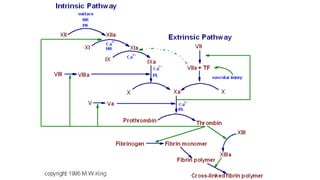
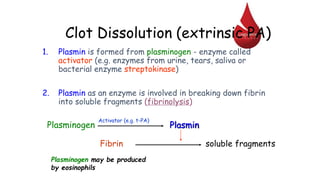
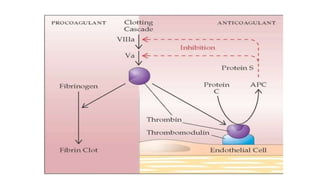
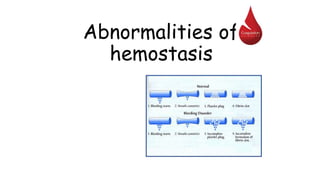
Hemostasis is the process of stopping bleeding when blood vessels are damaged. It involves three main steps: 1) local vasoconstriction of the damaged blood vessels, 2) formation of a temporary platelet plug at the site of injury, and 3) development of a blood clot via the clotting cascade. Precise regulation of hemostasis is vital, as both excessive and inadequate clotting can lead to harmful bleeding disorders. The document discusses the mechanisms of hemostasis and various bleeding and clotting abnormalities that can occur when this complex system is disrupted.