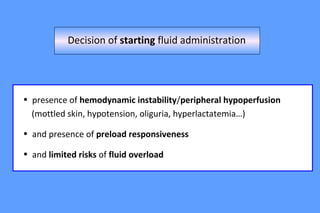
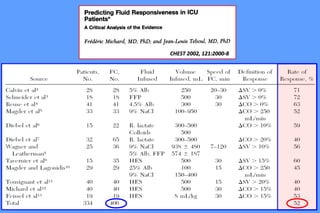
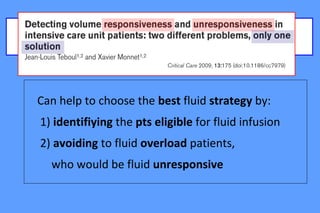
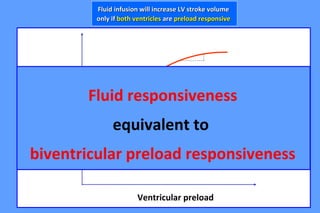
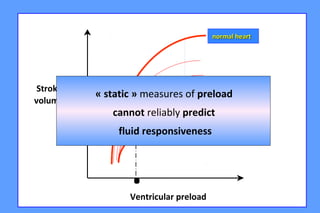
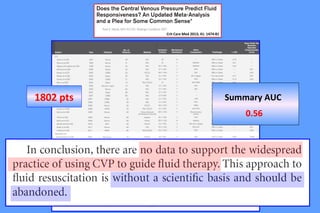
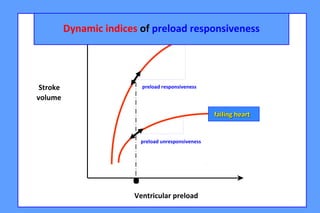
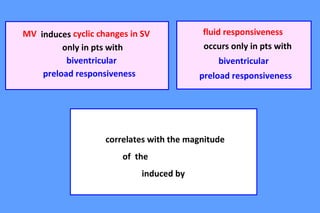
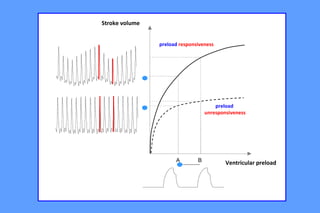
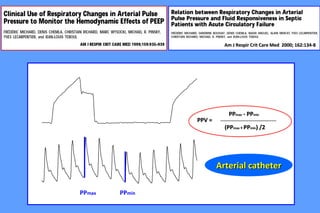
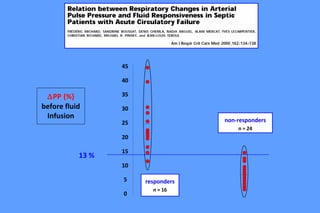
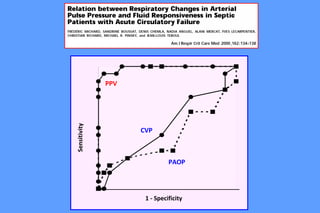
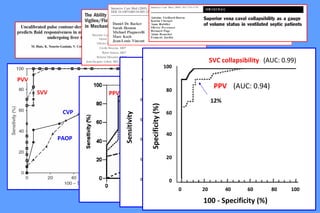
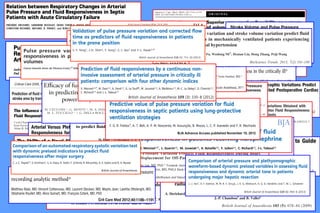
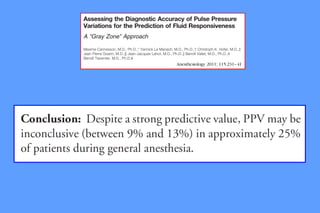
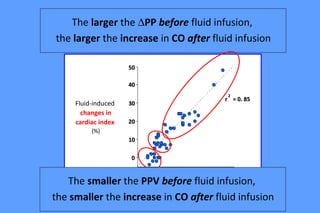
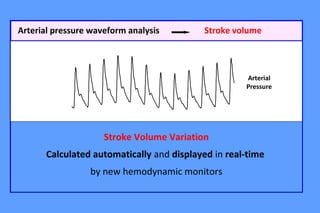
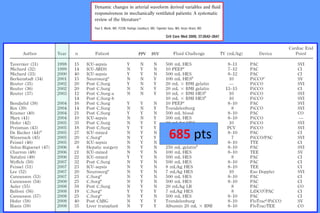
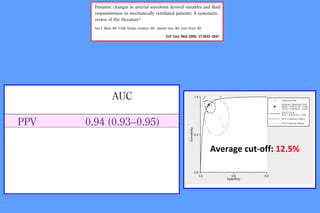
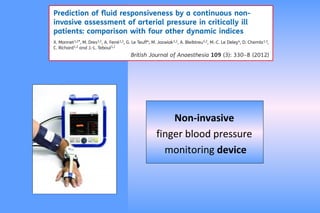
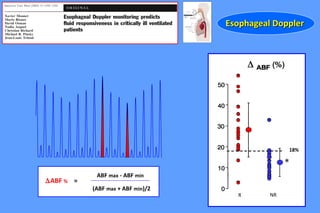
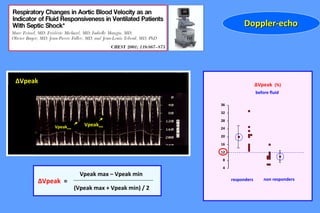
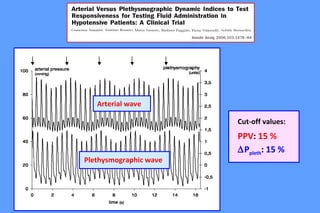
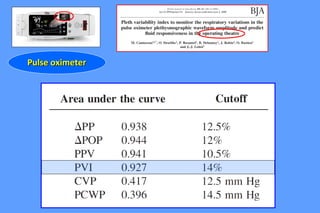
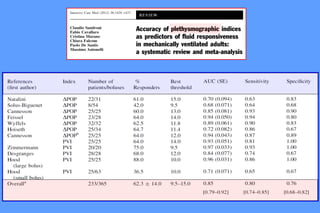
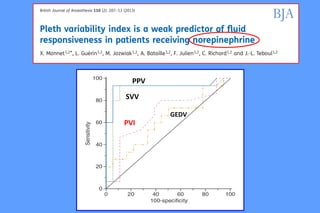
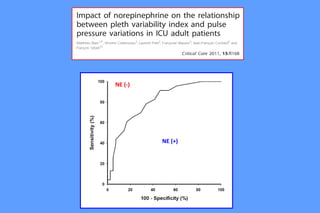
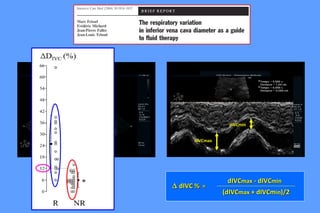
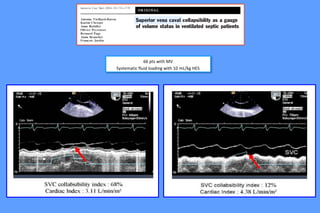
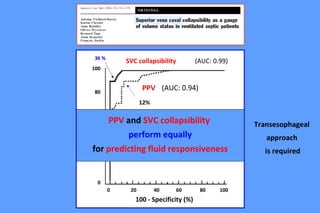
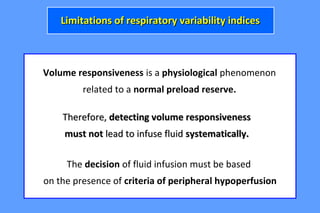
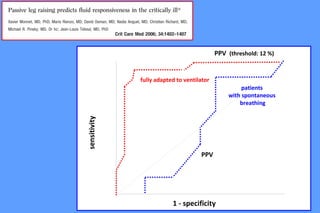
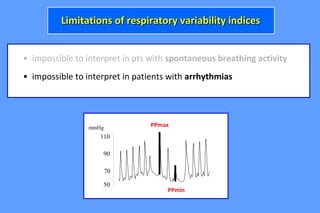
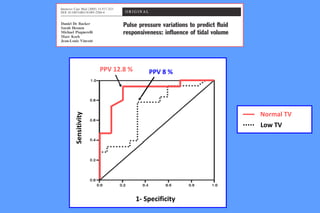
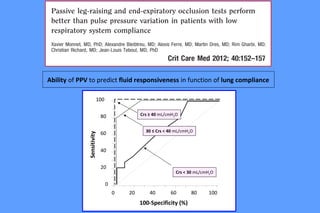
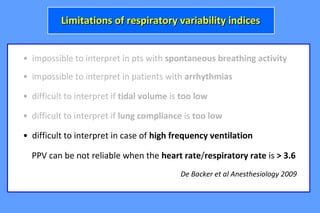
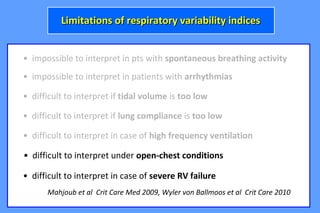
This document discusses fluid responsiveness and methods for assessing preload responsiveness. It summarizes that dynamic indices of preload responsiveness like pulse pressure variation (PPV) and stroke volume variation (SVV) can help identify patients who will respond to fluid by increasing their stroke volume. However, these indices have limitations and may not be reliable in patients with spontaneous breathing, arrhythmias, low tidal volumes, low lung compliance, high frequency ventilation, open chest conditions, or severe right ventricular failure. In these situations where the indices cannot be interpreted reliably, other dynamic tests are needed to assess fluid responsiveness.