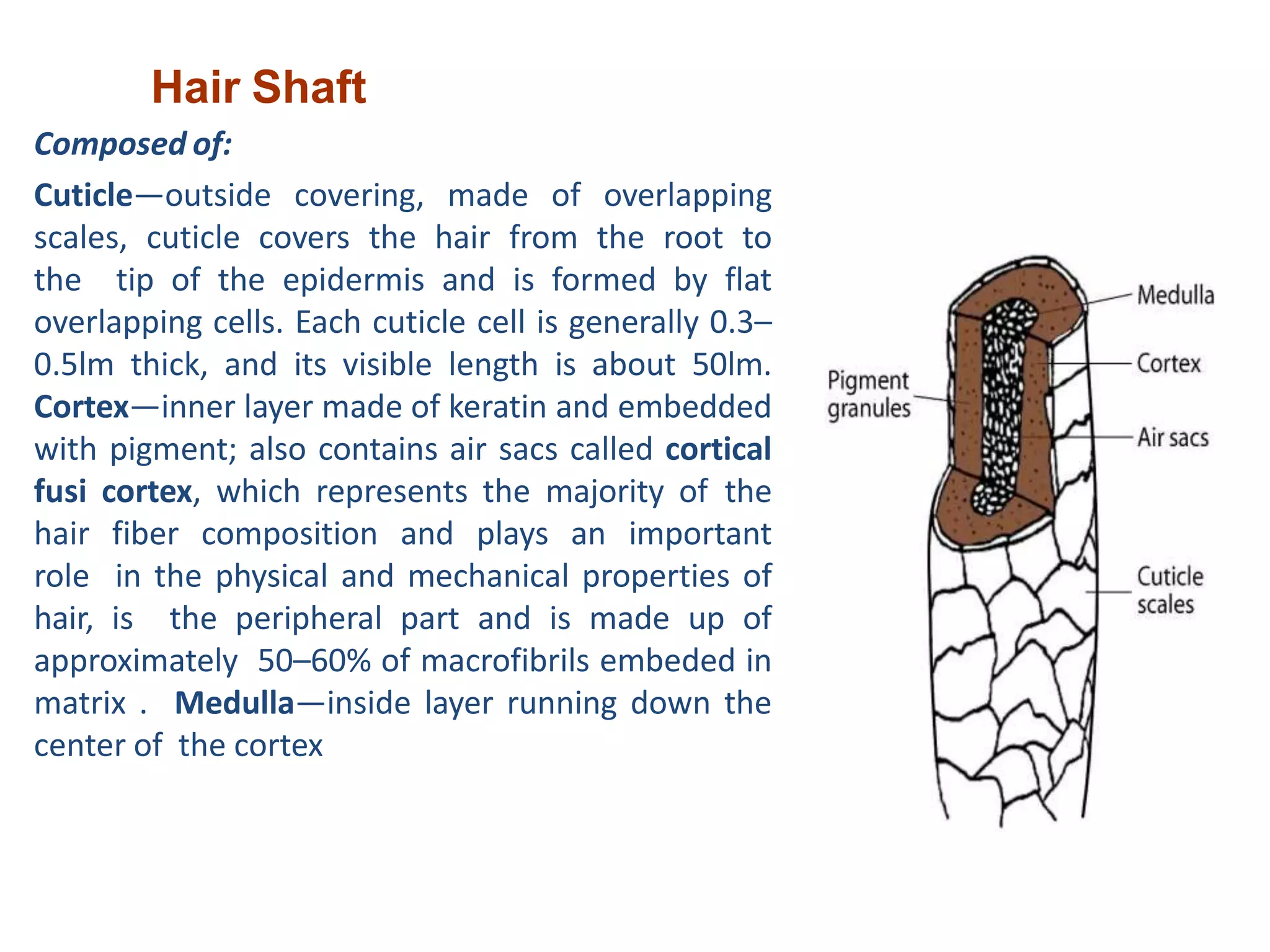
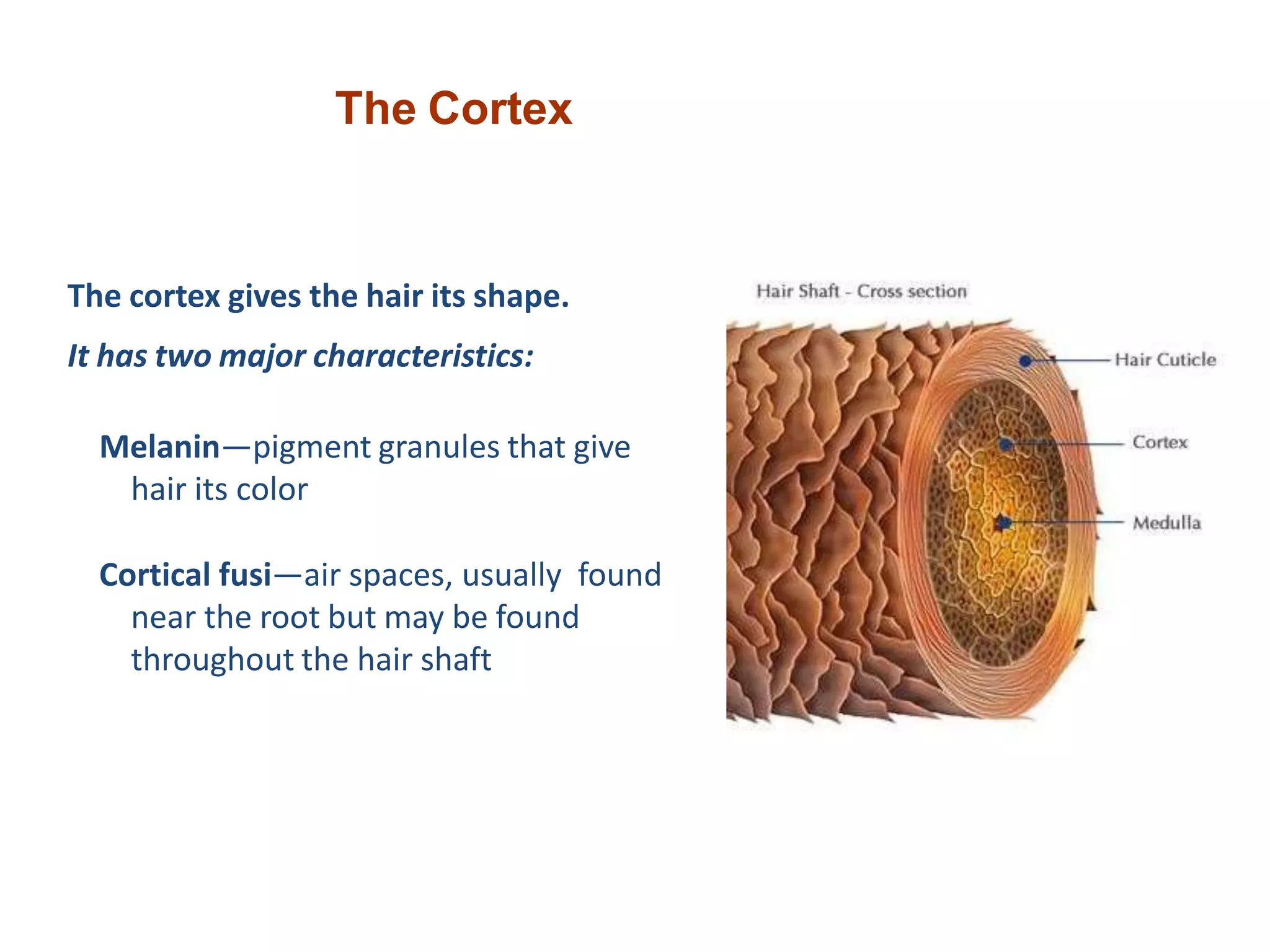
The document discusses hair disorders and provides details about hair structure and the hair growth cycle. Some key points:
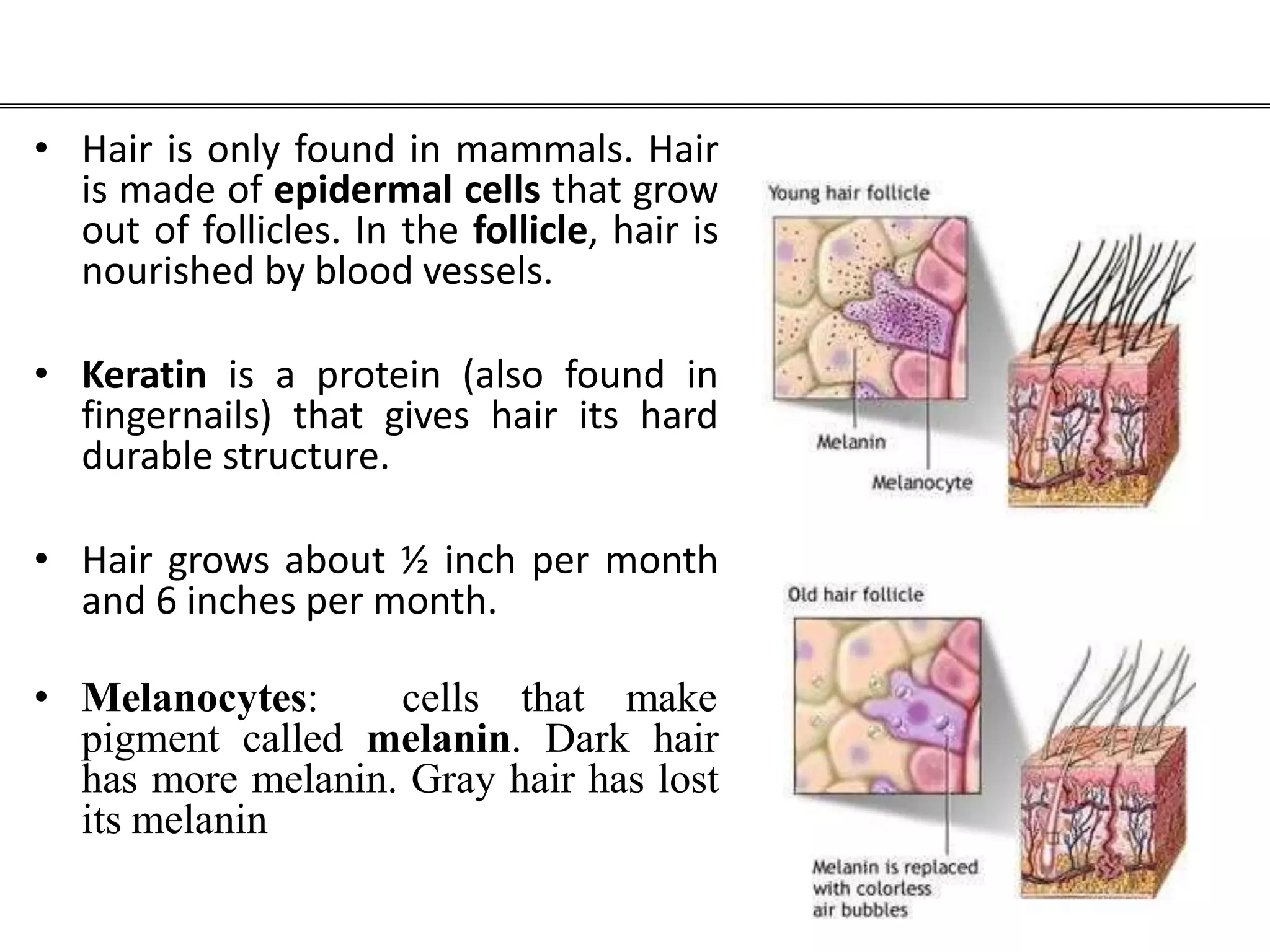
- Hair is found in mammals and grows from follicles, providing protection and regulating temperature. It grows about half an inch per month.
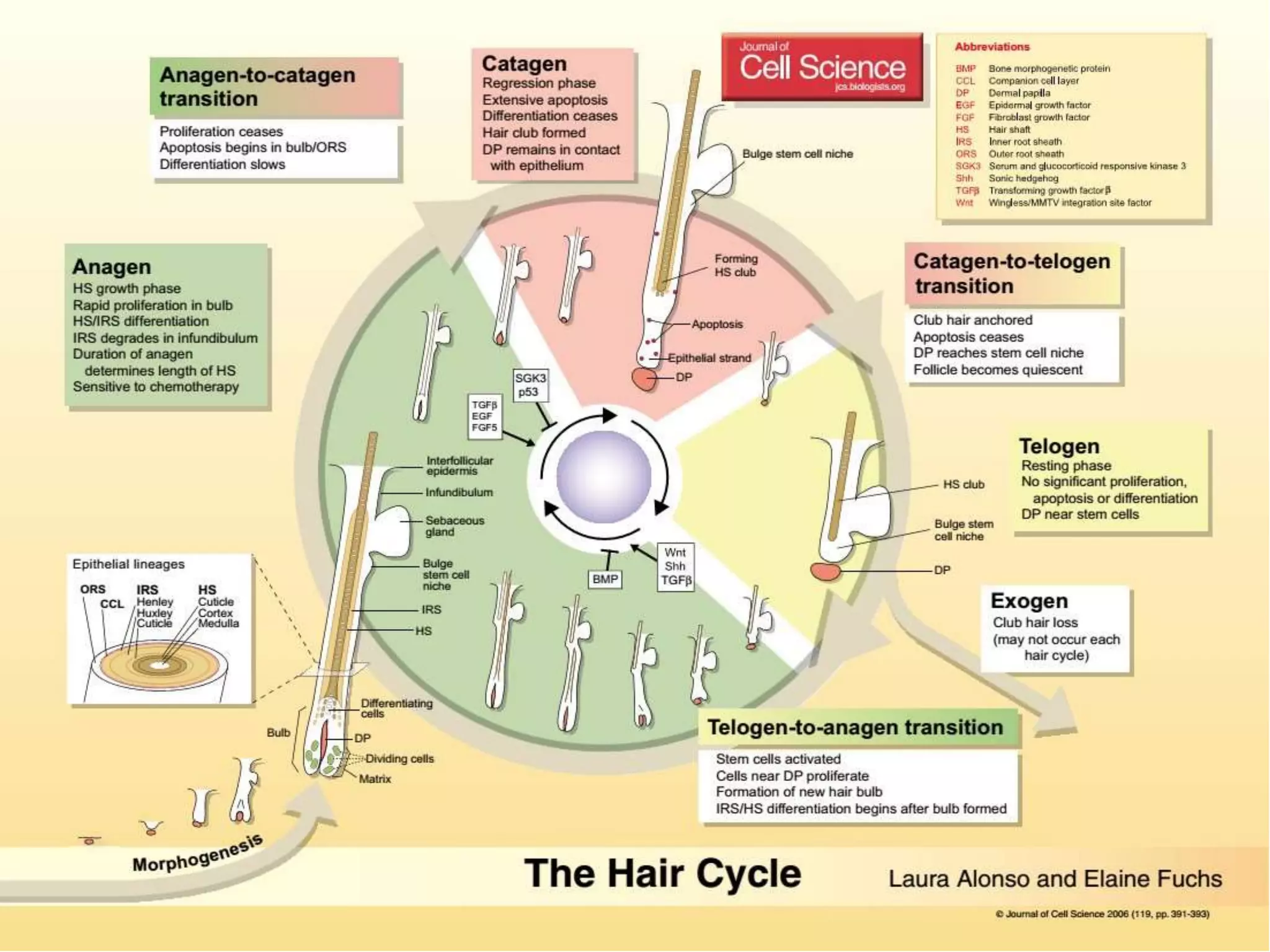
- The hair growth cycle consists of anagen (growth phase), catagen (transition phase), and telogen (resting phase). Hair disorders can disrupt this cycle.
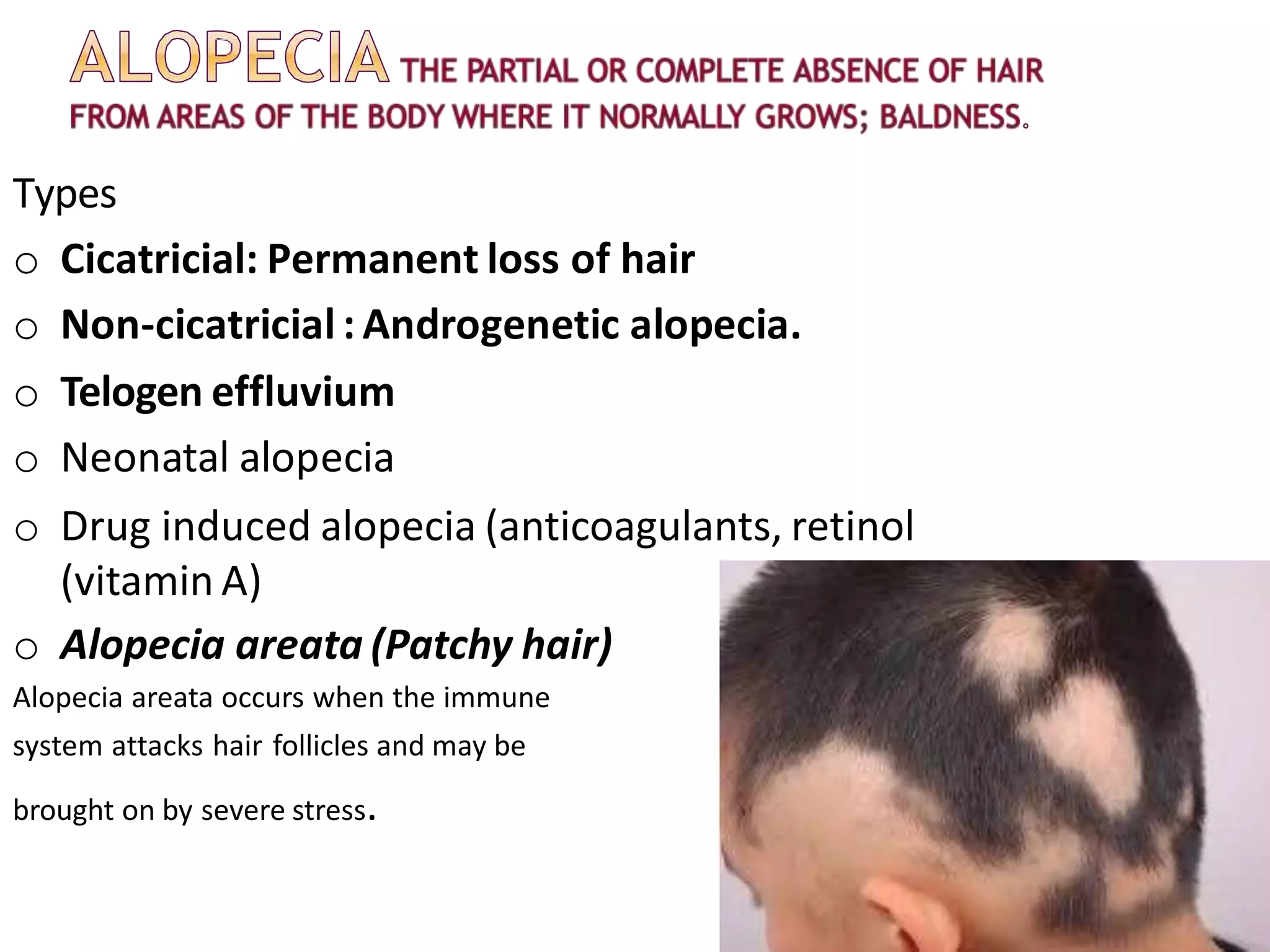
- Common hair disorders include dandruff, seborrheic dermatitis, alopecia (hair loss), hirsutism (excess hair growth), and hair shaft abnormalities. Treatment depends on the specific disorder.