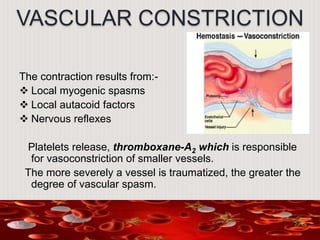
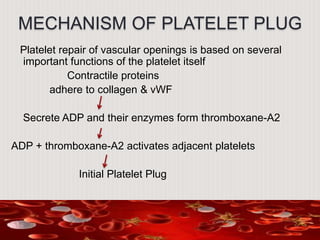
Hemostasis is the process by which bleeding is stopped. It occurs via mechanical, chemical, and thermal means. Mechanical hemostasis involves direct pressure, gauze packing, and suturing or ligating cut blood vessels. Chemical hemostasis occurs via platelet plug formation and blood coagulation, while thermal hemostasis involves vasoconstriction to reduce blood flow to the site of injury. Together, these processes form a clot to seal the damaged vessel until tissue repair can take place.

![.
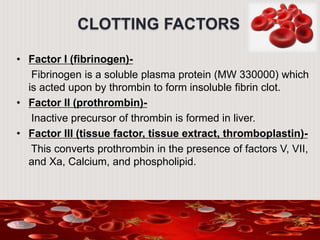
Factor IV (calcium)-
Factor V (labile factor, thrombogene or proaccelerin)-
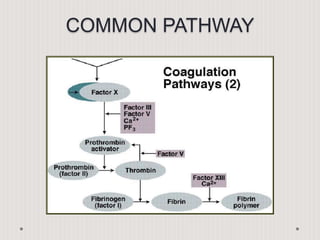
This factor is reqd. for the conversion of prothrombin to
thrombin by tissue extract and plasma factors.
Factor VII (stable factor, autoprothrombin I)-
Factor VII is reqd. for the formation of prothrombin activator
by tissue extract.
Factor VIII (antihemophilic globulin [AHG],
antihemophilic factor)-
Factor VIII is reqd. for the formation of prothrombin activator
from blood constituents; it’s consumed during clotting and
hence
absent from serum. In vivo the half life of factor VIII is 10-20h.](https://image.slidesharecdn.com/jkok-150829082436-lva1-app6891/85/Hemostasis-27-320.jpg)