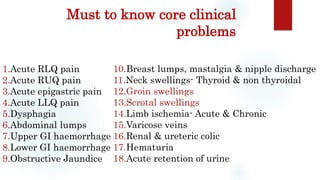
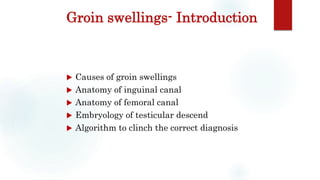
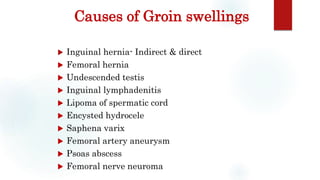
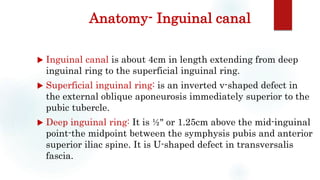
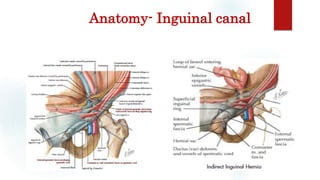
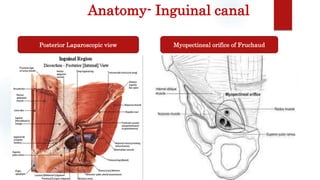
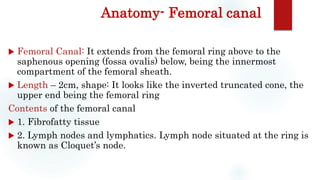
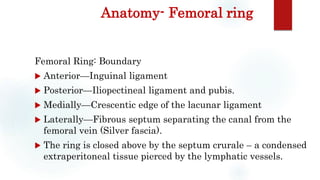
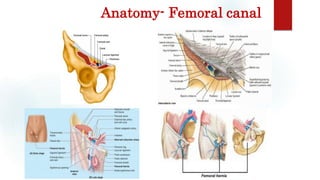
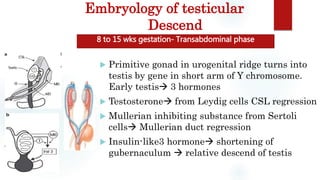
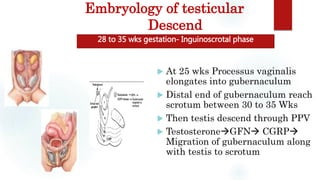
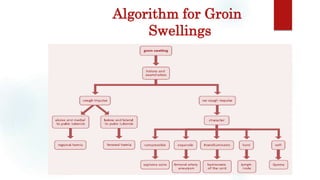
This document, authored by Dr. B. Selvaraj, discusses groin swellings and their clinical significance, detailing various causes and anatomical considerations such as the inguinal and femoral canals. It also covers embryology regarding testicular descent and provides an algorithm for diagnosing groin swellings. The text serves as a comprehensive overview for medical practitioners focusing on surgical issues related to groin swellings.