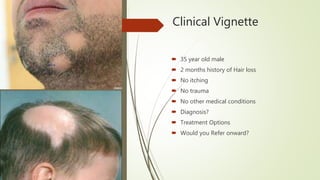
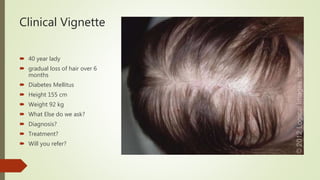
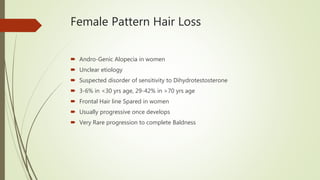
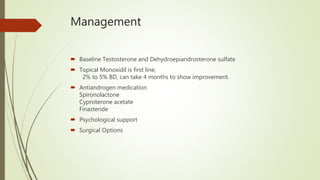
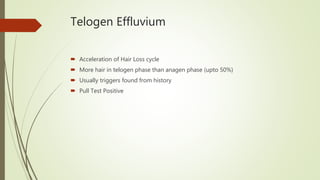
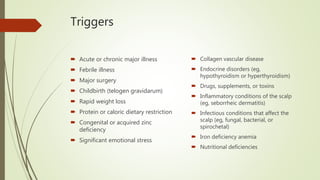
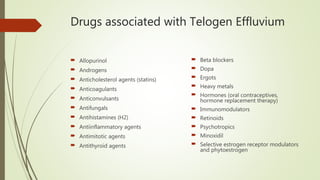
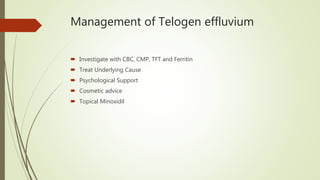
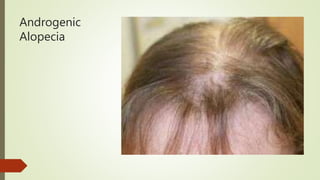
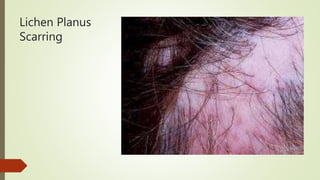
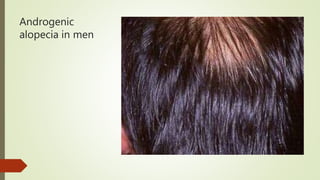
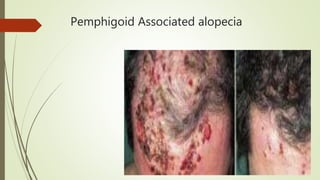
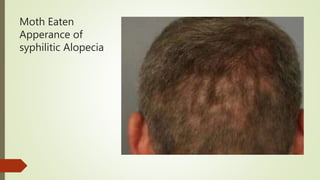
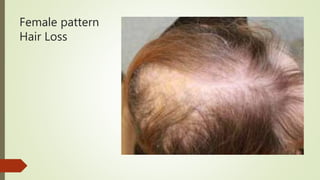
The document outlines common hair disorders, their management in primary health care, and referral criteria, emphasizing educational intent and evidence-based recommendations. It covers various conditions like alopecia areata, androgenic alopecia, and telogen effluvium, detailing their symptoms, assessments, and treatment options. Clinical cases illustrate diagnostic considerations and management strategies for hair loss disorders.