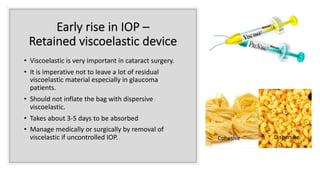
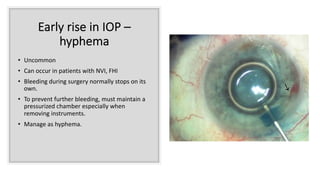
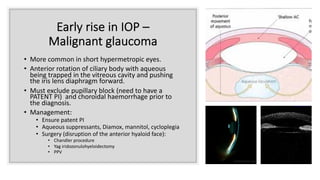
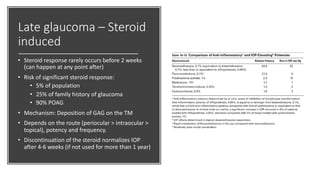
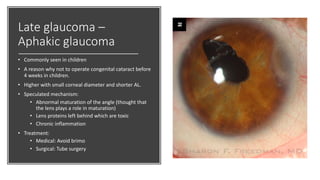
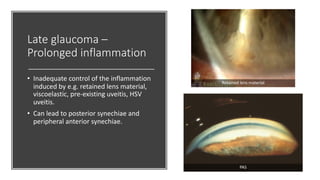
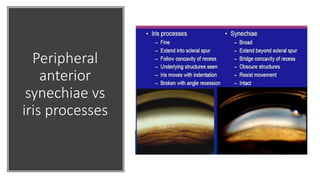
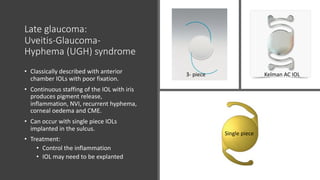
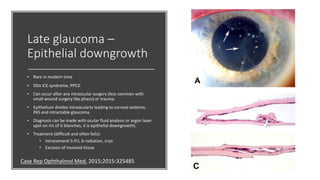
Glaucoma can develop after cataract surgery due to various mechanisms. Early causes within the first few days include retained viscoelastic material, inflammation, hyphema, pupillary block, and malignant glaucoma. Late causes after 2 weeks can be steroid-induced glaucoma, changes to the trabecular meshwork from aphakia, peripheral anterior synechiae, epithelial ingrowth, retained lens matter, or uveitis-glaucoma-hyphema syndrome from intraocular lens complications. Managing the underlying cause through medical or surgical treatment is important to control post-operative glaucoma.