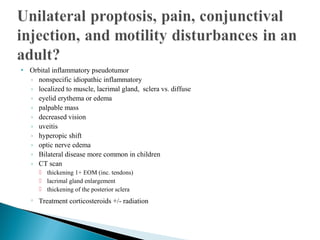
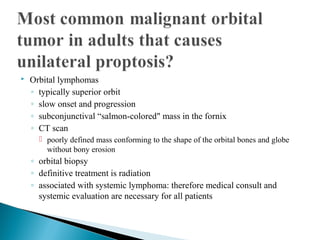
This document discusses various causes of proptosis (forward protrusion of the eyeball), including thyroid eye disease, orbital inflammatory pseudotumor, infectious orbital cellulitis, optic nerve glioma, rhabdomyosarcoma, cavernous hemangioma, and orbital lymphomas. For each condition, it provides details on symptoms, diagnostic tools such as CT scans, characteristic findings, treatment options, and importance of systemic evaluation. Thyroid eye disease and orbital inflammatory pseudotumor are highlighted as common causes of bilateral proptosis, while rhabdomyosarcoma has the highest mortality risk if untreated and spreads beyond the orbit.