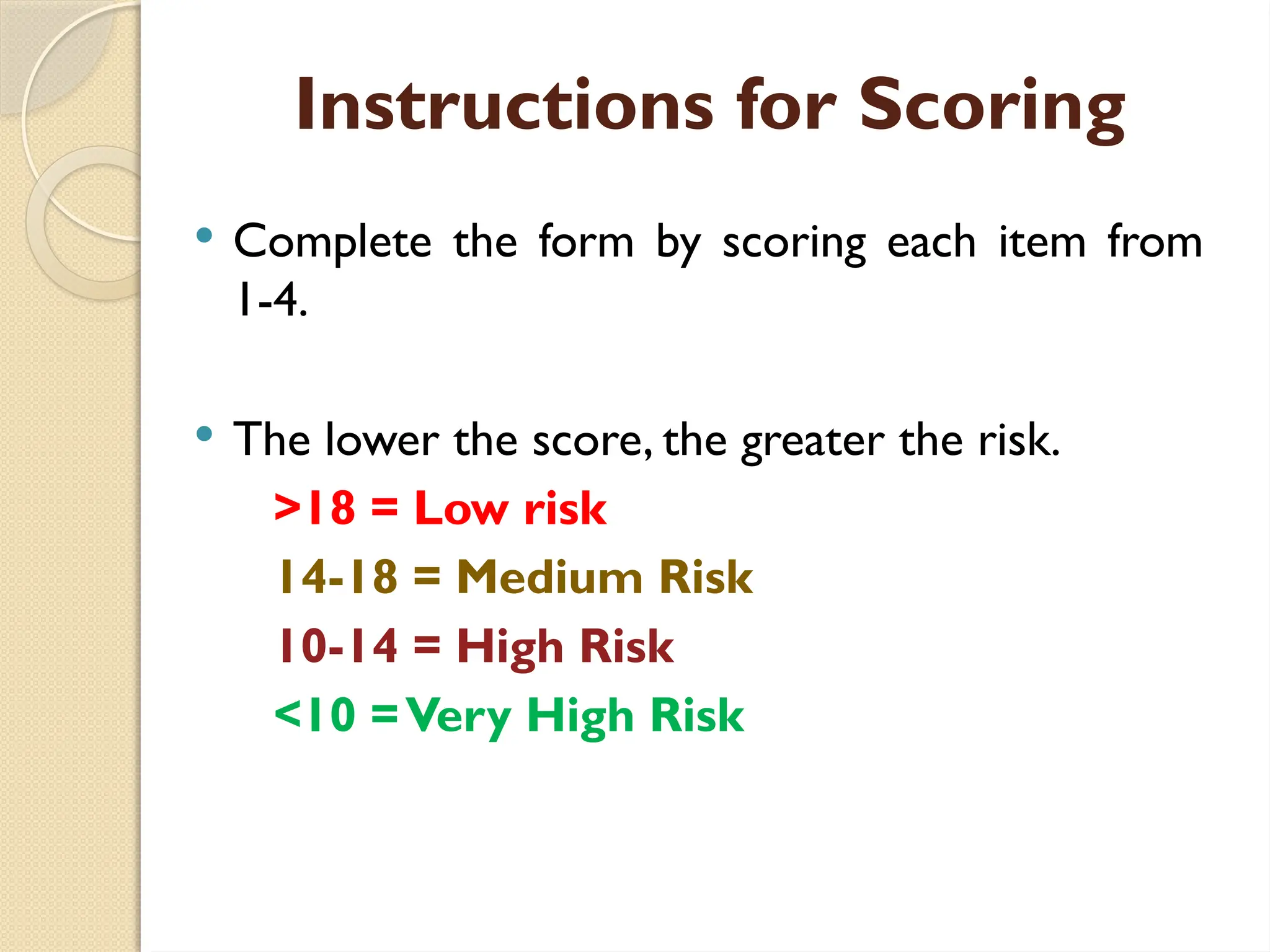
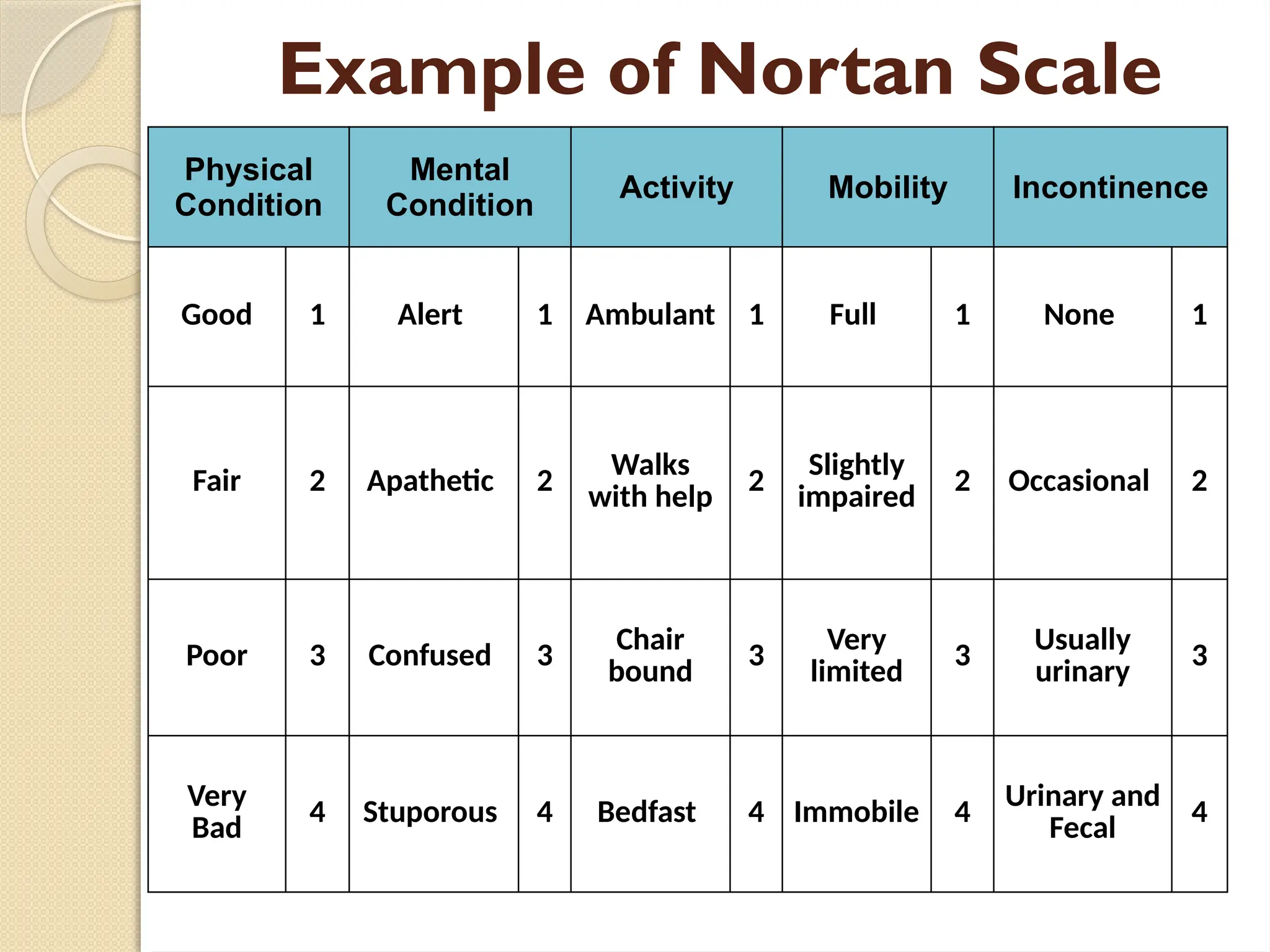
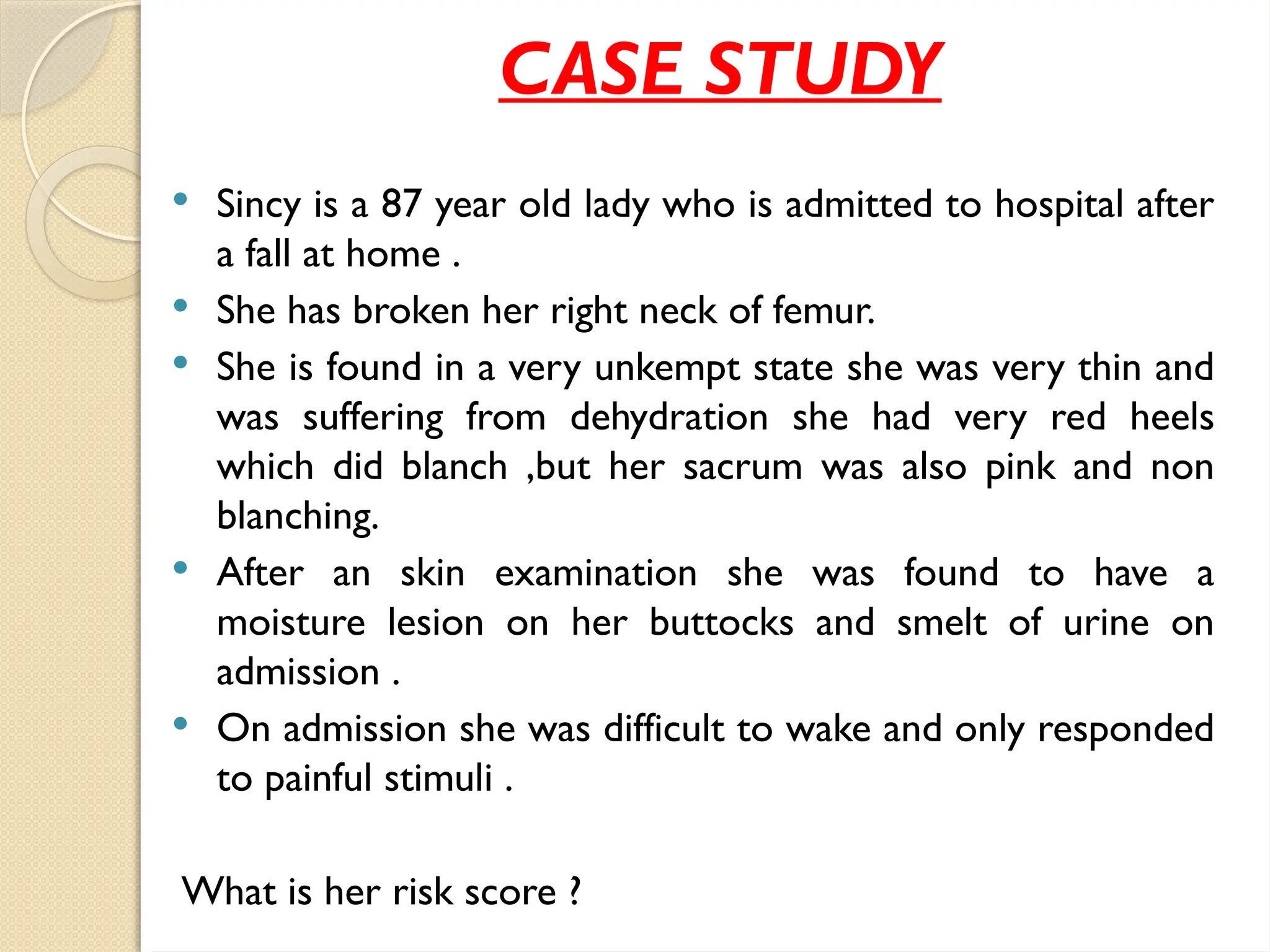
The Braden and Norton scales are tools developed to assess the risk of pressure ulcer development, with scores indicating varying levels of risk. The Braden scale has six factors with scores from 6-23, while the Norton scale evaluates five factors with scores from 5-20, both using lower scores to denote higher risk. A case study of an 87-year-old patient highlights the application of these scales, revealing significant concerns regarding her health and risk of pressure ulcers.