Embed presentation
Downloaded 89 times
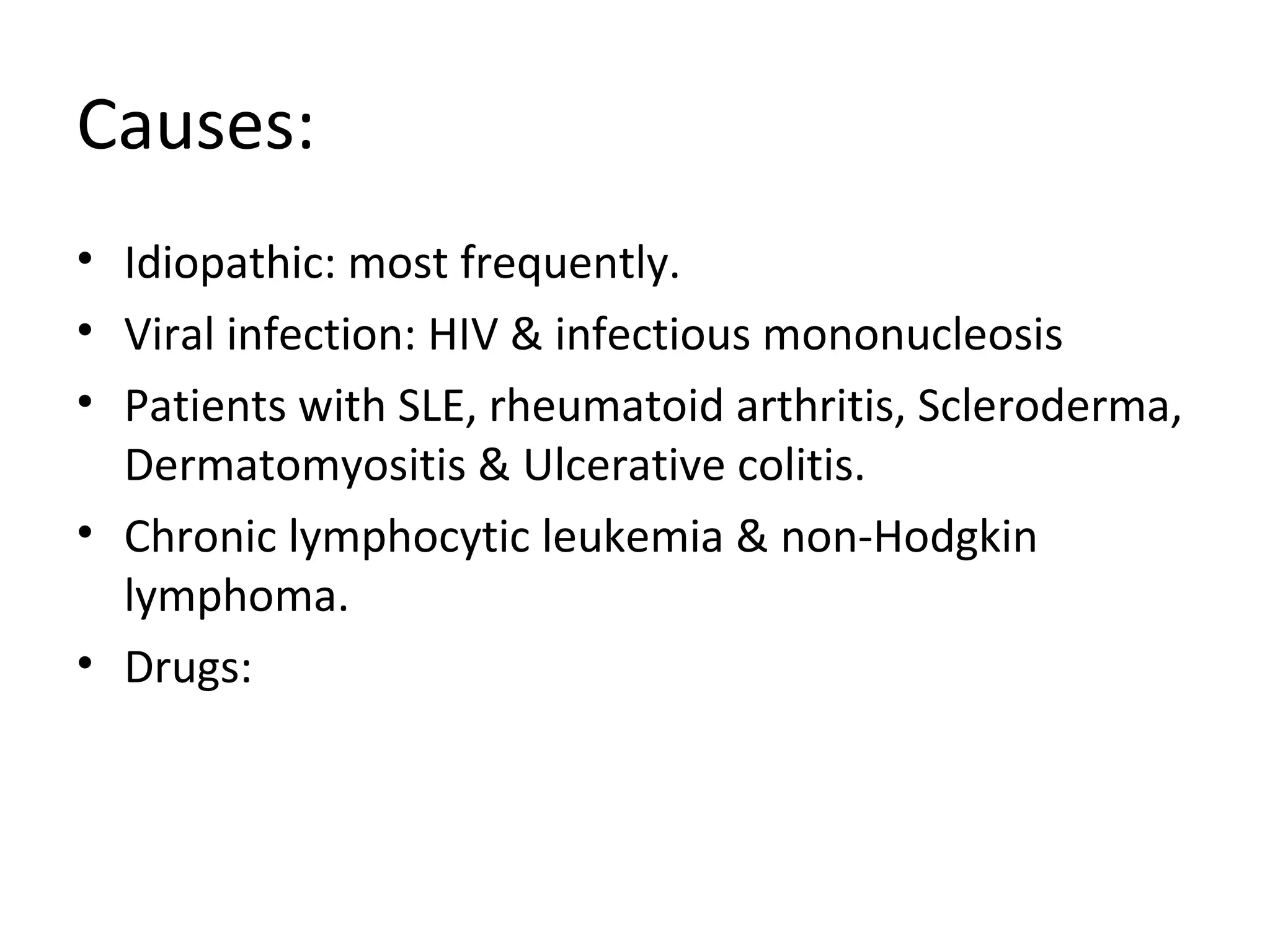
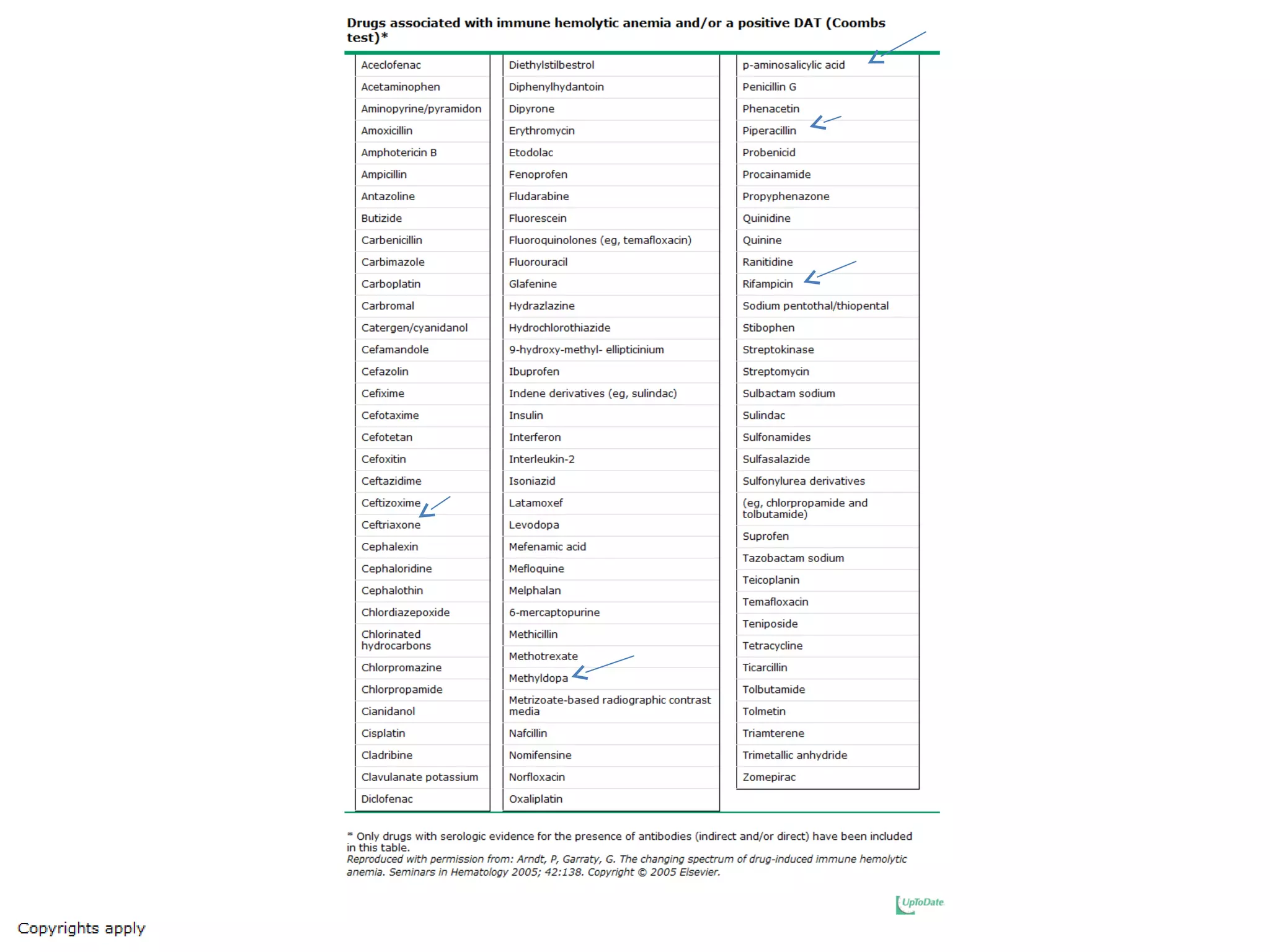
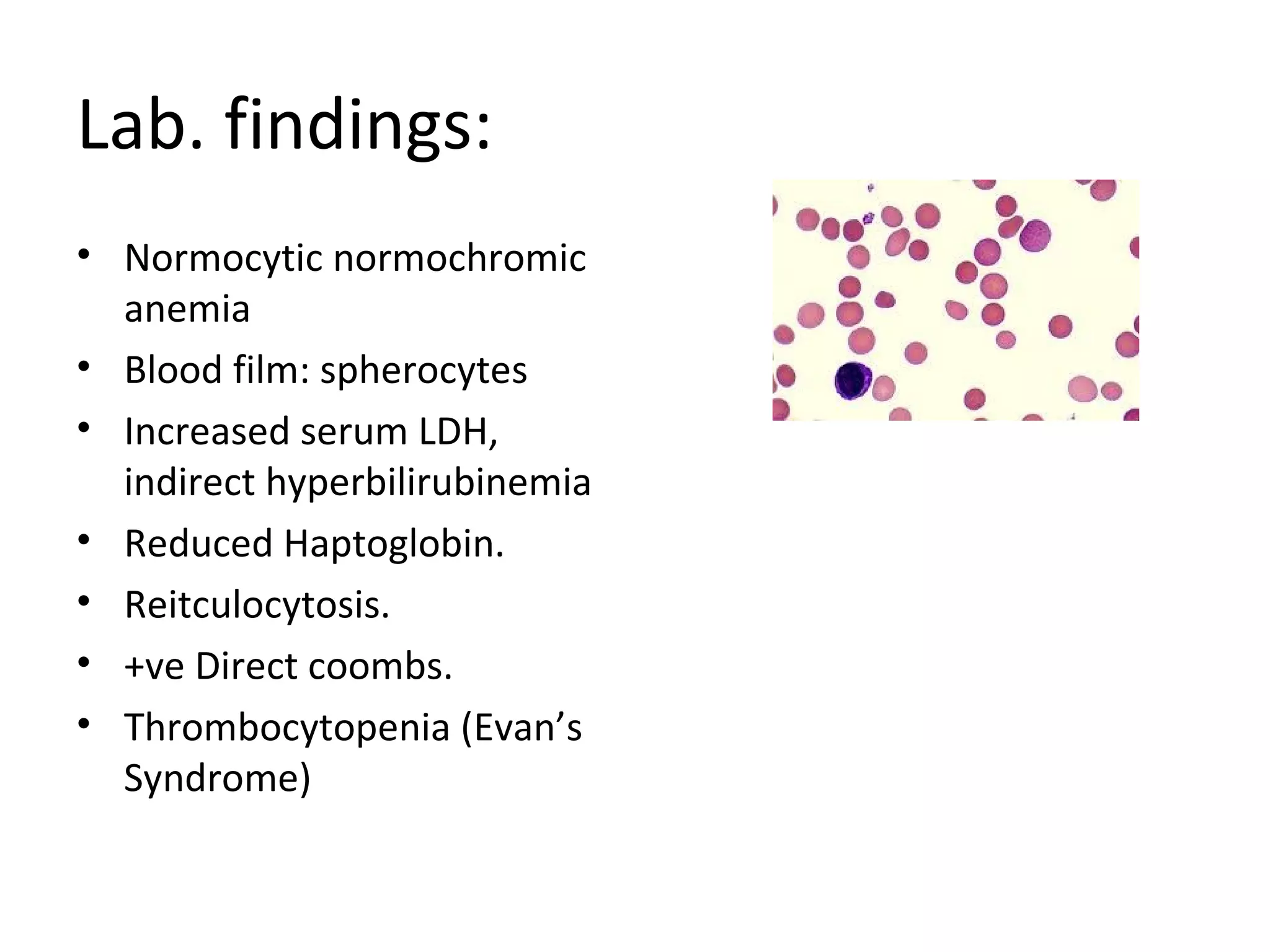
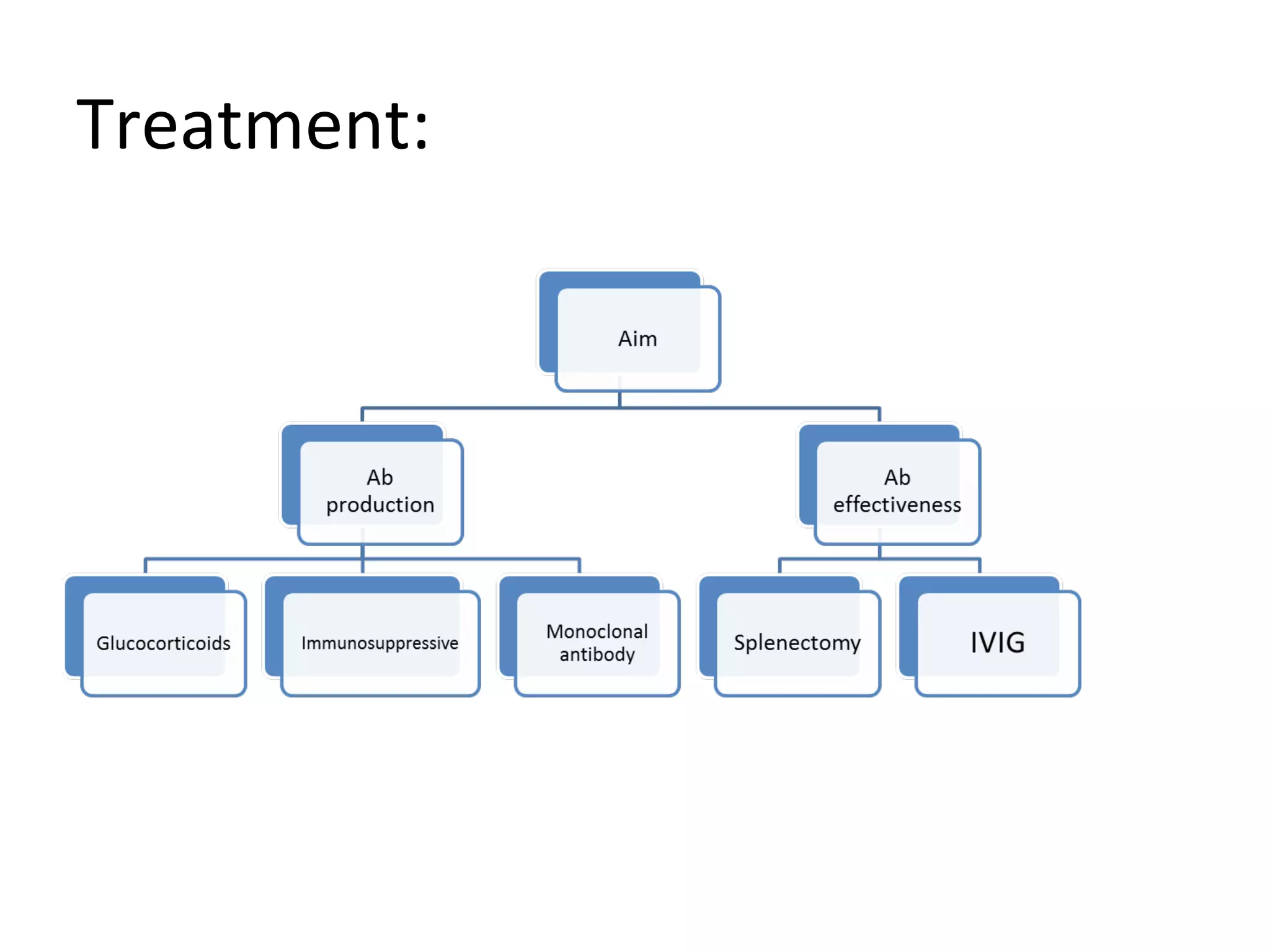
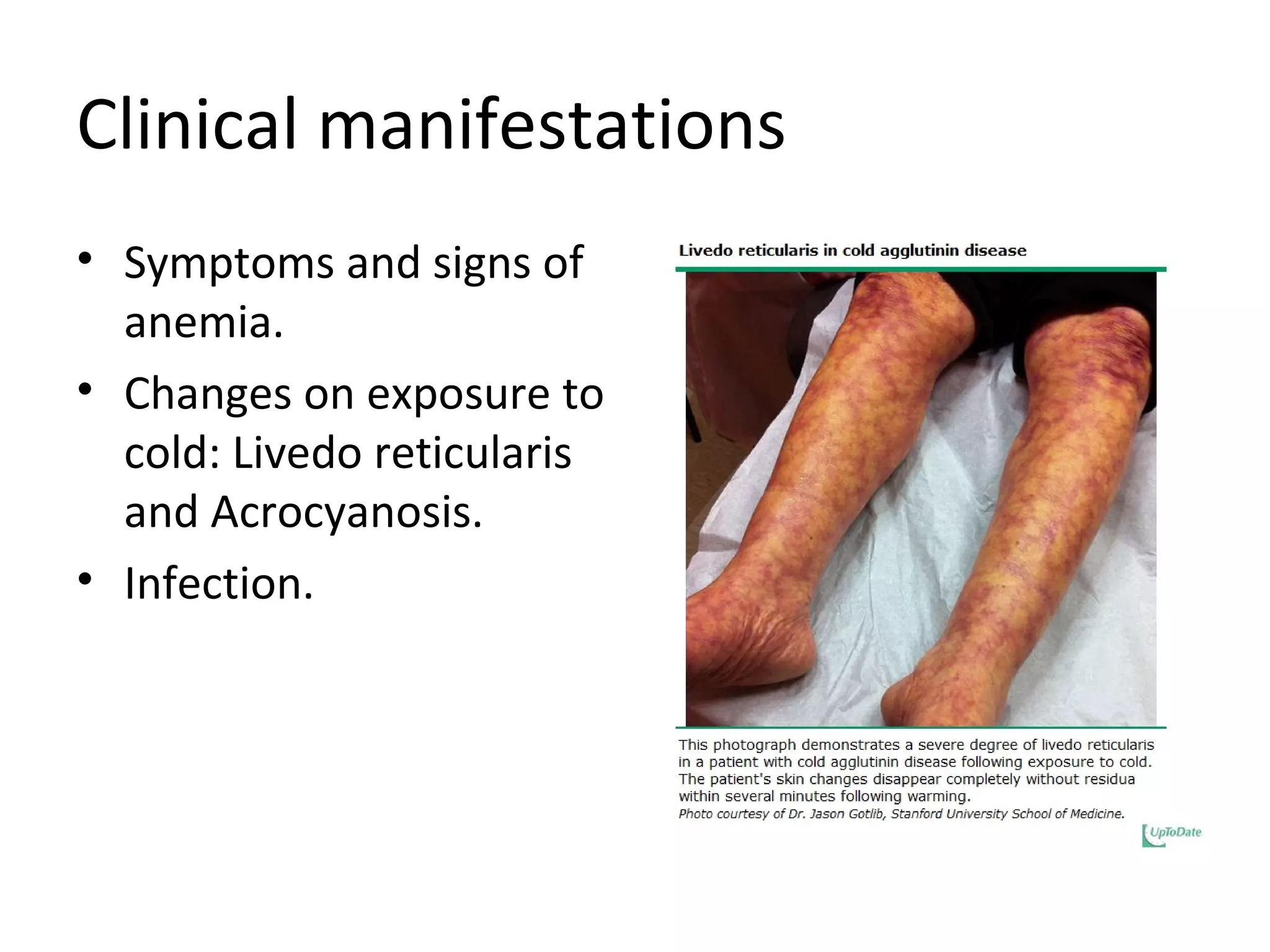

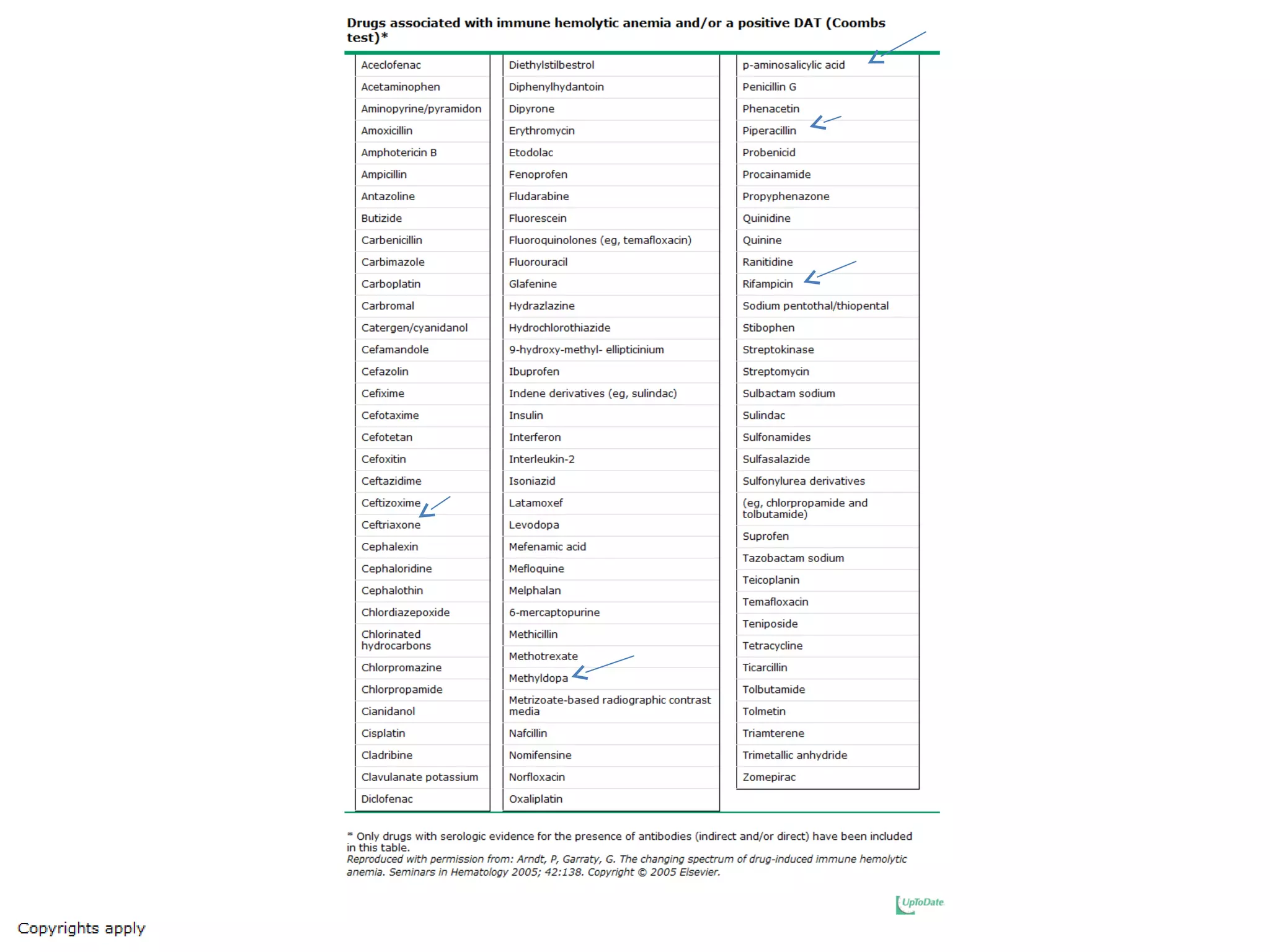
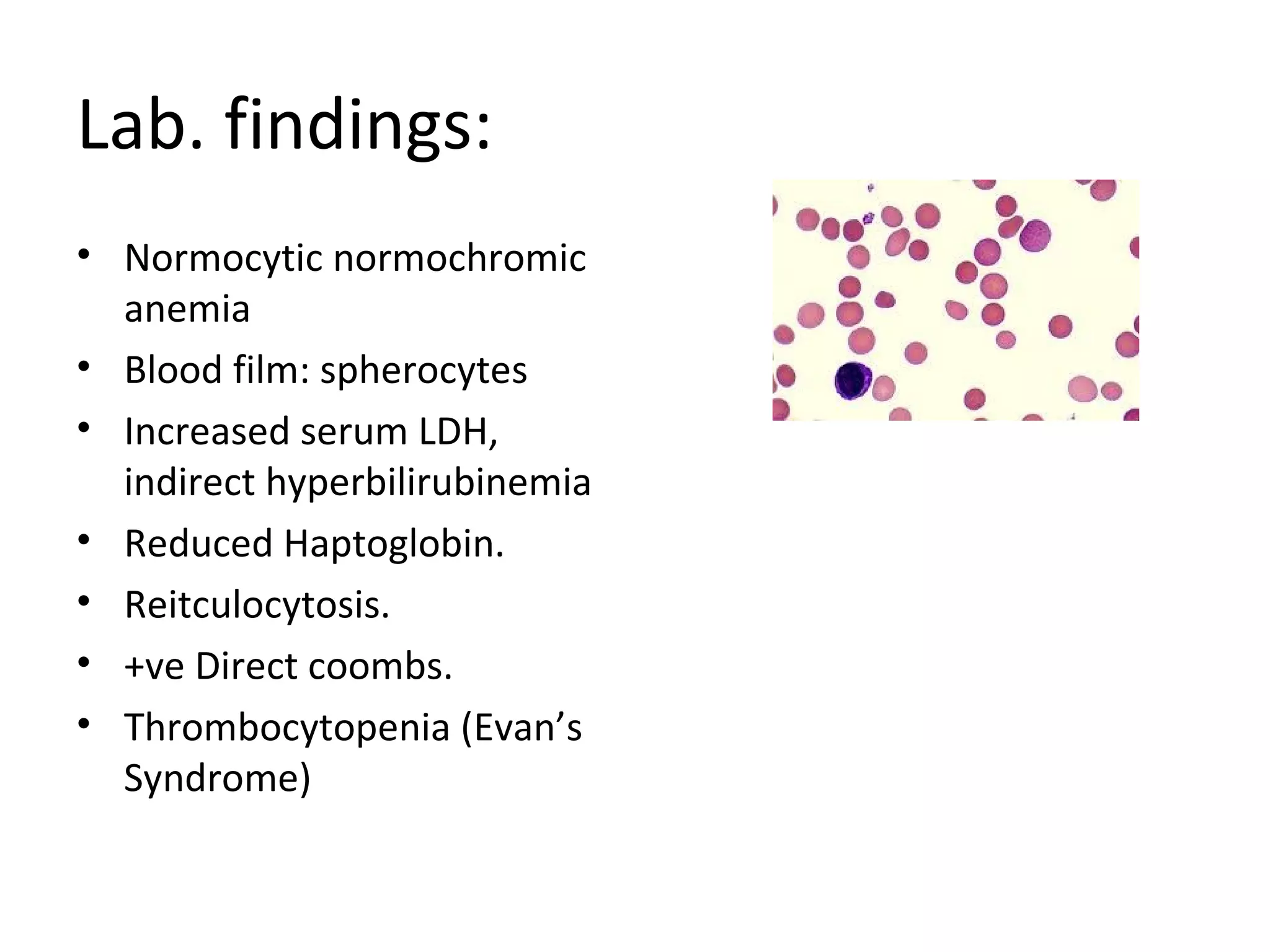
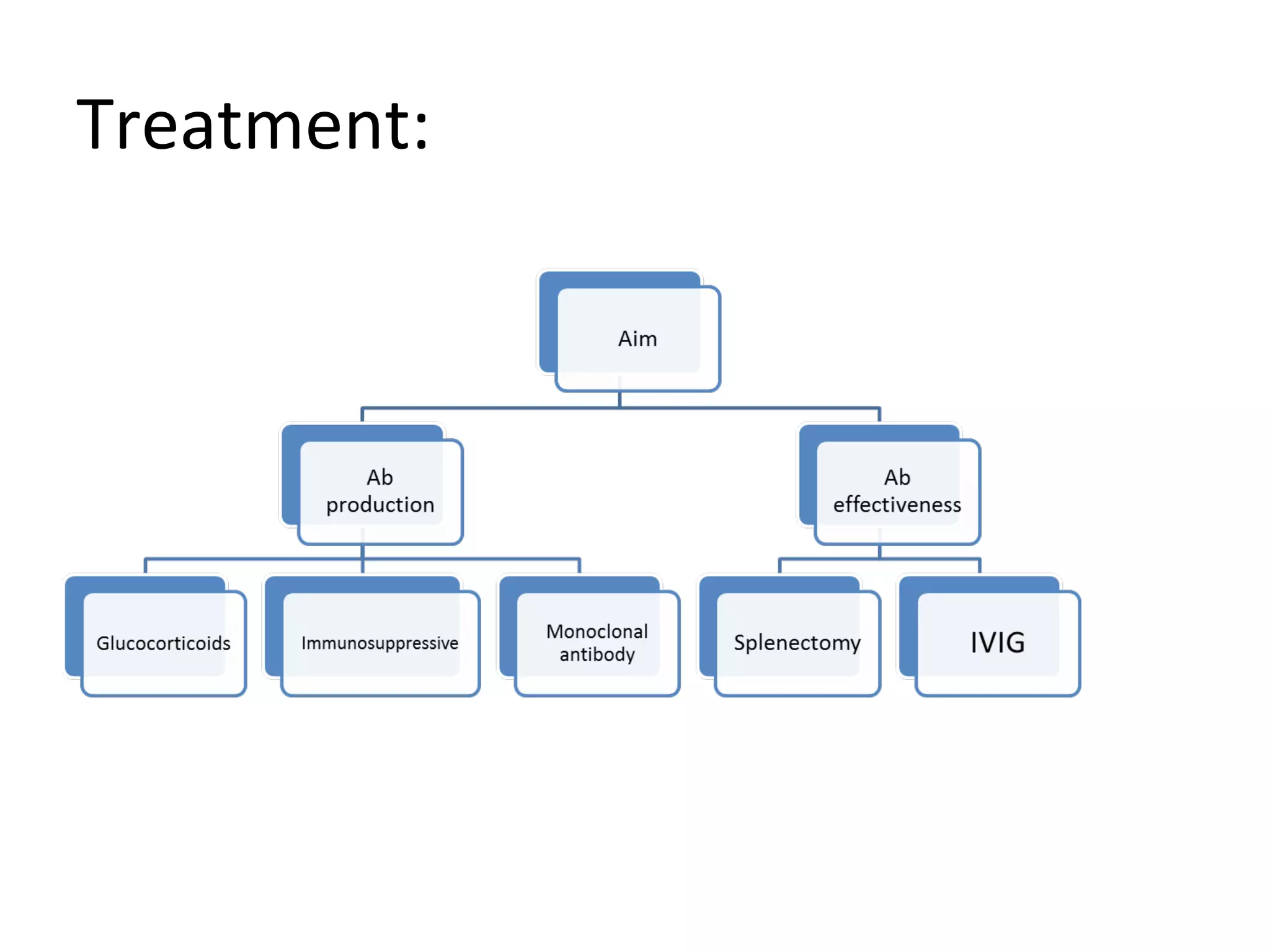
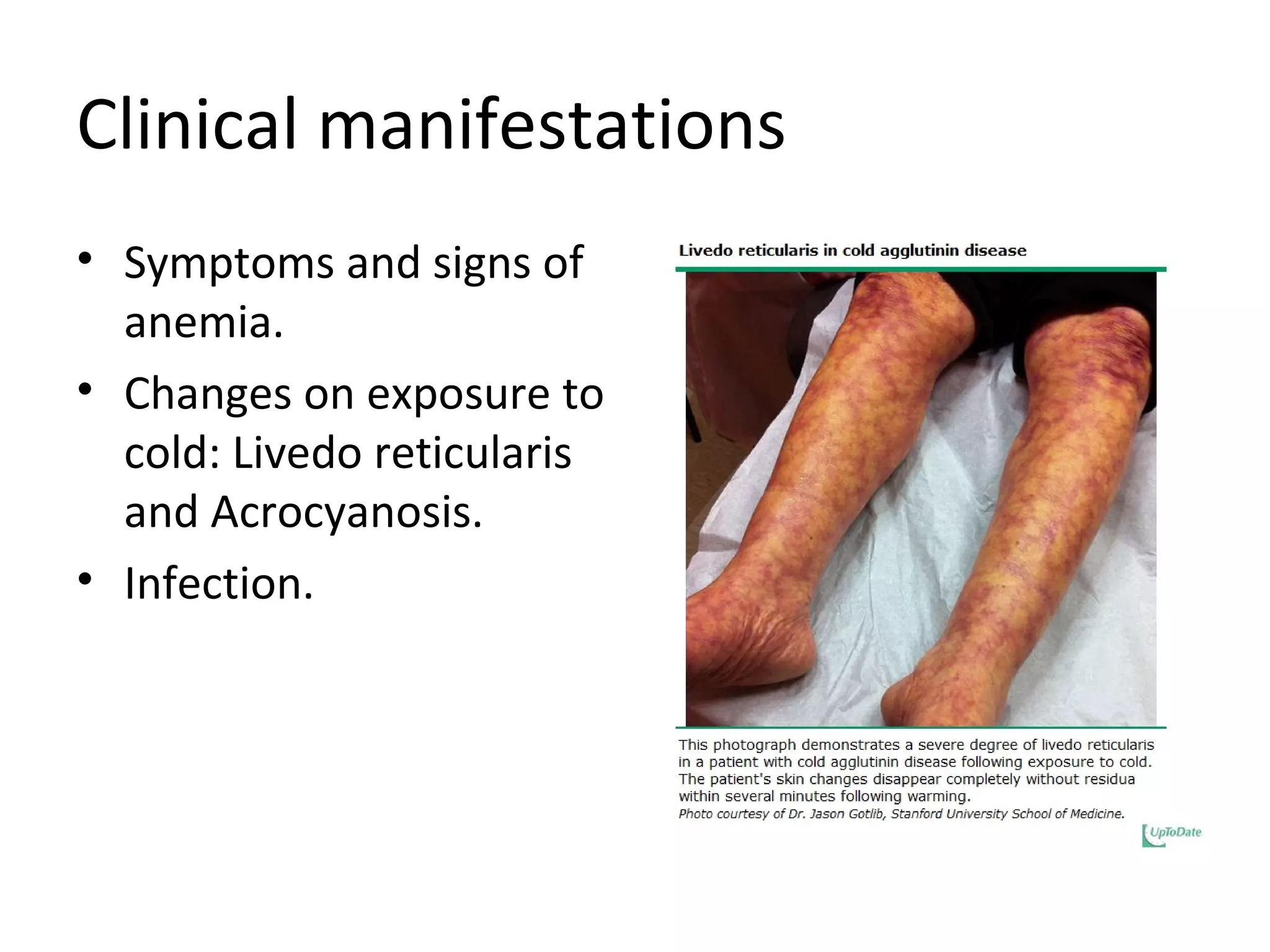
Autoimmune hemolytic anemia is one of the most common causes of acquired hemolytic anemia and can be caused by two types of antibodies - IgG or IgM. There are two main types: warm autoimmune hemolytic anemia, which has various potential causes like infection or underlying conditions, and cold autoimmune hemolytic anemia caused by IgM antibodies against red blood cells leading to symptoms on cold exposure. Both types result in anemia and can be diagnosed through laboratory tests showing signs of hemolysis and the presence of antibodies, and treatments aim to avoid triggers and suppress the immune system response.