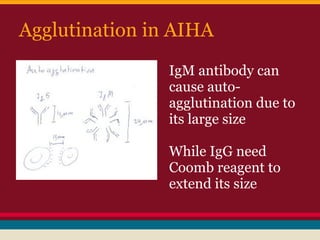
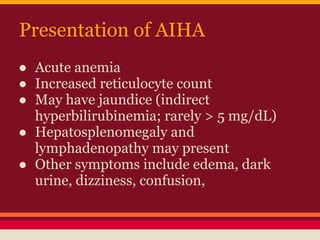
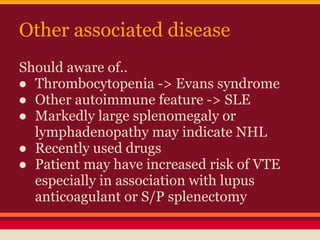
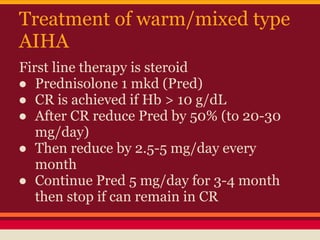
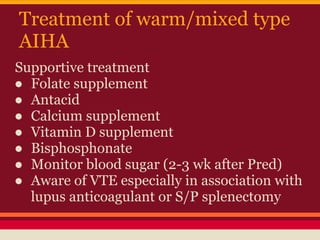
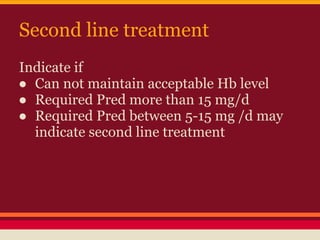
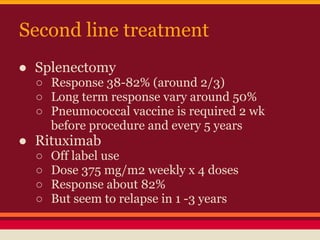
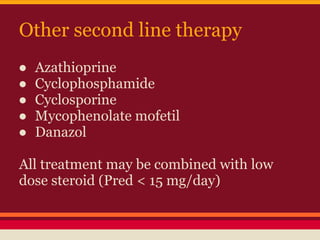
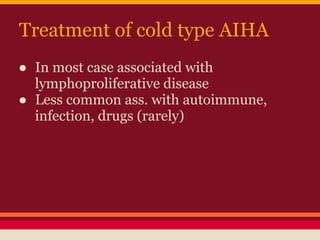
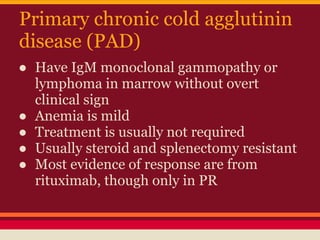
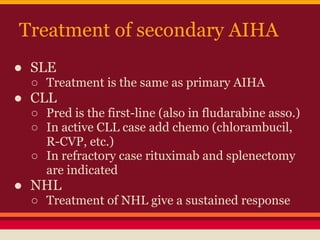
Autoimmune hemolytic anemia (AIHA) can be primary or secondary. Primary AIHA has no obvious cause, while secondary is precipitated by conditions like drugs, infections, or tumors. AIHA is caused by autoantibodies binding to red blood cells (RBCs), which are then destroyed in the spleen or liver. Warm antibody AIHA is treated mainly with steroids, while cold antibody types are more resistant and associated with lymphoproliferative diseases. Treatment depends on the type and severity of AIHA.