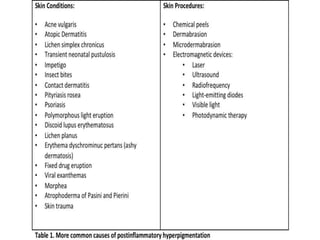
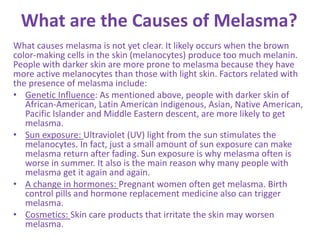
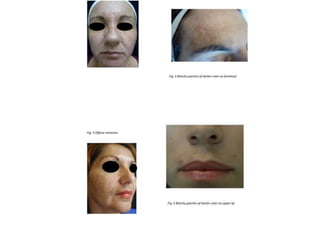
The document explains hyperpigmentation, a condition where excessive melanin darkens the skin, which can take two forms: diffuse and circumscribed, often caused by inflammation or certain conditions like melasma. Treatment includes addressing underlying causes, using photoprotection, topical agents like hydroquinone, and cosmetic procedures, while recognizing that melasma, particularly in women and those with darker skin, can also be significantly influenced by sun exposure and hormonal changes. Both conditions can lead to emotional distress, affecting individuals' self-esteem and quality of life.