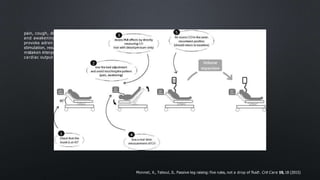
1) The document discusses various echocardiography techniques to assess fluid responsiveness in critically ill patients, including measuring changes in stroke volume, velocity time integral, and inferior vena cava diameter and collapsibility in response to passive leg raises or mini-fluid boluses.
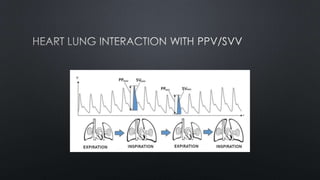
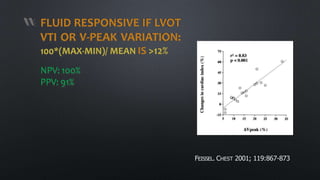
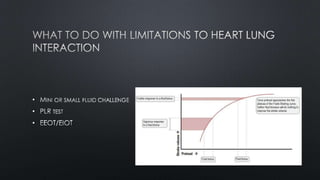
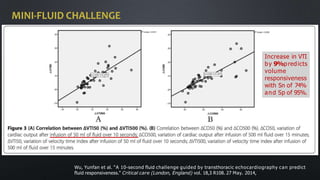
2) Key techniques mentioned are measuring stroke volume variation (SVV) or pulse pressure variation (PPV), which can predict fluid responsiveness if above 12%, and observing changes in velocity time integral during end-expiratory and end-inspiratory occlusion tests, with a change over 13% predicting a fluid response.
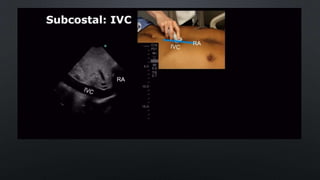
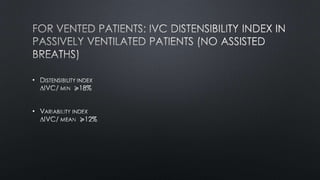
3) Measuring inferior vena cava collapsibility or distensibility is also discussed, with values