This document discusses deep anterior lamellar keratoplasty (DALK), a type of corneal transplant surgery. It provides:
1) A brief history of DALK, beginning with early successful transplants in the late 19th century and developments in techniques in the 1950s and 1980s.
2) Indications for DALK including keratoconus, post-LASIK ectasia, hereditary stromal dystrophies, infectious keratitis, and tectonic indications.
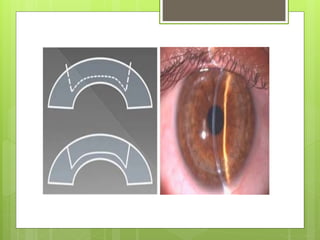
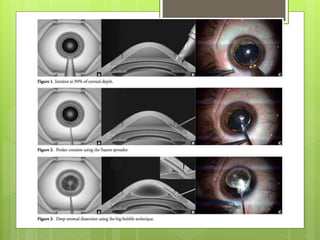
3) An overview of various surgical techniques for DALK including manual dissection, air-assisted dissection, and techniques using viscoelastic or femtosecond lasers.
4) Preparation of