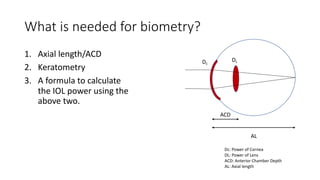
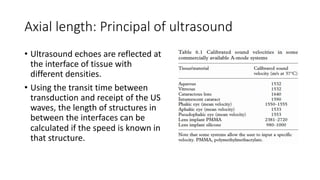
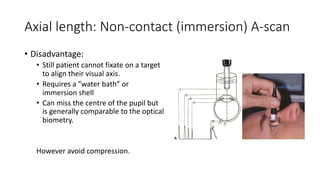
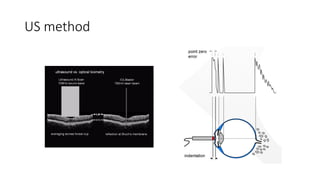
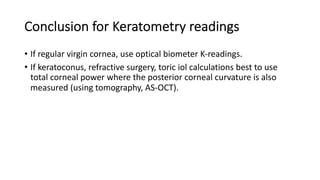
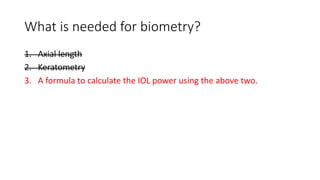
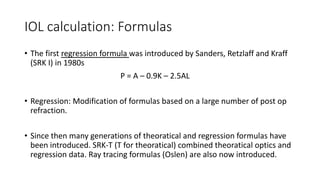
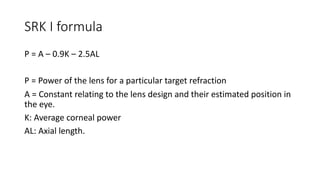
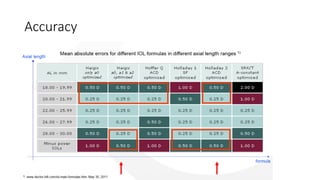
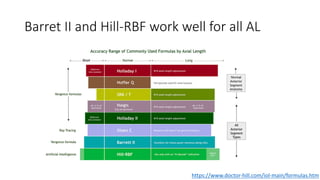
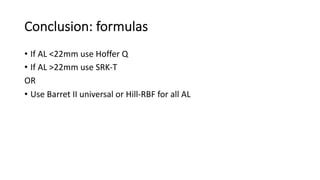
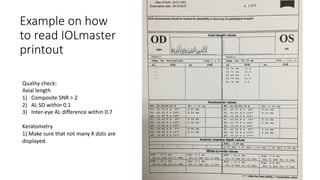
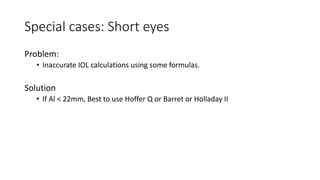
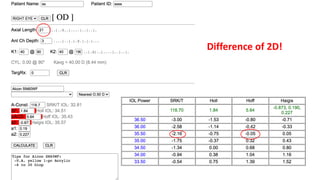
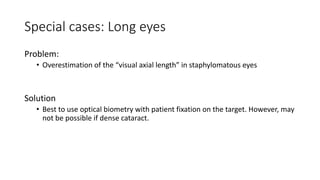
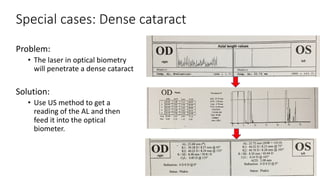
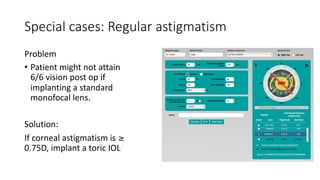
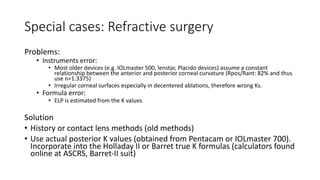
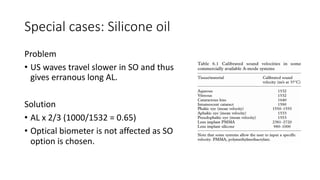
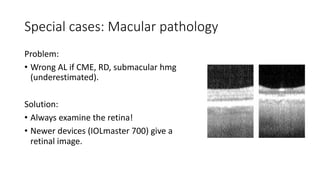
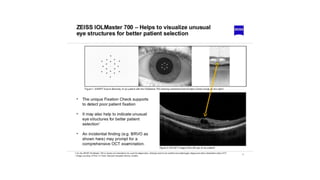
Biometry is used to measure the eye to determine the correct intraocular lens power for cataract surgery. It involves measuring the corneal power with keratometry and the eye length with axial length measurement. The optimal method is optical biometry which measures both simultaneously while allowing the patient to fixate, improving accuracy. Special cases like high myopia, prior refractive surgery, or pathology require adjusted measurement techniques or formulas to calculate the lens power accurately.