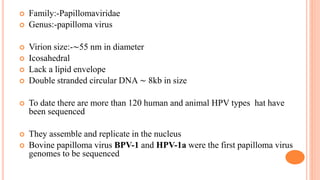
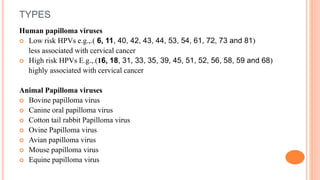
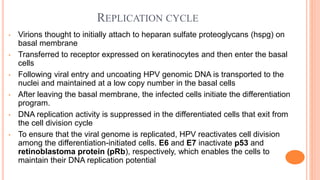
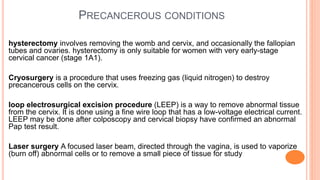
Human papillomavirus (HPV) is a double stranded DNA virus that infects basal epithelial cells. There are over 100 types of HPV, with some causing warts and others being carcinogenic. HPV is transmitted through skin to skin contact and replicates in a differentiation-dependent manner in the epithelium. High risk HPV types like HPV-16 and HPV-18 can lead to cancers like cervical cancer by inactivating tumor suppressor proteins. Diagnosis involves tests like Pap smear, biopsy and PCR. Prevention is through vaccination and safe sex practices, while treatment depends on the condition, ranging from topical creams for warts to surgery for precancerous lesions.