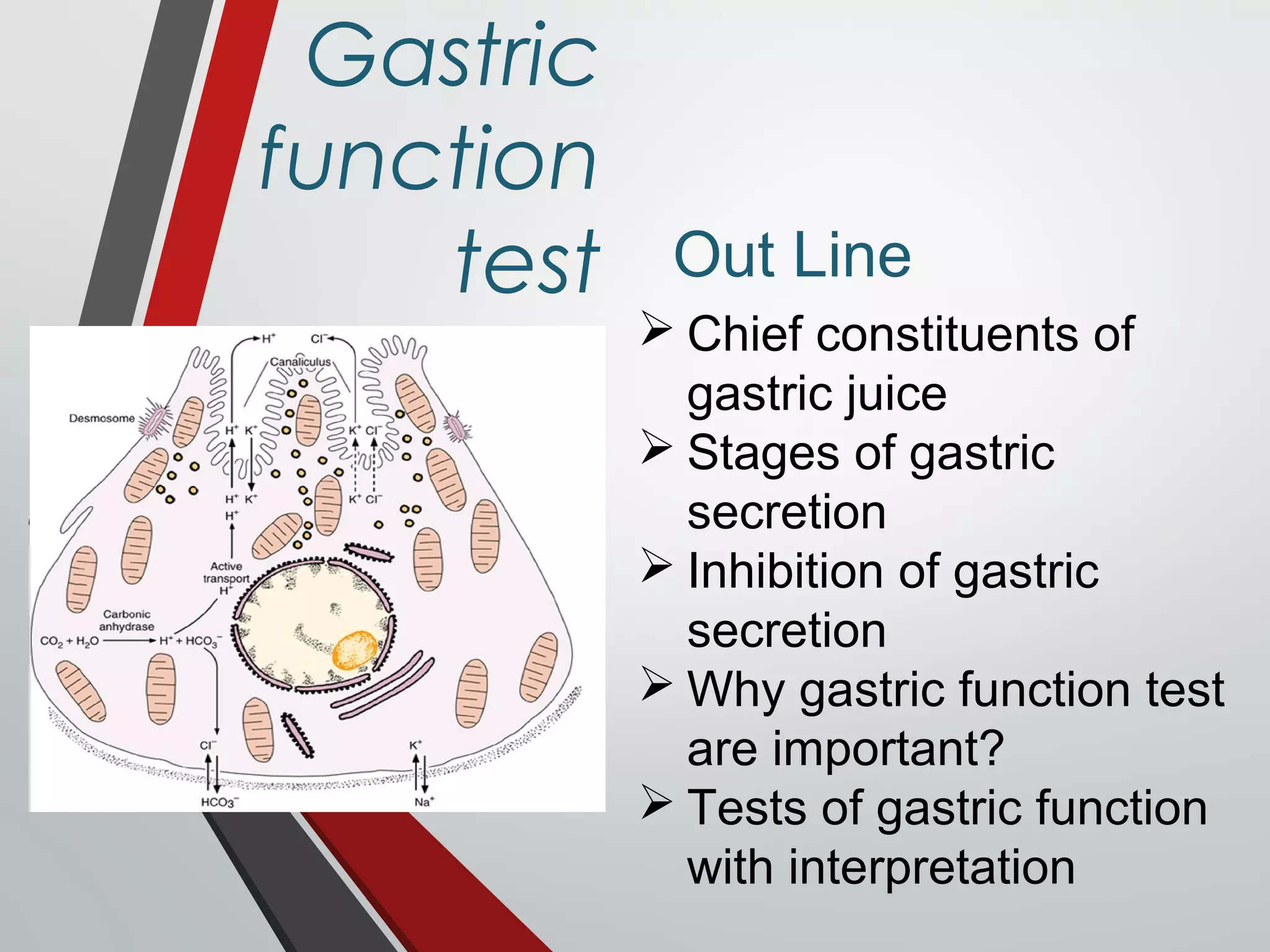
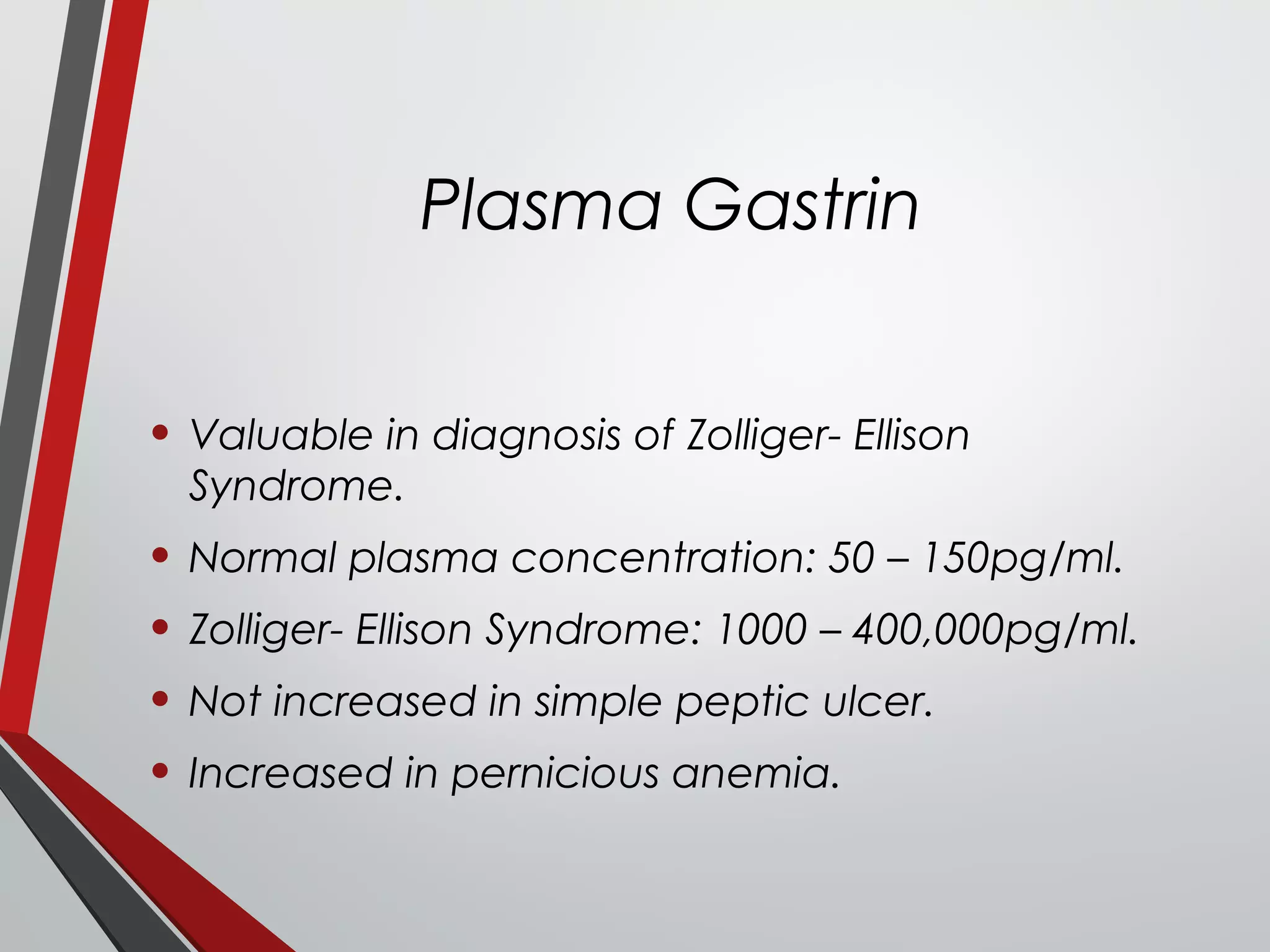
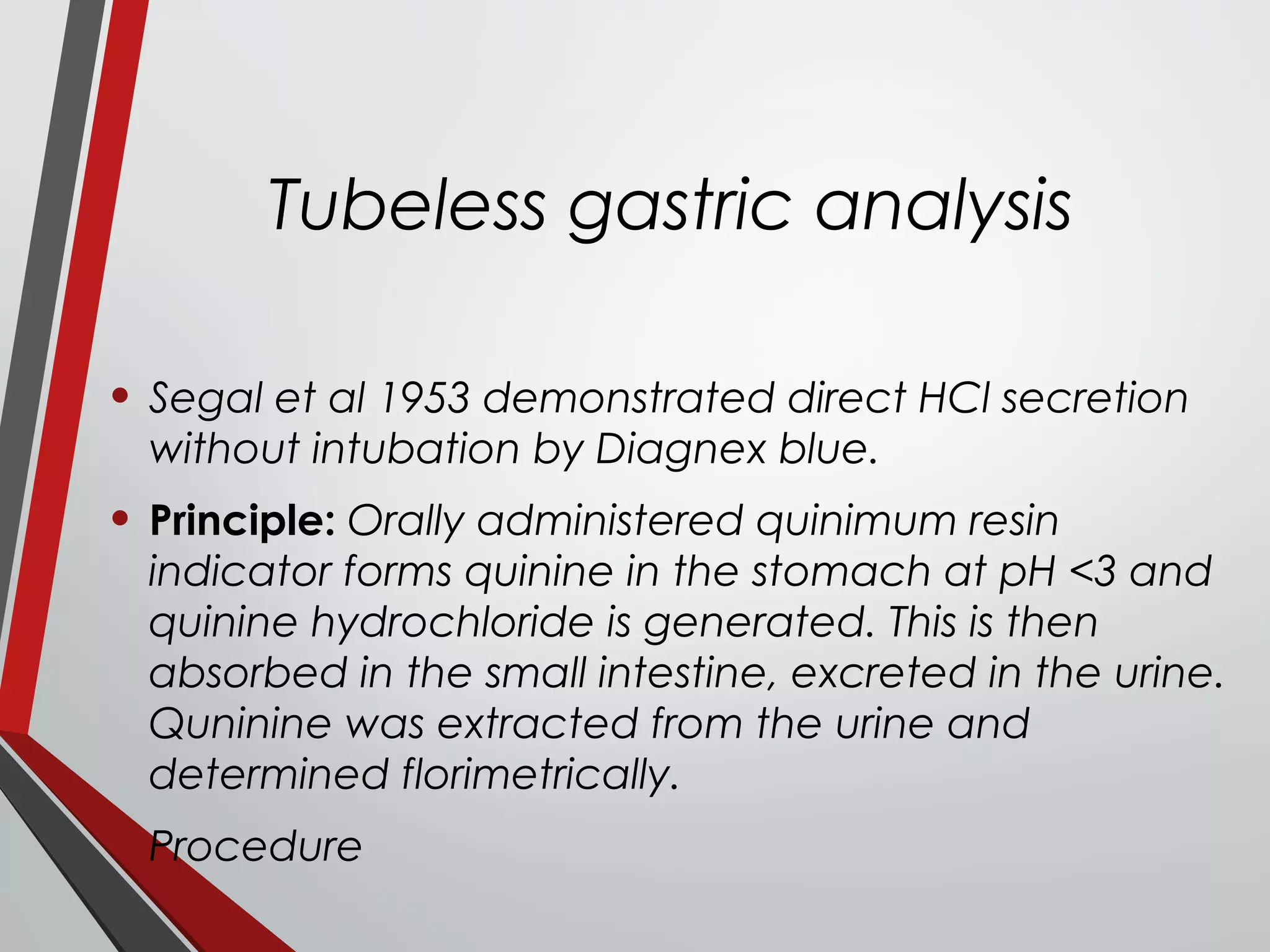
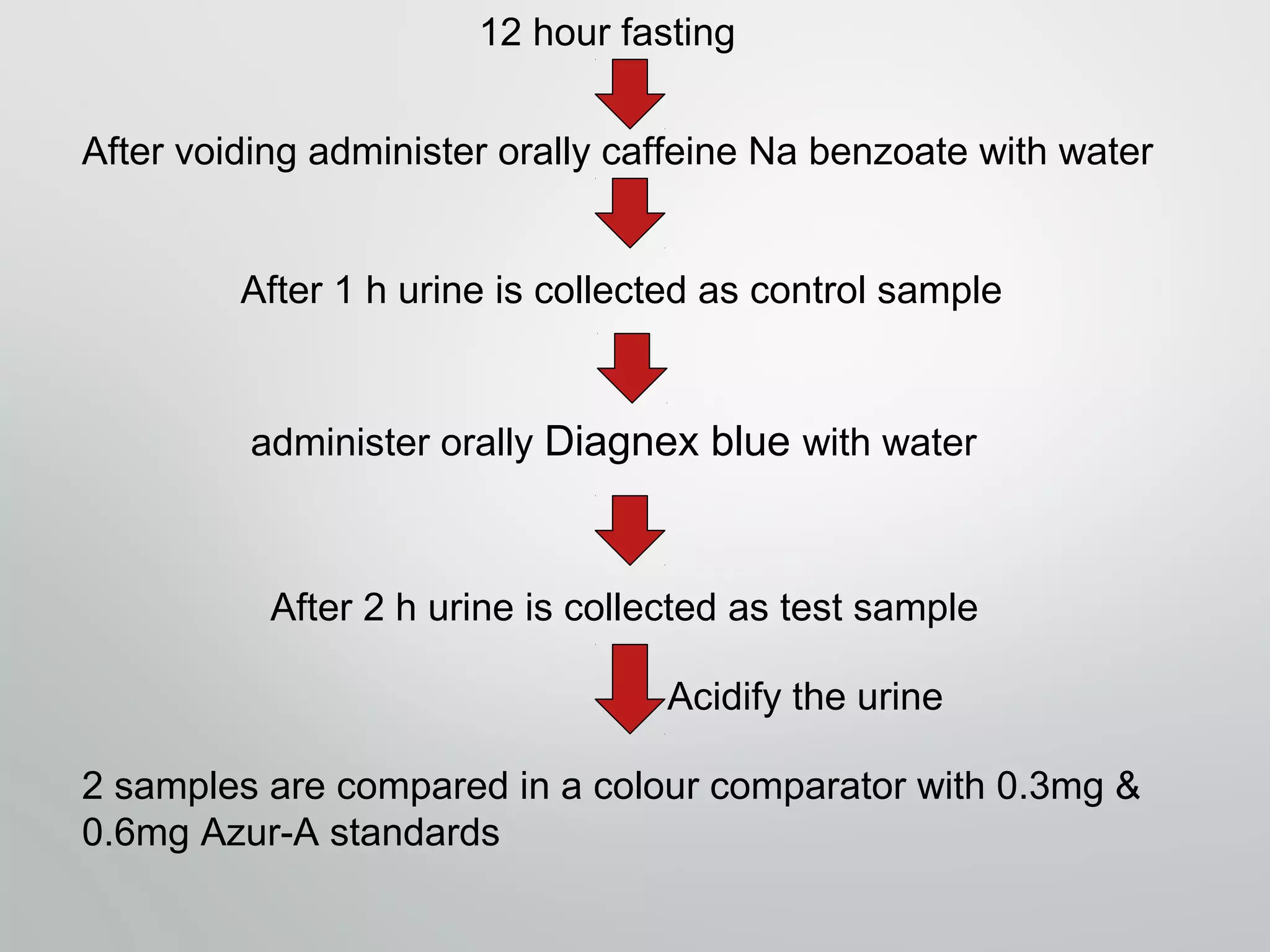
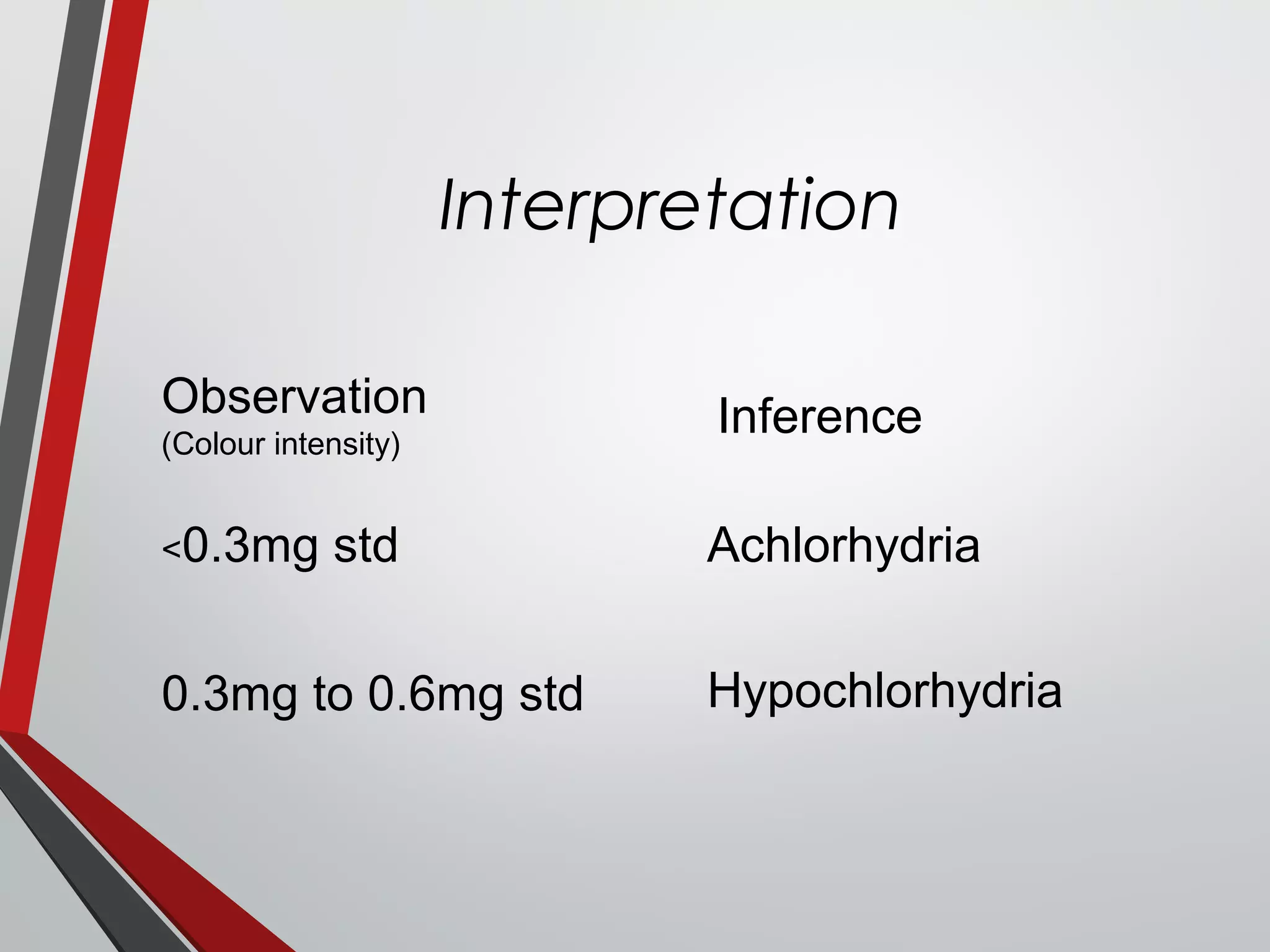
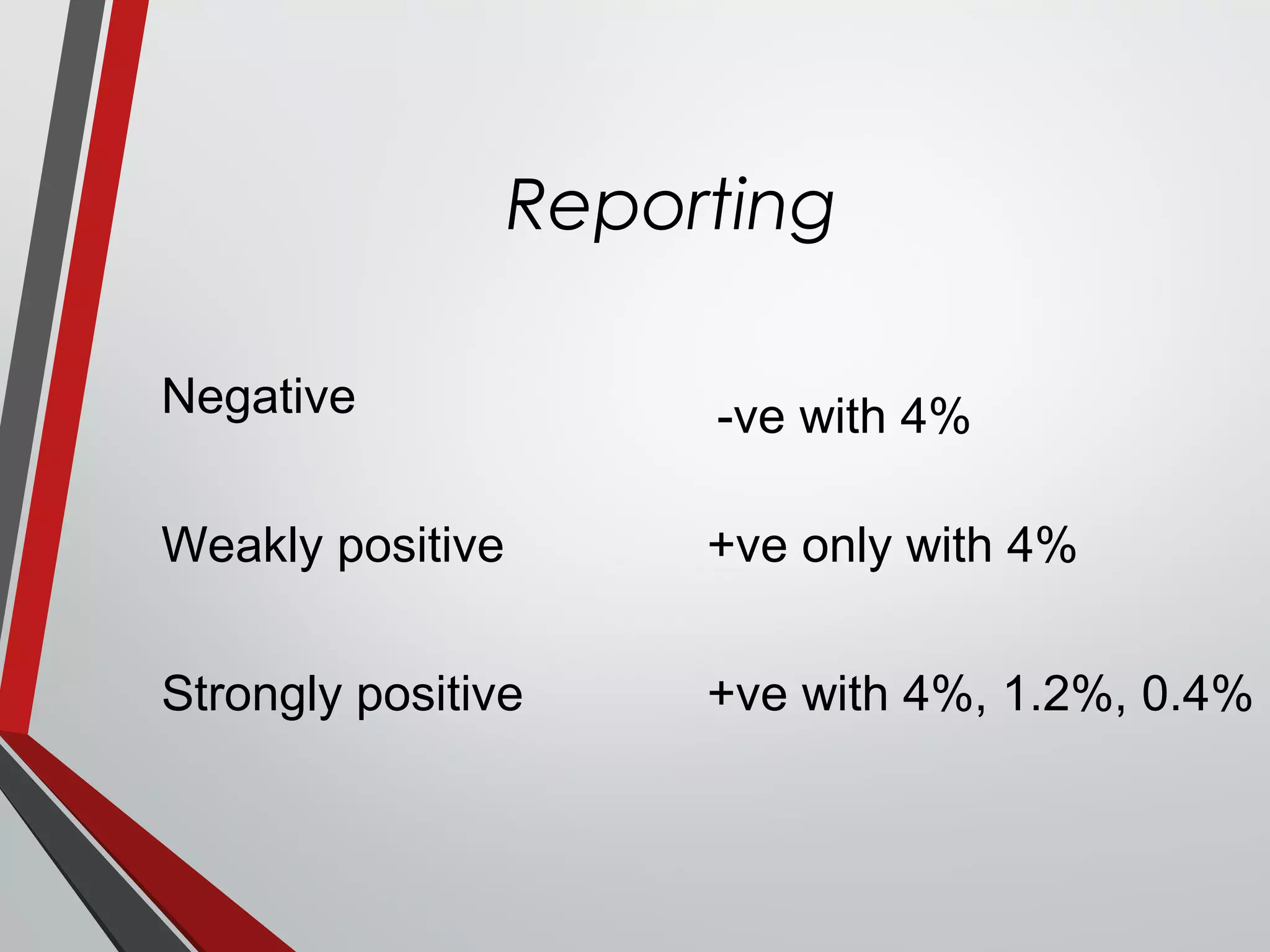
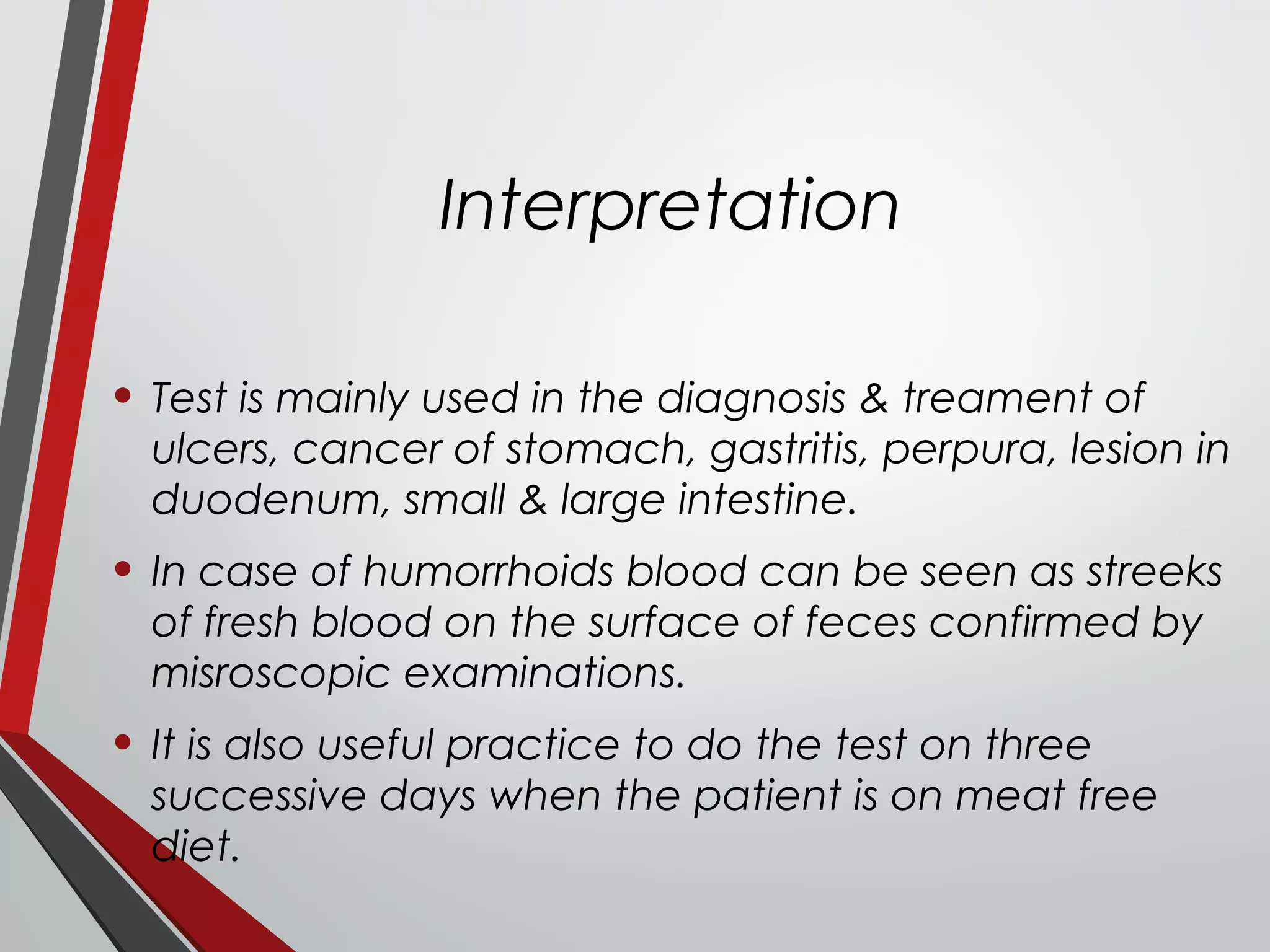
The document provides a comprehensive overview of gastric and pancreatic function tests, highlighting the normal constituents and secretion phases of gastric juice, as well as various tests for assessing gastric function and their interpretations. It also covers pancreatic exocrine secretions, methods for analyzing amylase and lipase activity, and diagnostic significance in diseases like Zollinger-Ellison syndrome and pancreatitis. The document emphasizes the importance of these tests in diagnosing gastrointestinal disorders and tailoring appropriate treatments.
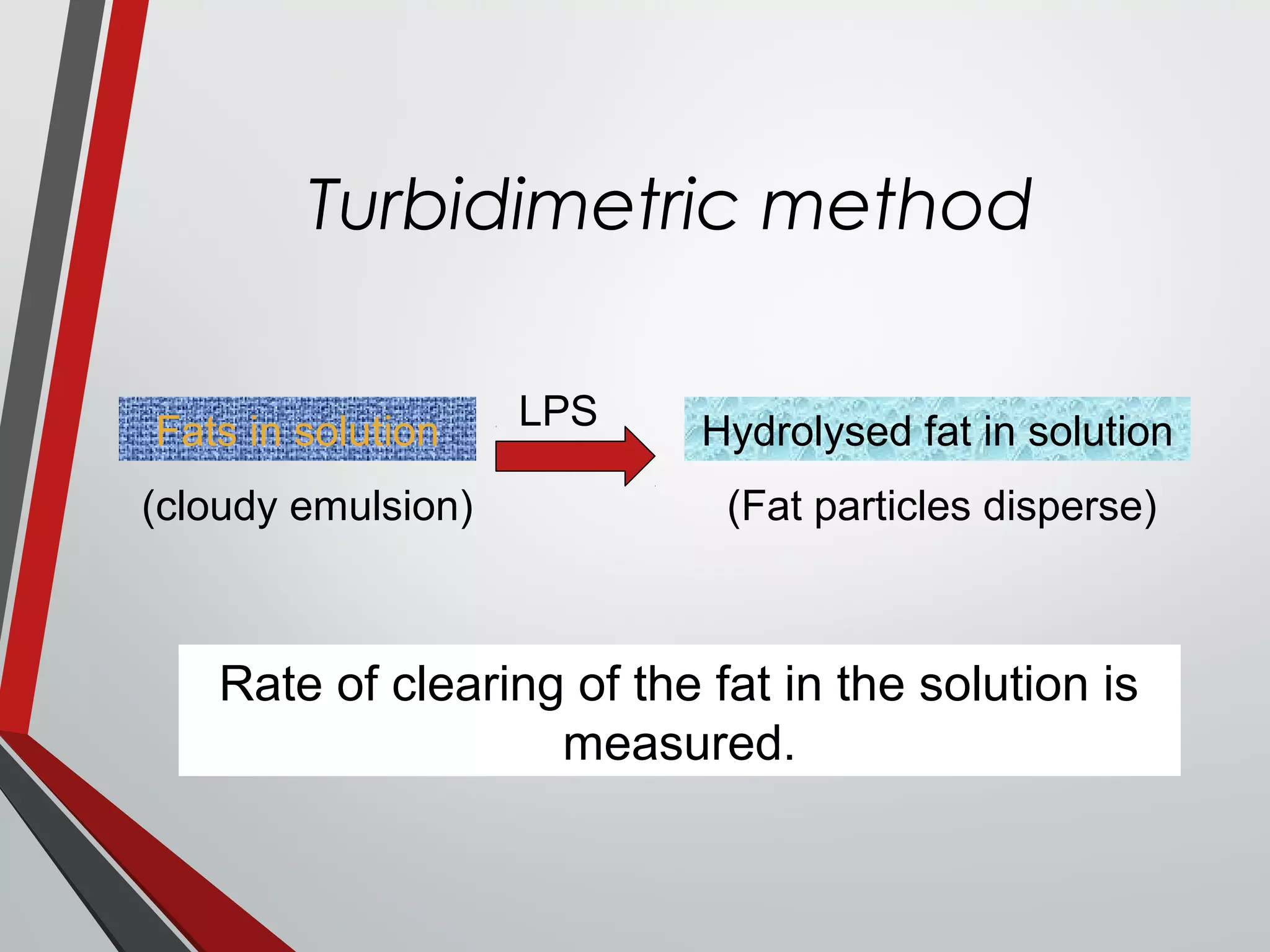
![Out Line
Exocrine secretions of
Pancrease
Tests in Pancreatic Diseases
with interpretation
Determination of [HCO3
-
]
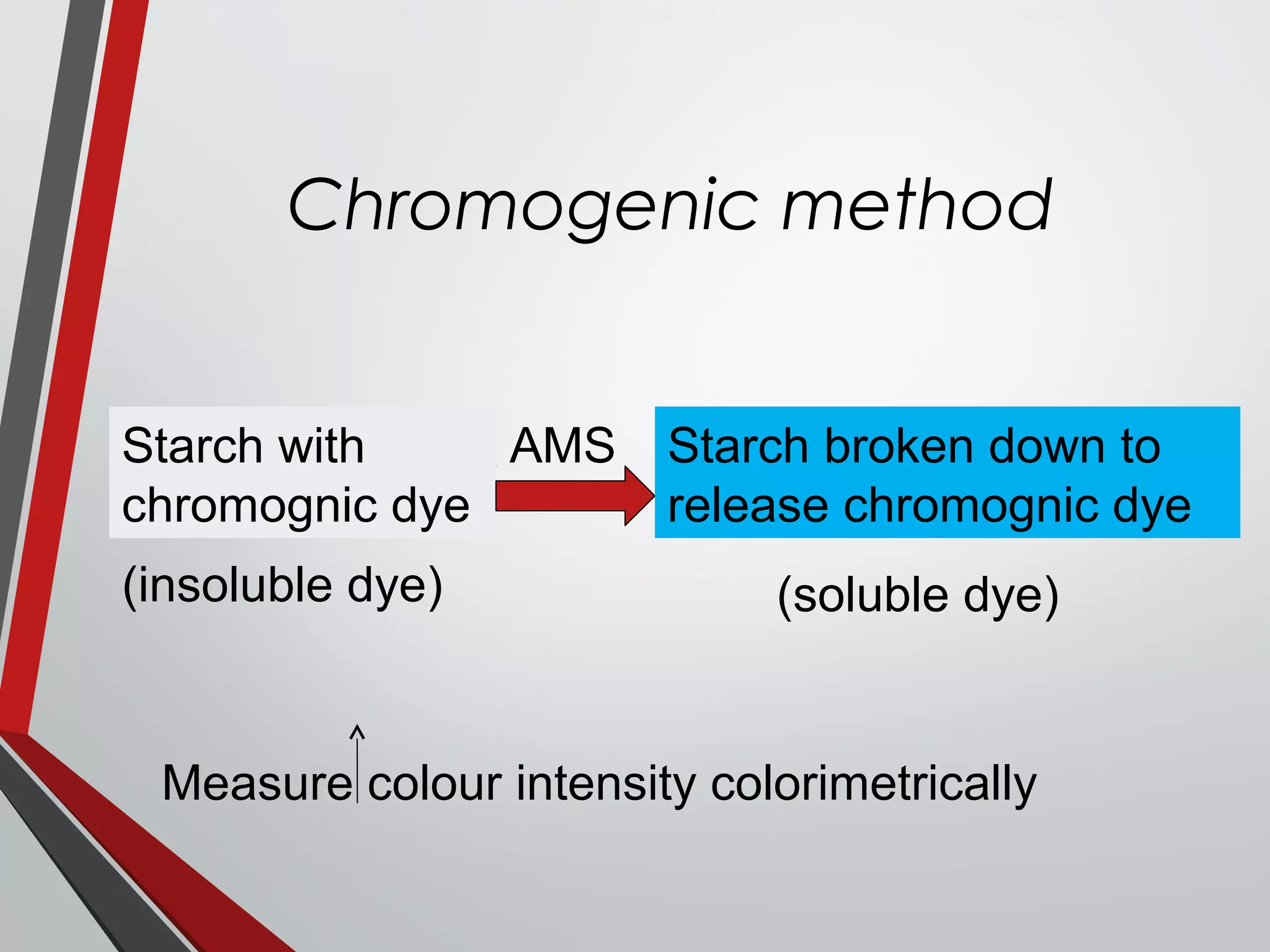
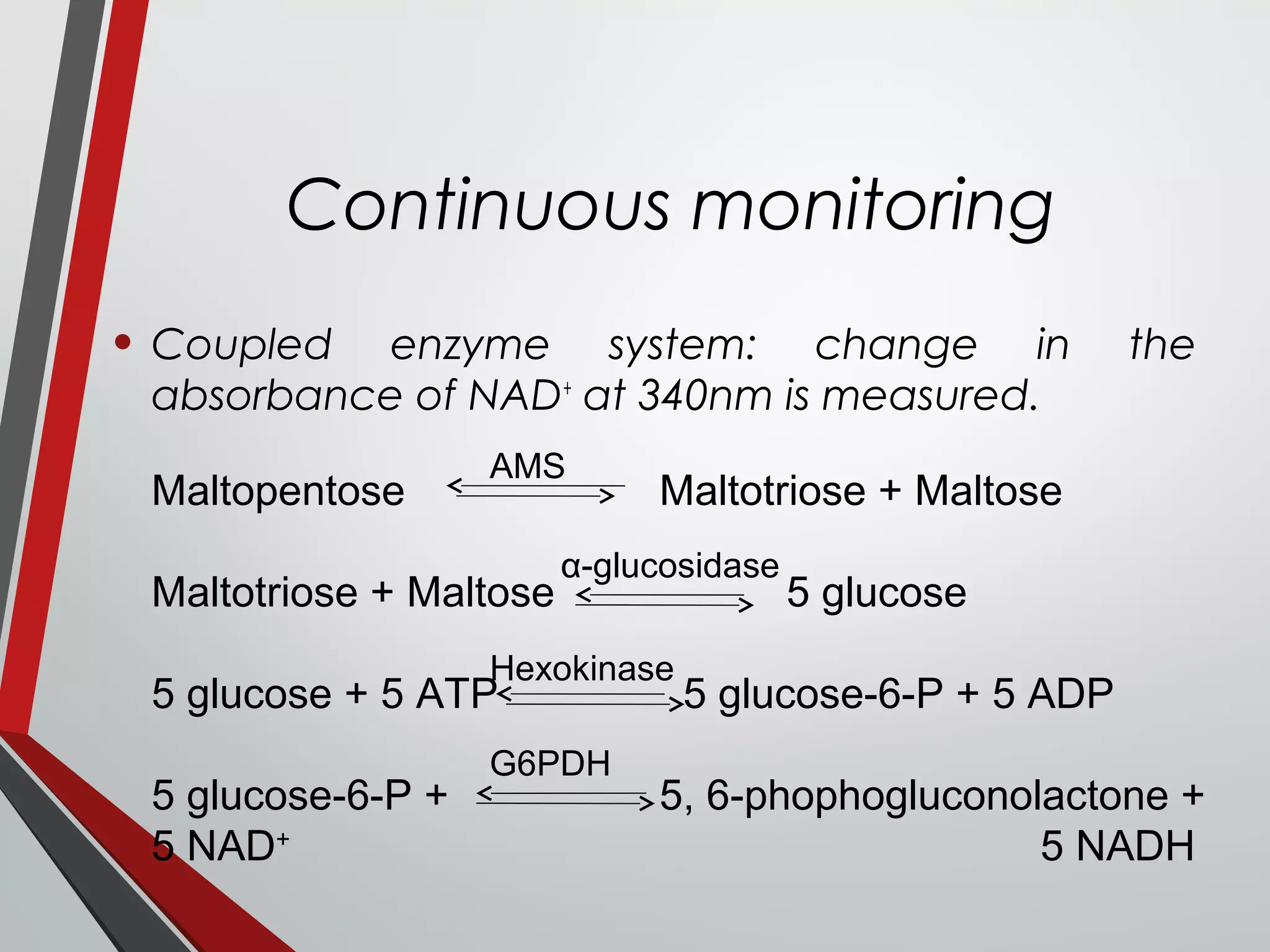
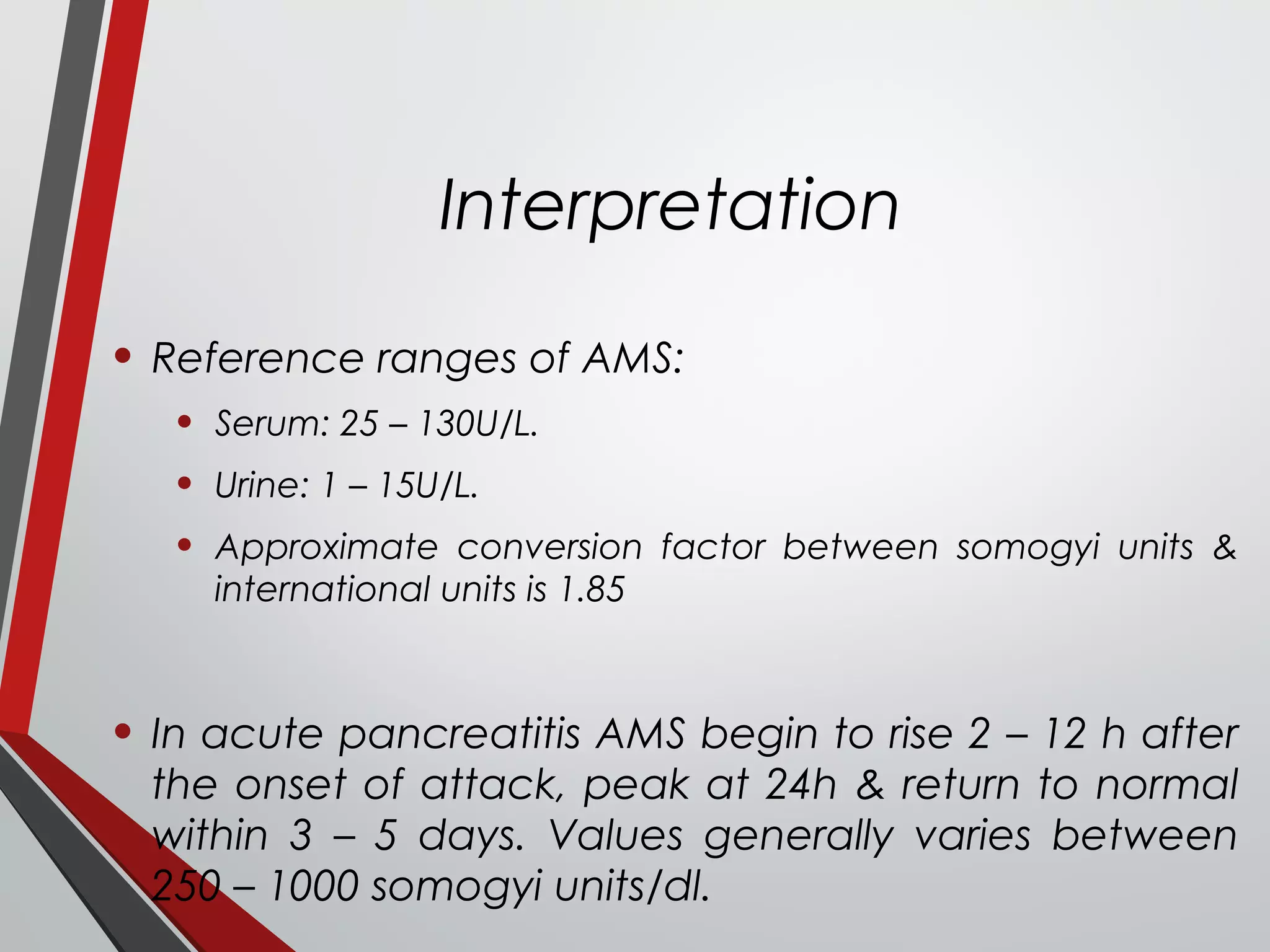
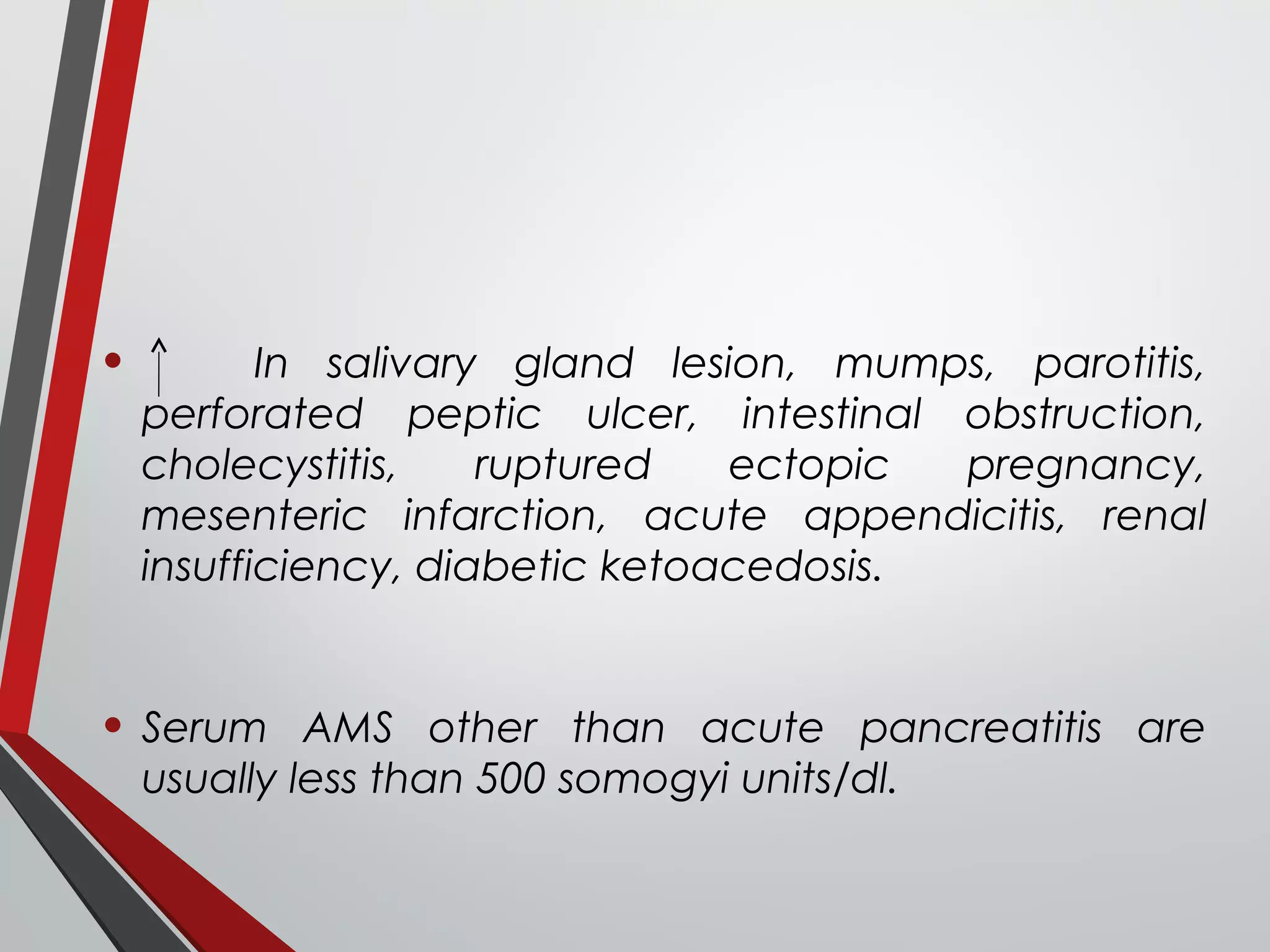
Amylase (AMS)
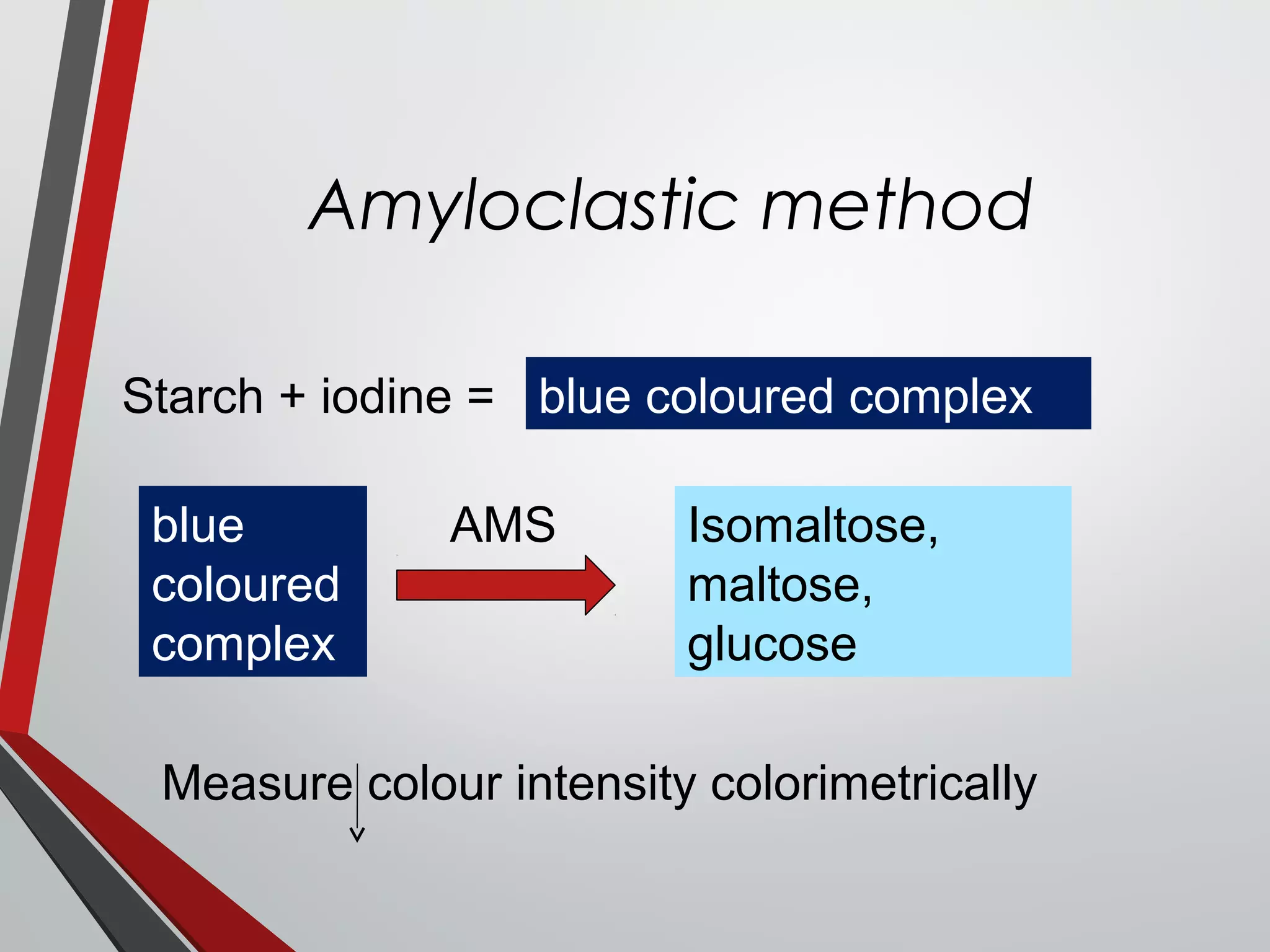
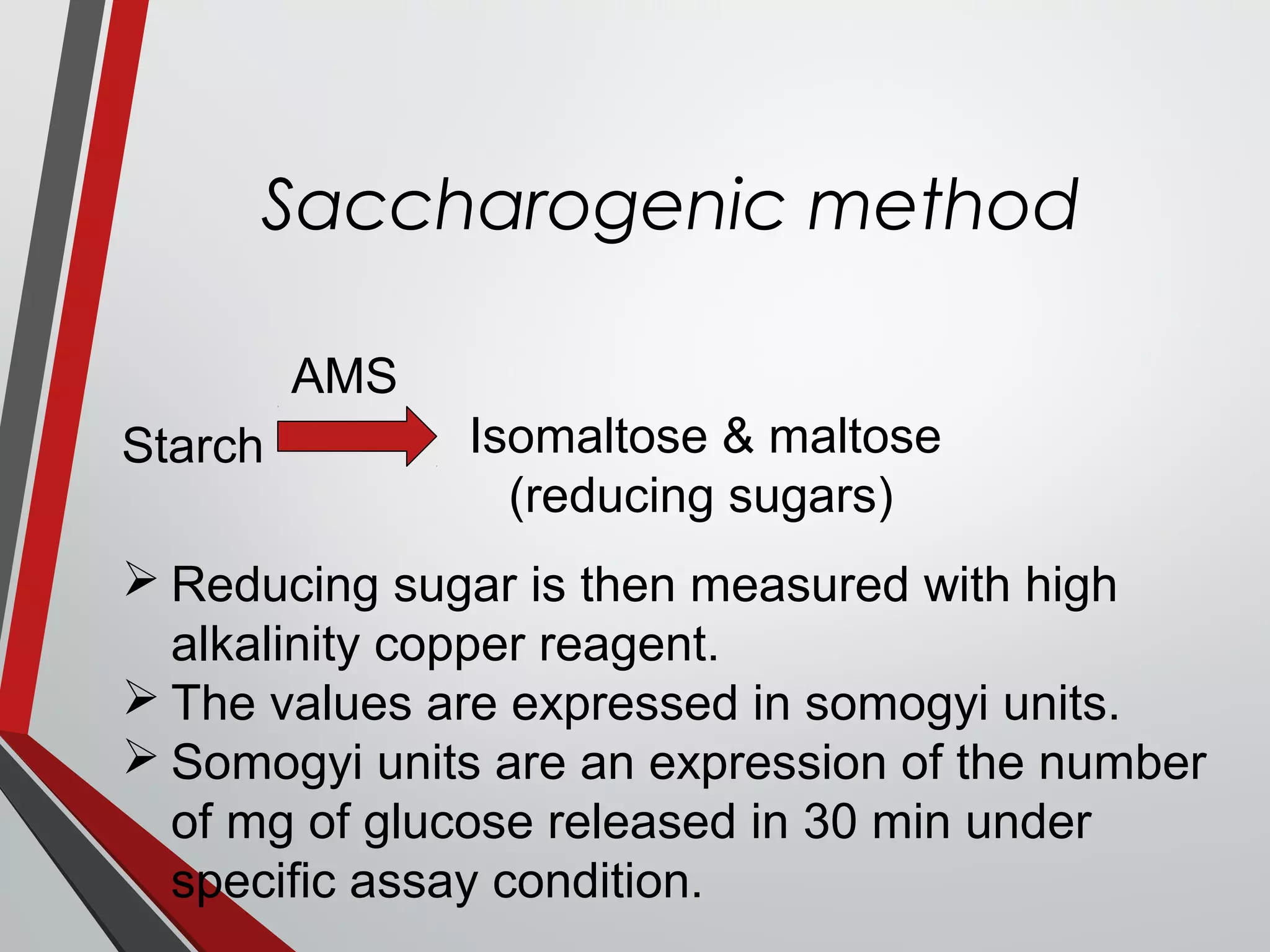
Essay of AMS activity
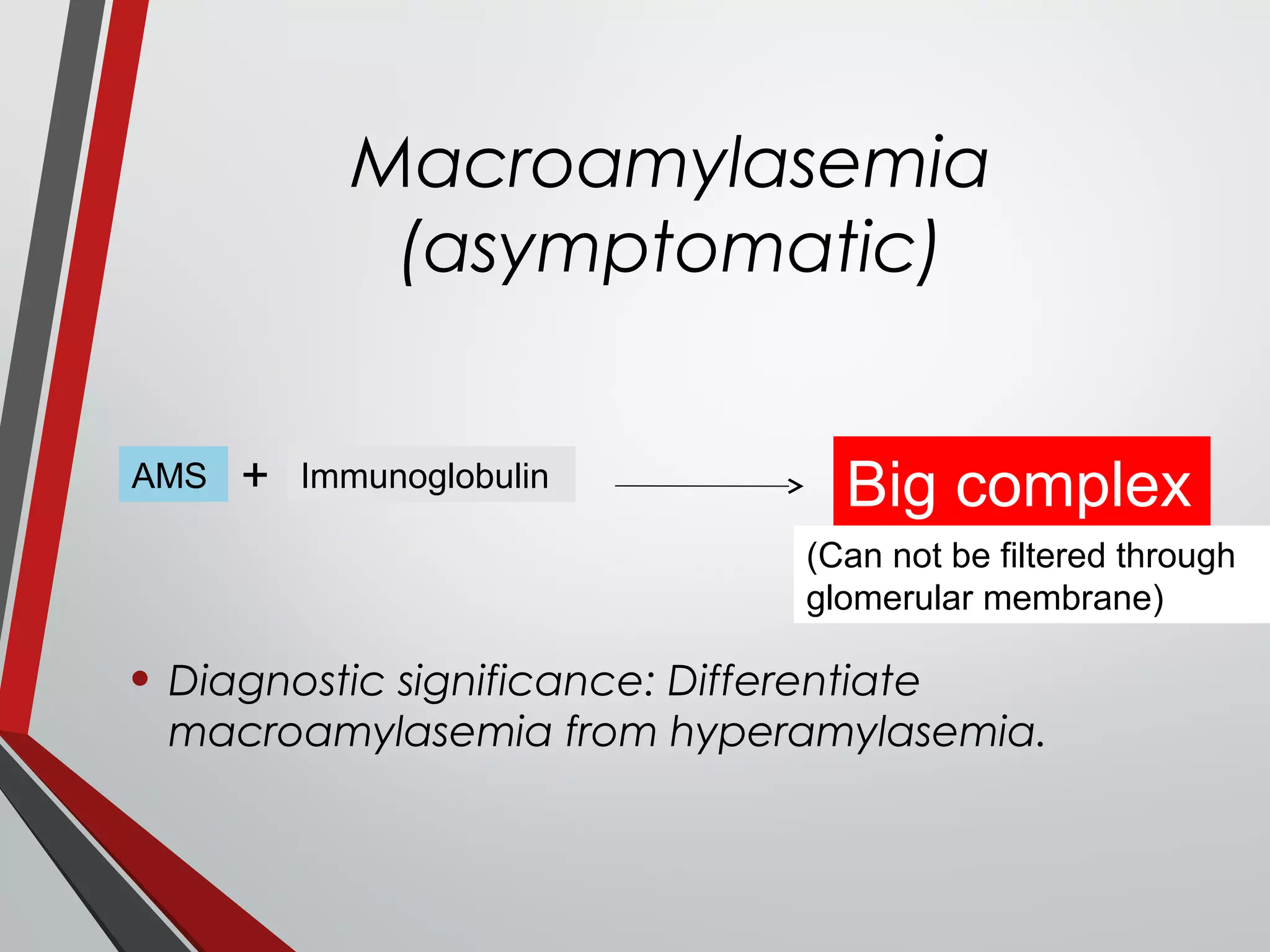
Macroamylasemia
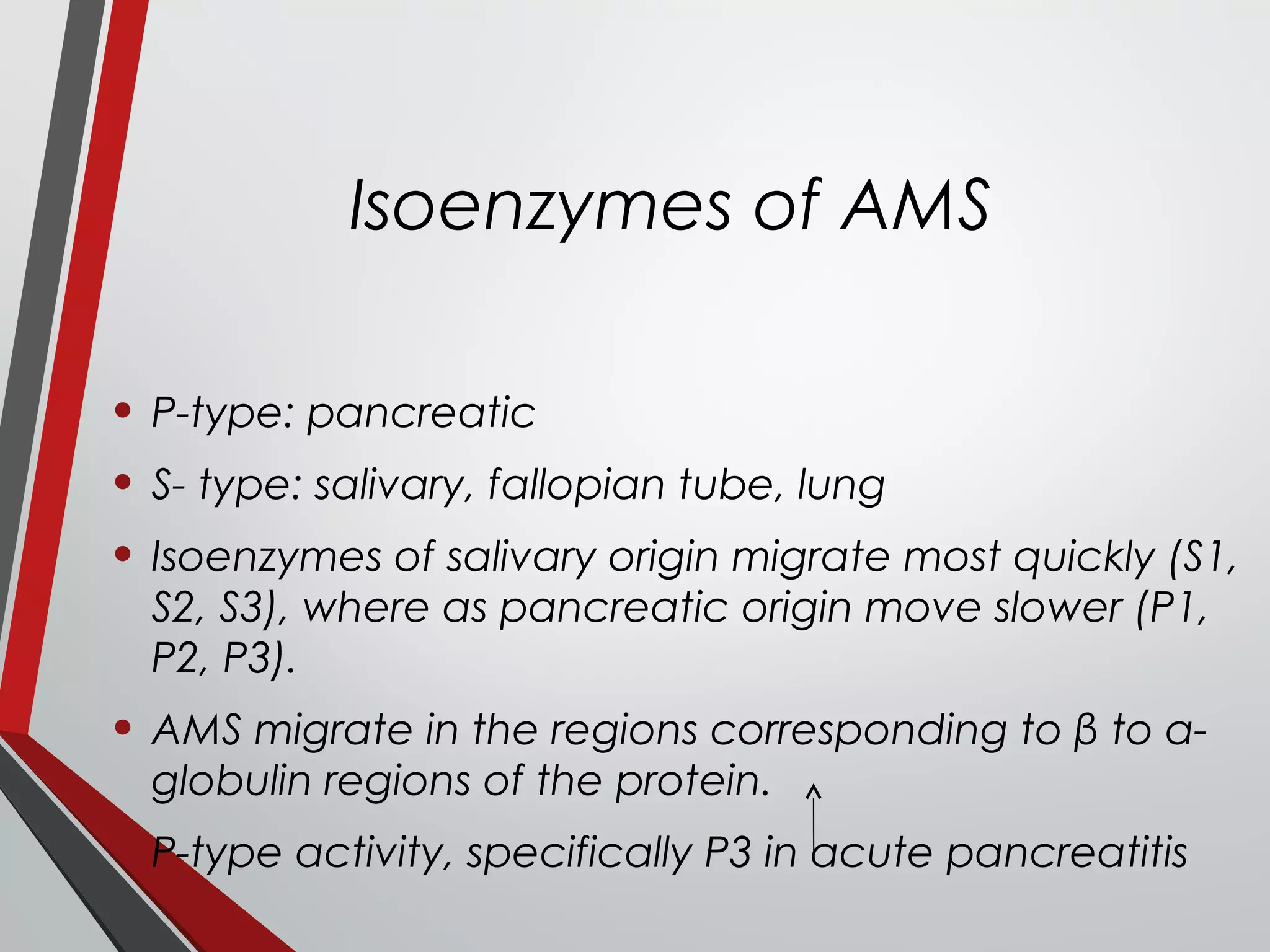
Isoenzymes of AMS
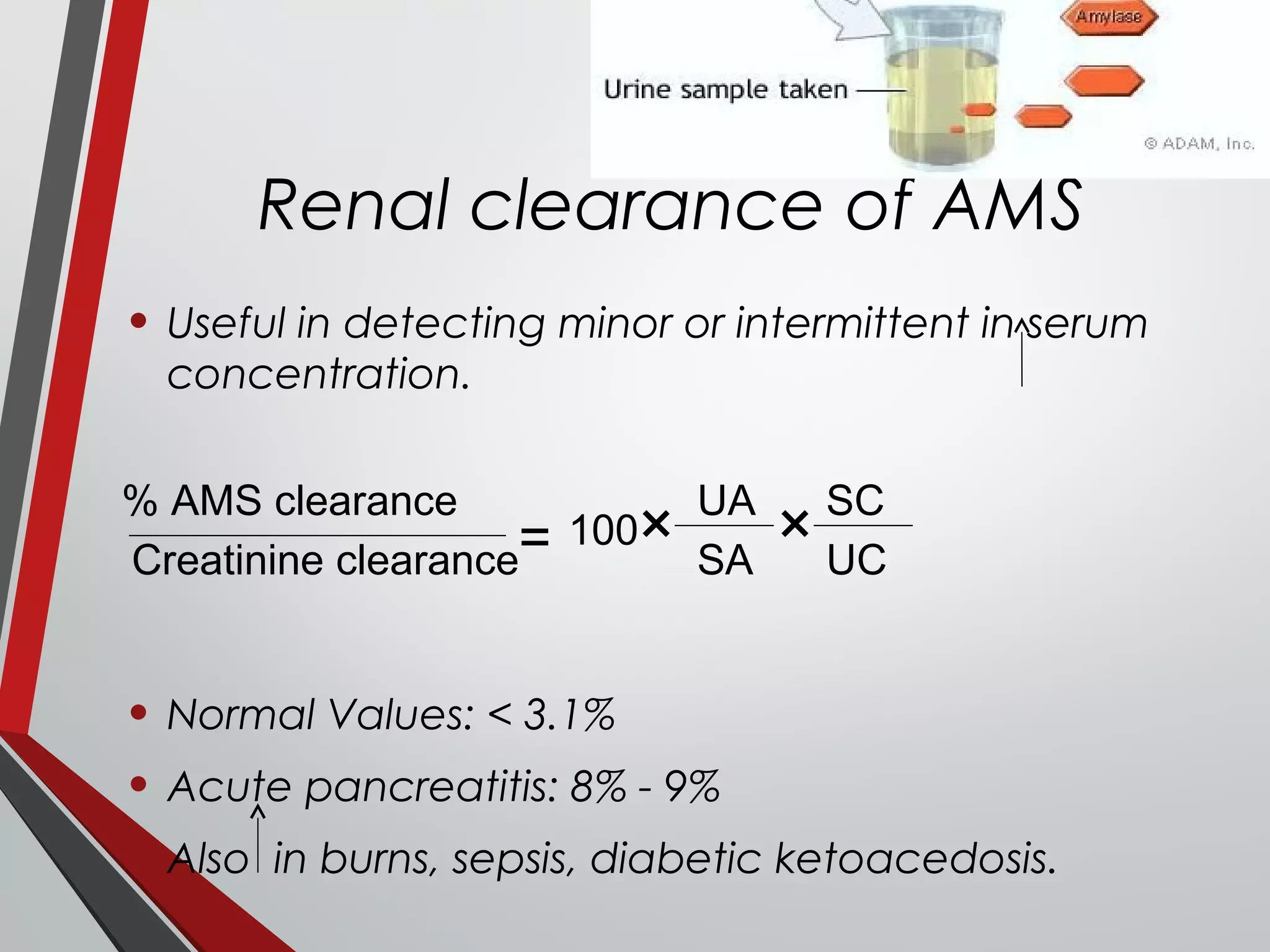
Renal clearance of AMS
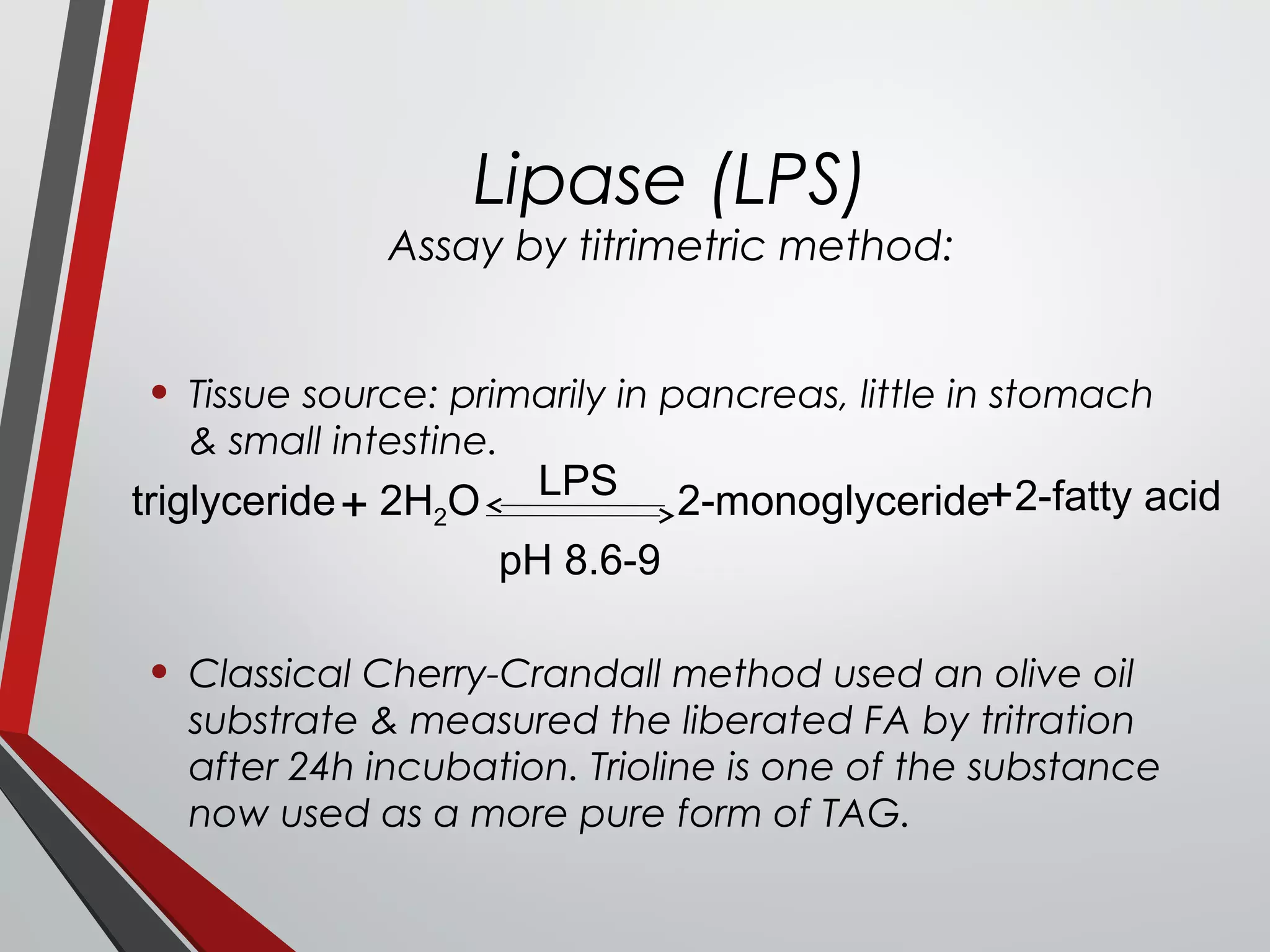
Lipase (LPS)
Assay of LPS activity](https://image.slidesharecdn.com/gastricfunctiontest-160911172756/75/Gastric-and-Pancreatic-function-tests-29-2048.jpg)
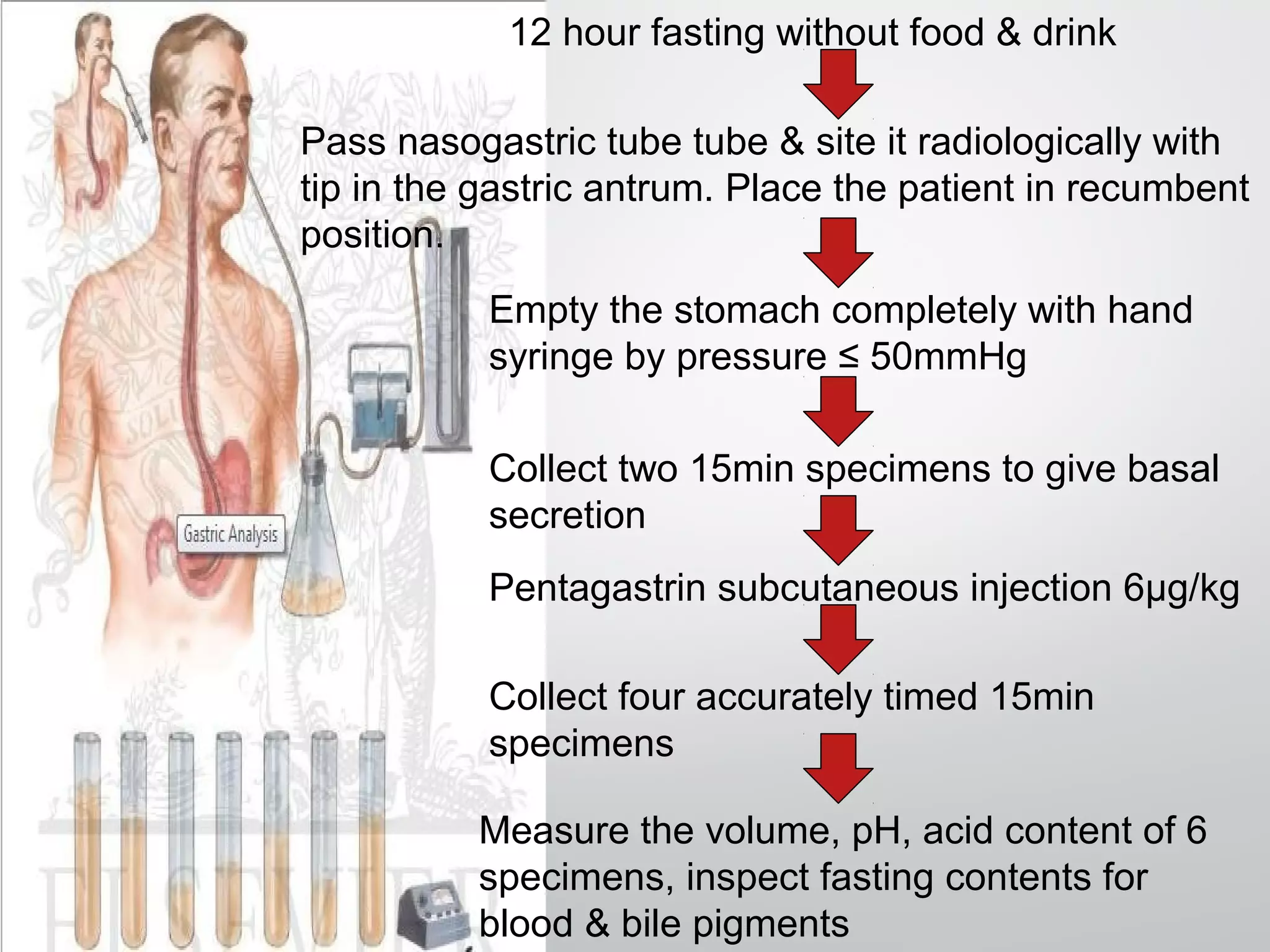
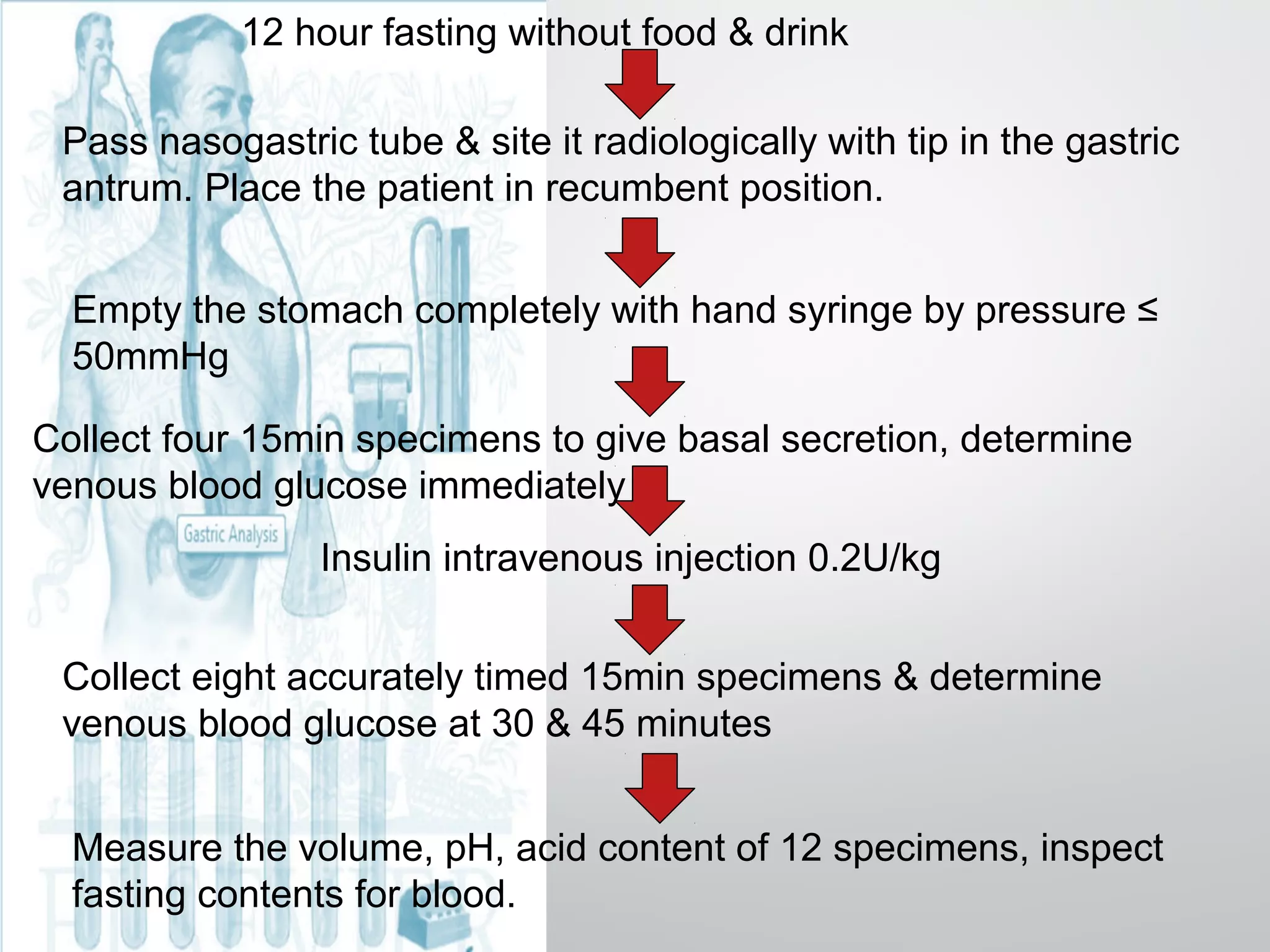
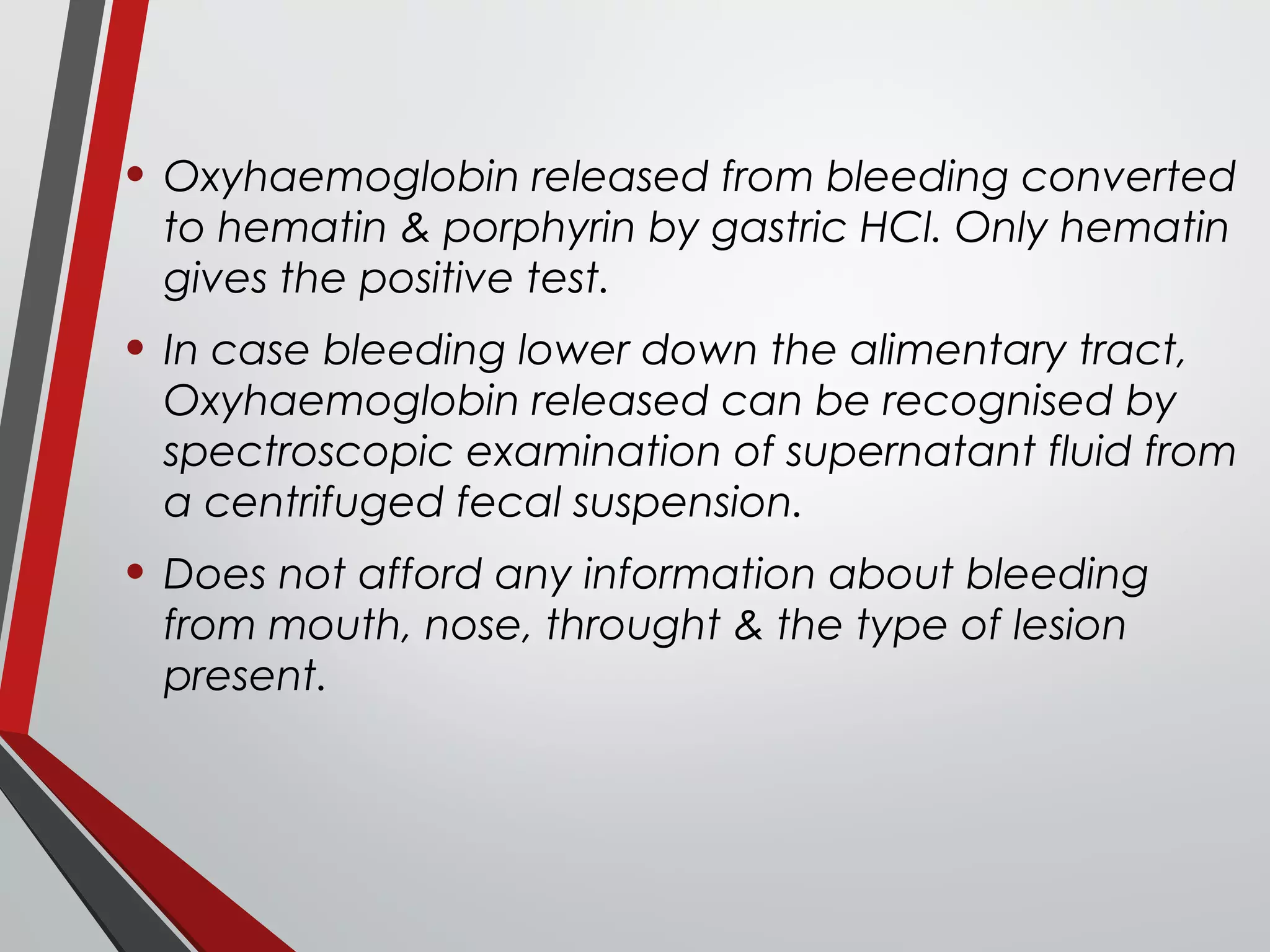
![12 hour fasting without food & drink
Pass the double lumen tube & site it radiologically with tip of inner
tube in the 3rd
part of duodenum.
Clear bile stained juice (two 10min samples) from the deuodenal tube
& juice free from bile from gastric tube were collected as basal
secretion.
2-3U/kg Secretin/CCK-PZ administred intravenously over 2 min.
Pancreatic secretions are collected for 30, 60, 80 minutes.
pH, secretory rate, [HCO3
-
] are measured.](https://image.slidesharecdn.com/gastricfunctiontest-160911172756/75/Gastric-and-Pancreatic-function-tests-32-2048.jpg)
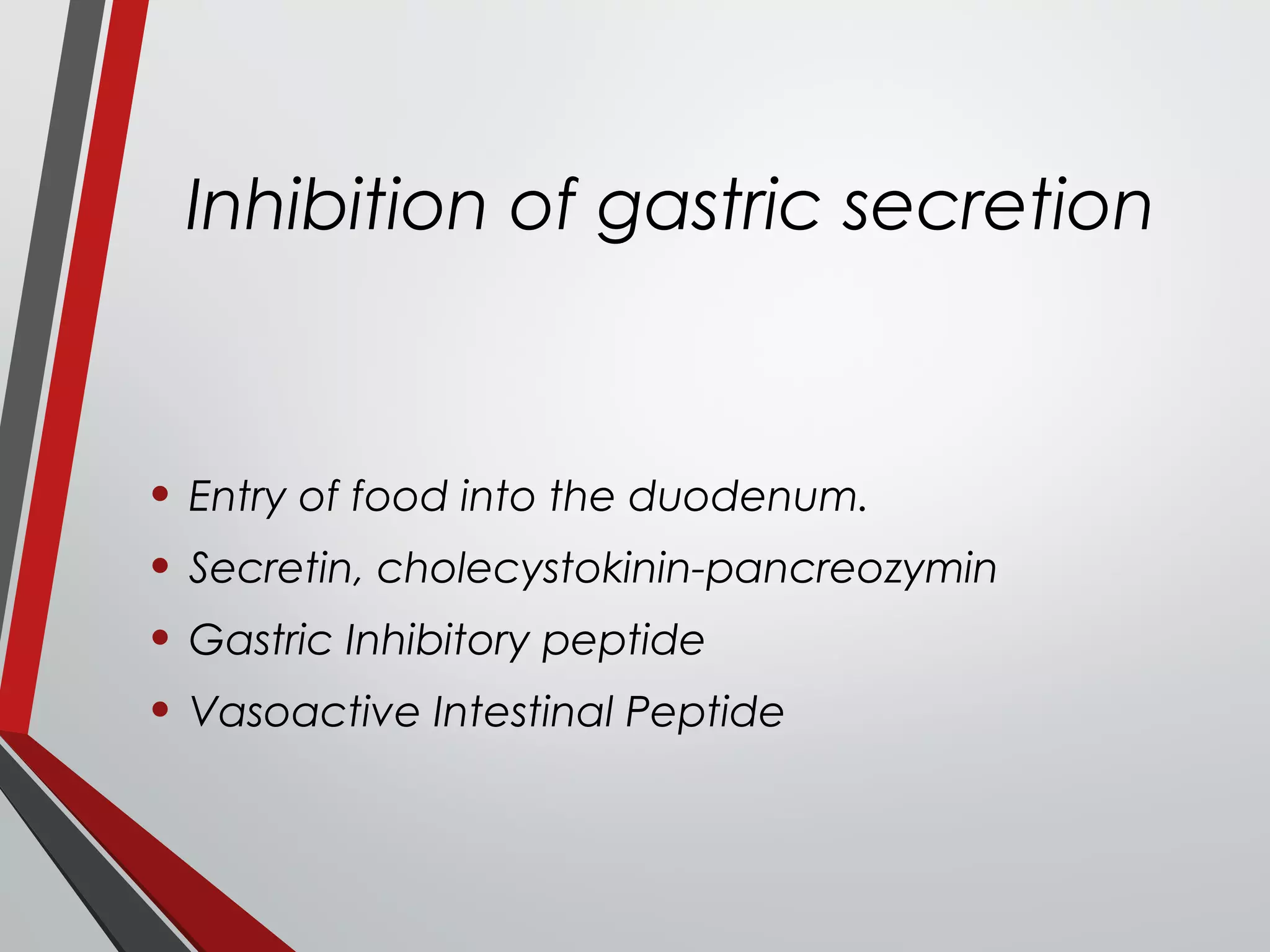
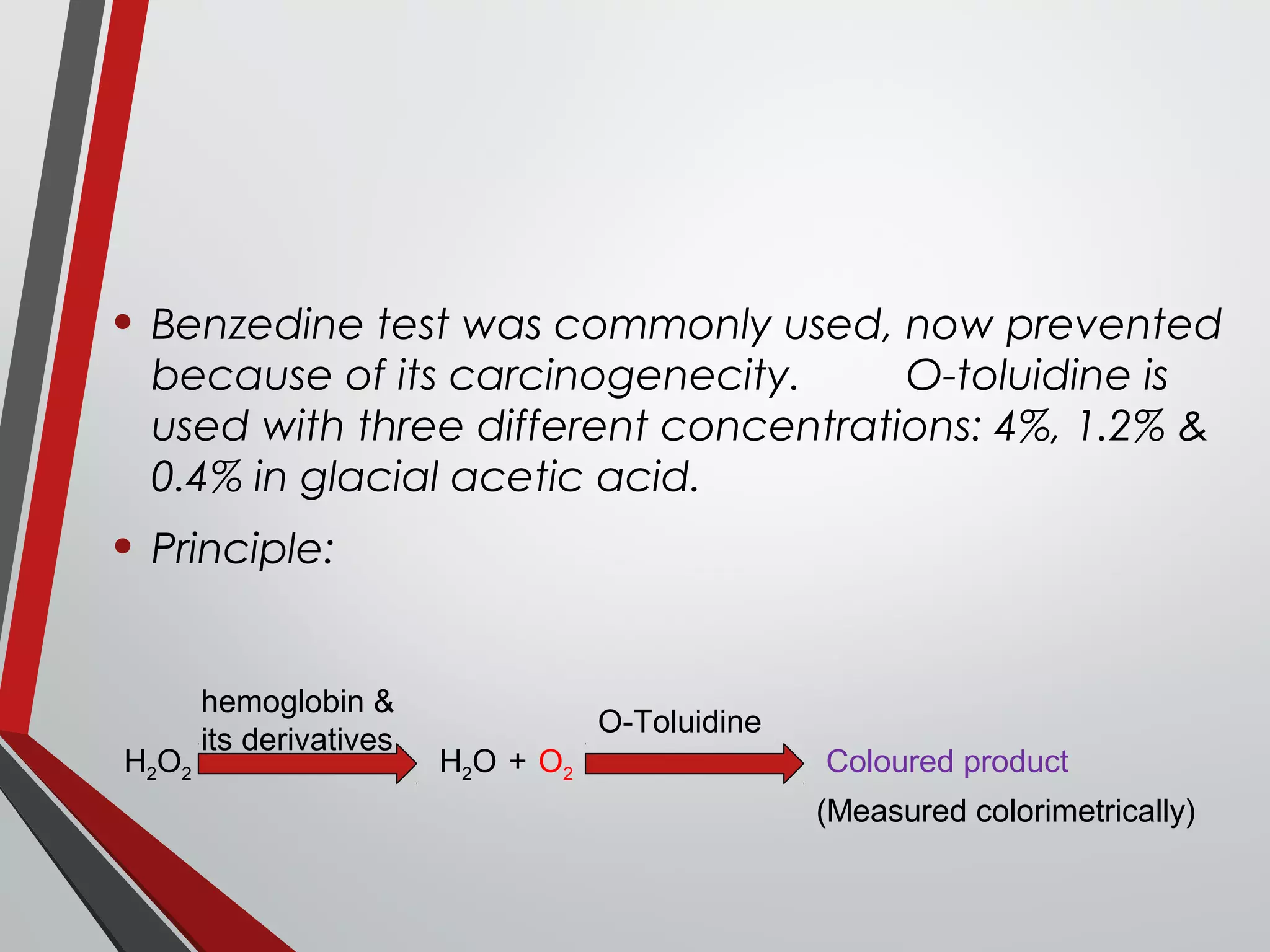
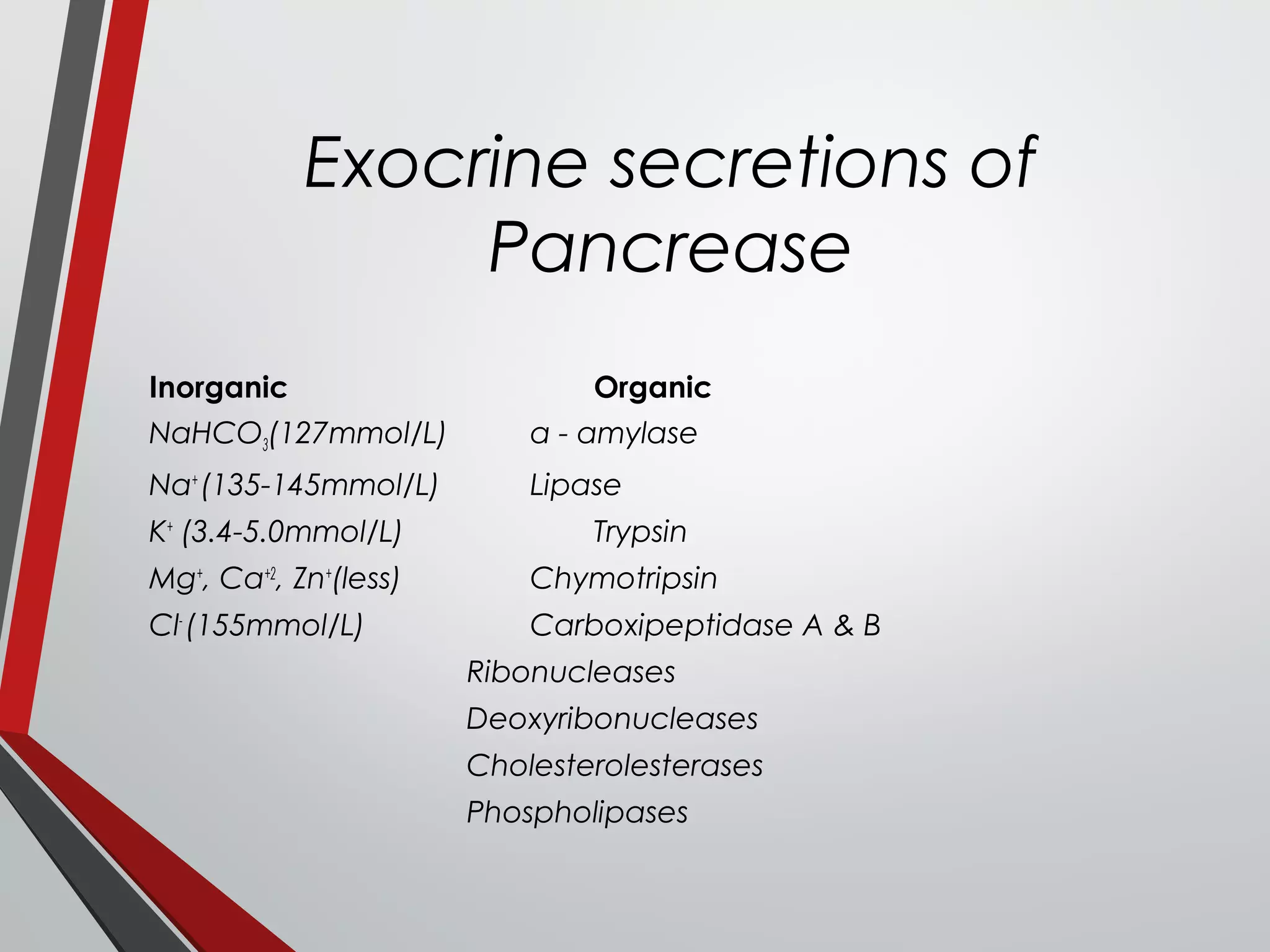
![Determination of [HCO3
-
]
• To 5ml duodenal juice add 10ml of 100mmol/l
HCl in a small beaker, boil to expel CO2, cool &
titrate with 100mmol/l NaOH to pH 7.0 by a glass
electrode or to an end point with
phenolphthalein indictor.
• [HCO3
-
] in mmol/l =
(Vol. of HCl – Vol. of NaOH) 20](https://image.slidesharecdn.com/gastricfunctiontest-160911172756/75/Gastric-and-Pancreatic-function-tests-33-2048.jpg)
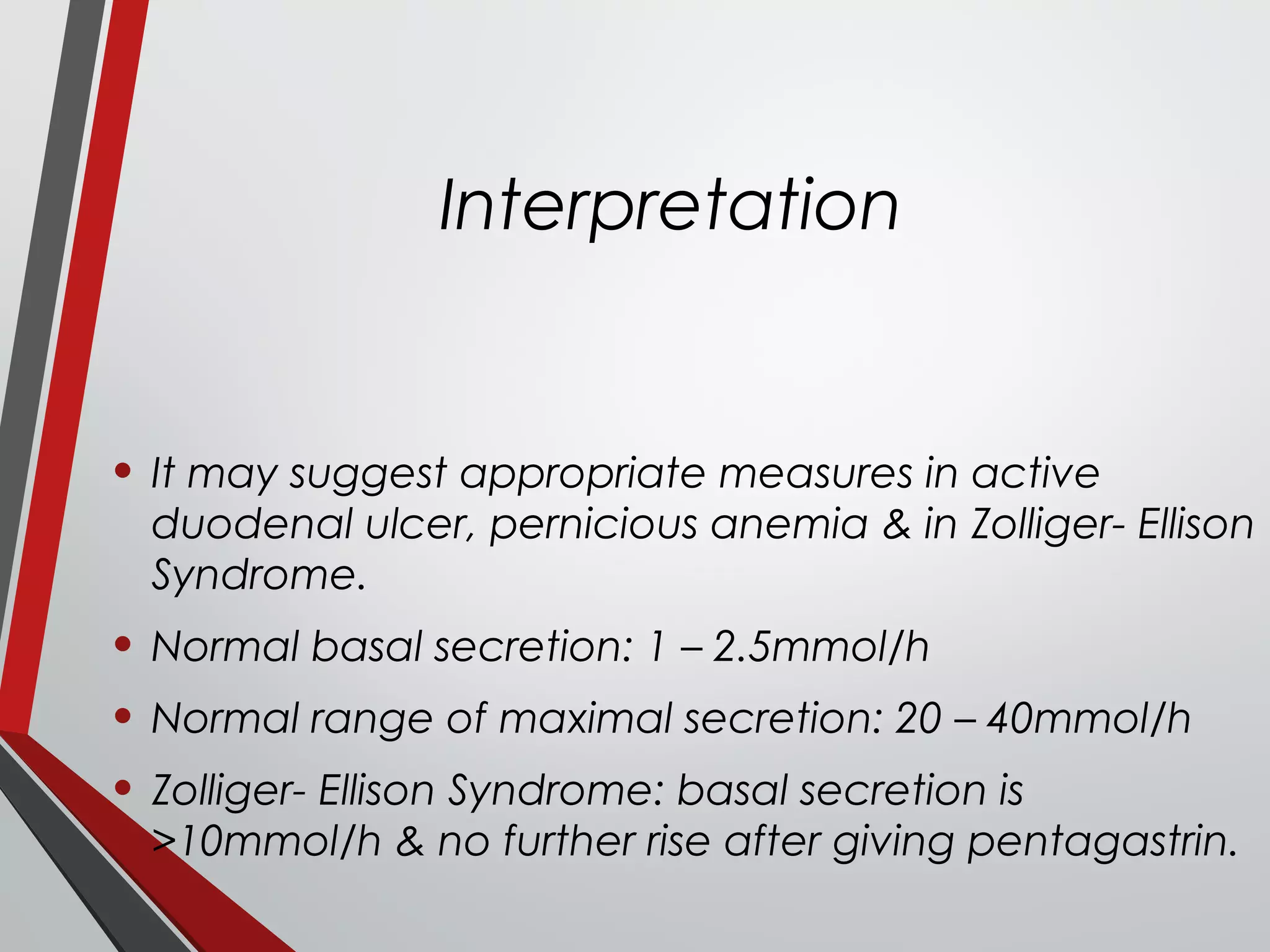
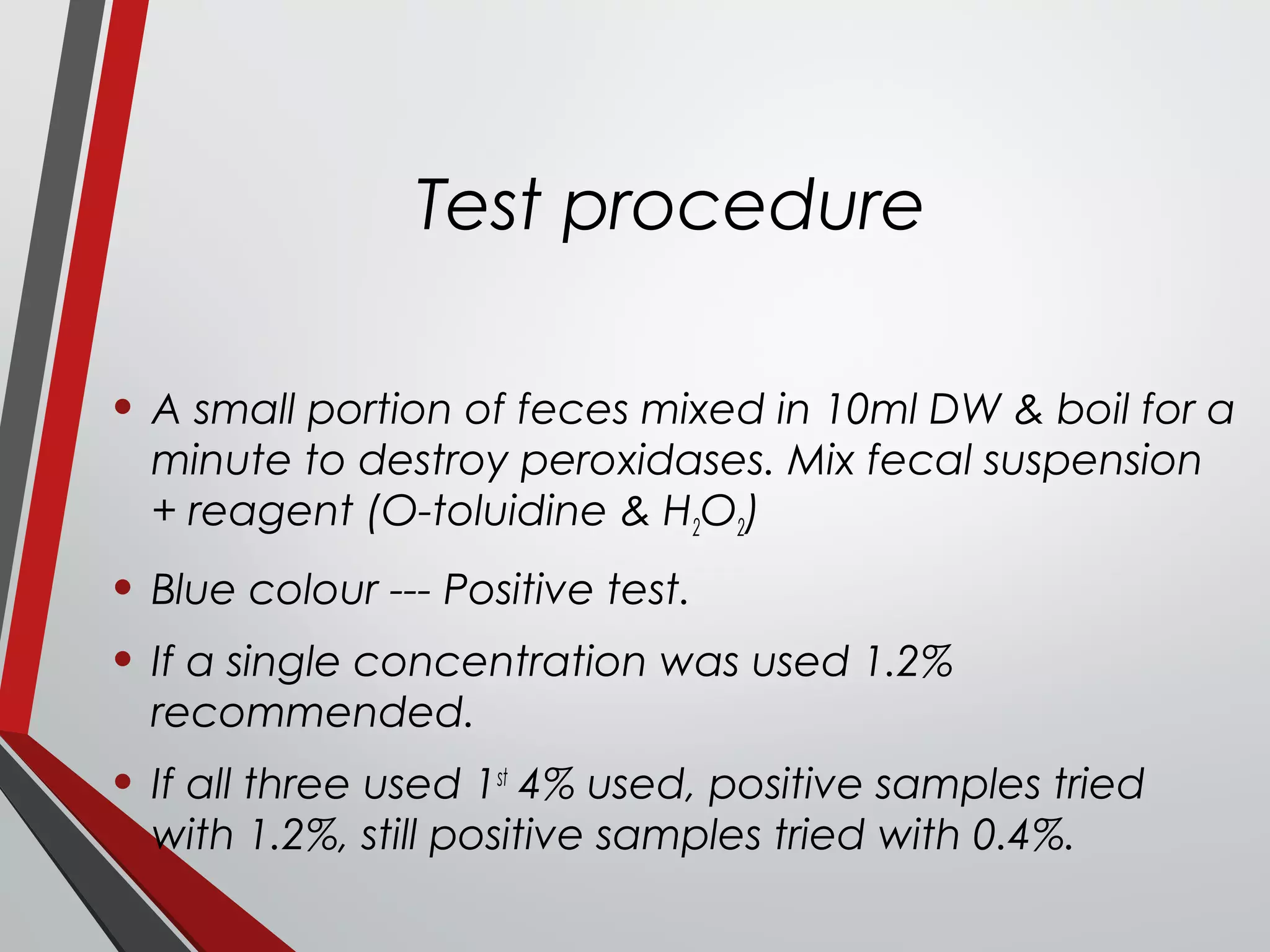
![Interpretation
• Normal [HCO3
-
] = 127mmol/L
• Secretory rate:
• Men: 15mmol/h
• Women: 12mmol/h
Rate found in pancreatic obstruction with enzyme
concentration.
[HCO3
-
] and enzymes associated with cystic fibrosis, chronic
pancreatitis, pancreatic cysts, calcification & edema of
the pancreas.](https://image.slidesharecdn.com/gastricfunctiontest-160911172756/75/Gastric-and-Pancreatic-function-tests-34-2048.jpg)