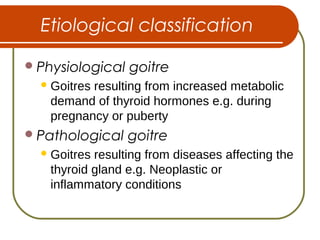
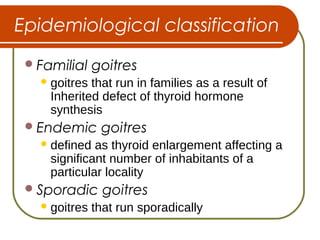
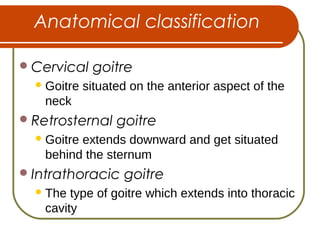
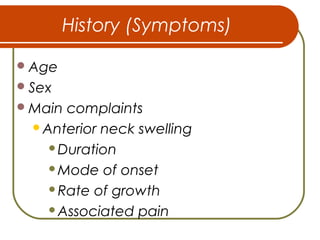
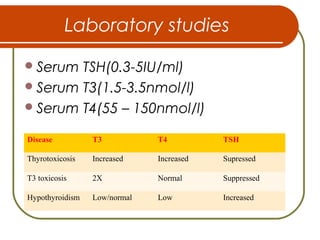
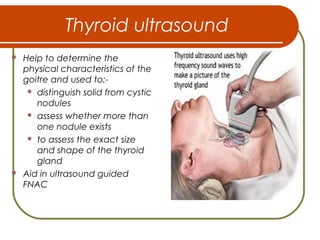
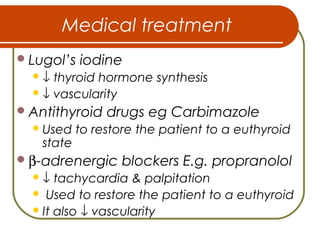
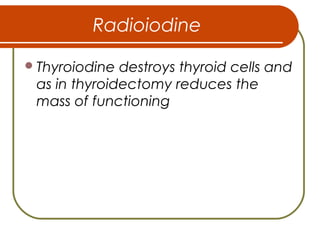
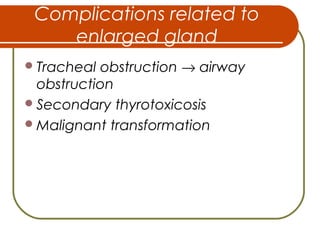
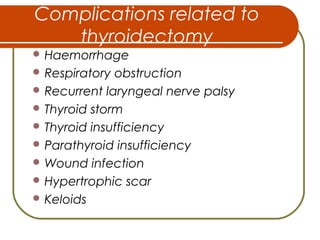
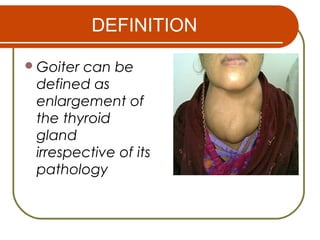
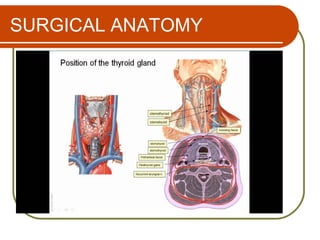
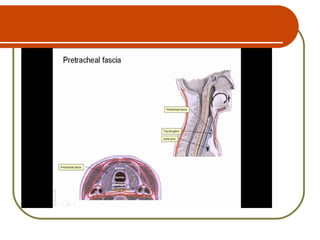
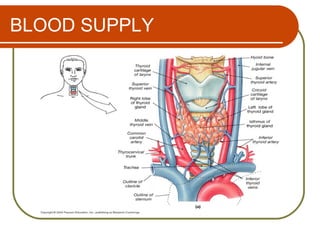
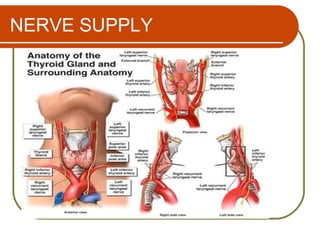
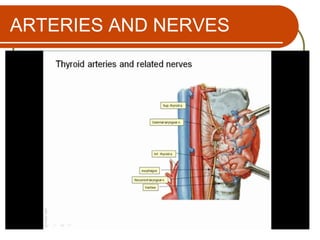
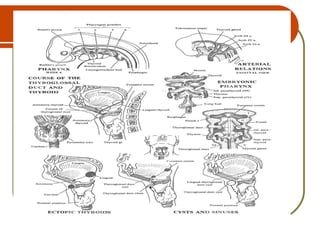
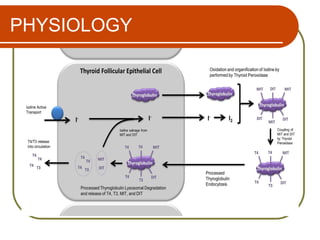
This document provides an overview of goiter (enlargement of the thyroid gland). It defines goiter and discusses the surgical anatomy and embryology of the thyroid gland. It covers the etiology, classification, pathophysiology, clinical presentation, workup, treatment, and complications of goiter. The document also discusses prevention of goiter through primary, secondary and tertiary prevention measures.
![Pharmacological factors
Use of goitrogen drugs like para-
aminosalicylic acid (PAS),
thiocyanate and antithyroid drugs
[e.g. thiouracil, carbimazole] →
hypothyroidism](https://image.slidesharecdn.com/goitres-160130110729/85/Goitres-19-320.jpg)