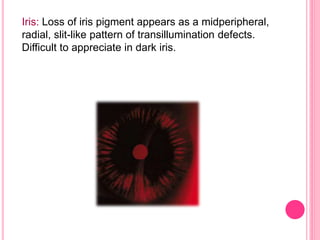
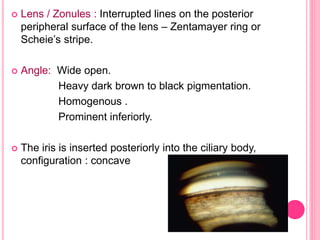
Pigment dispersion syndrome (PDS) and pigmentary glaucoma (PG) are two stages of the same disease caused by disruption of the iris pigment epithelium and deposition of pigment granules in the anterior segment. PDS typically affects young, myopic males and is characterized by blurry vision or eye pain after exercise. Over time, PDS can progress to PG as the deposited pigment increases resistance in the trabecular meshwork, elevating intraocular pressure. Treatment aims to reverse iris concavity, prevent further pigment release, and lower IOP using miotics, prostaglandin analogs, laser iridotomy, or surgery if needed to control pressure.