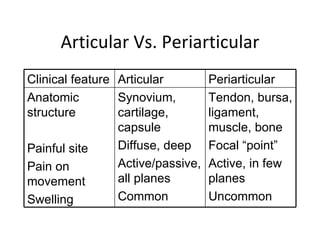
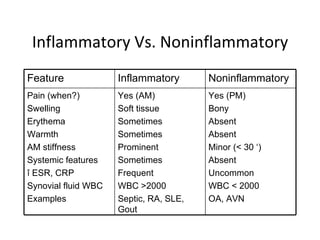
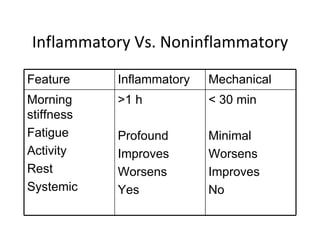
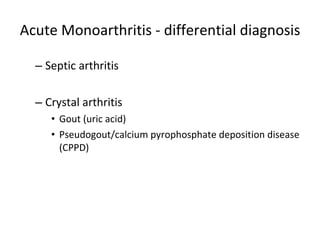
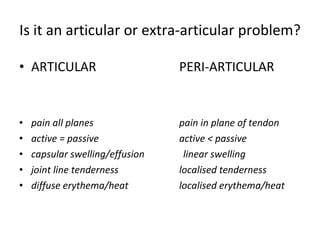
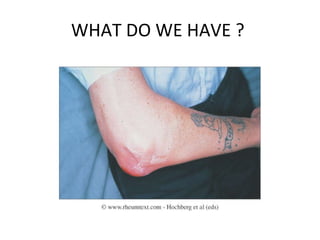
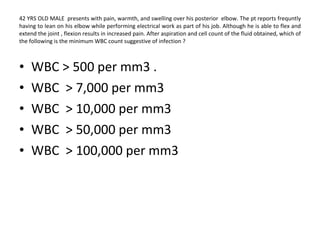
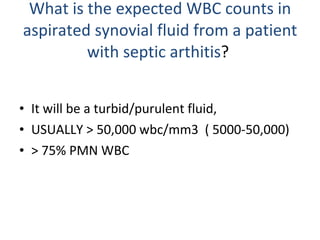
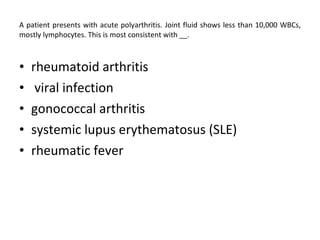
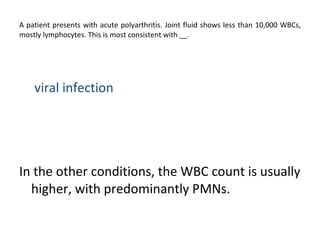
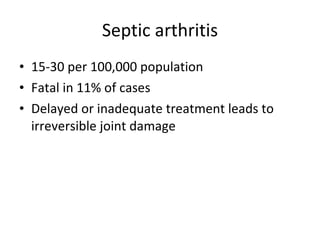
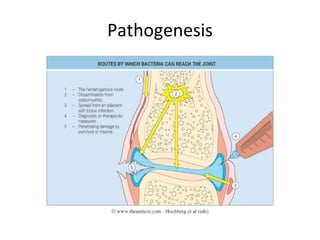
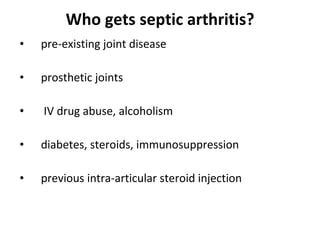
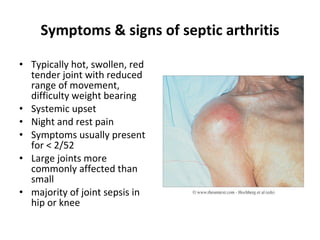
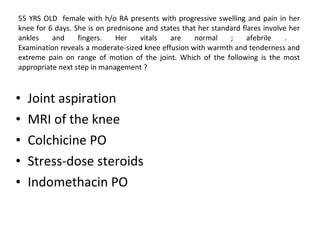
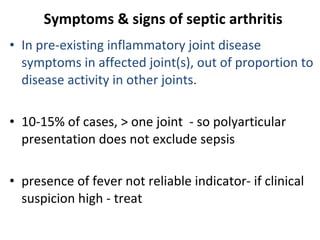
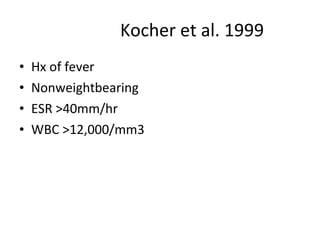
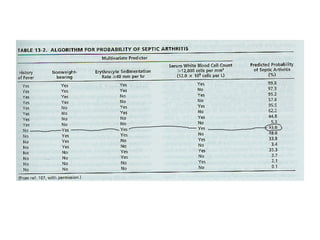
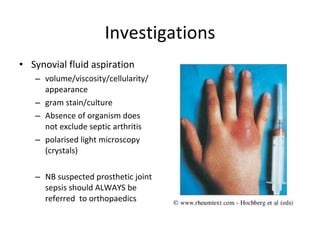
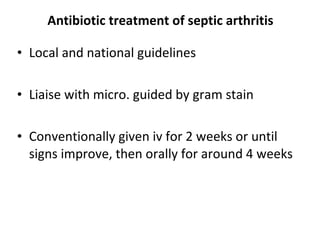
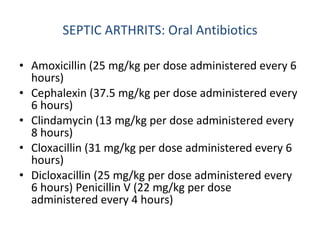
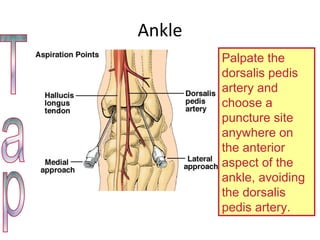
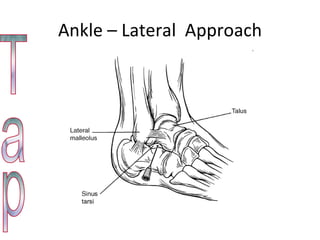
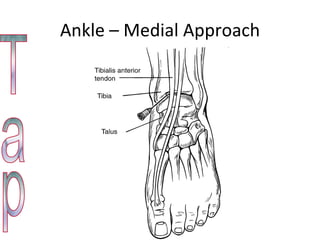
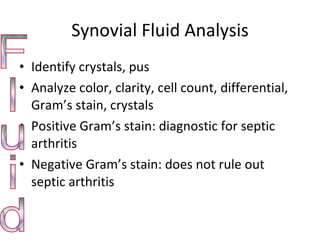
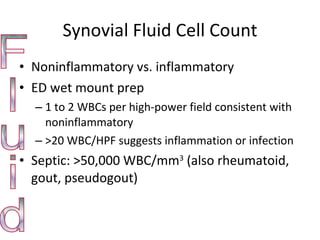
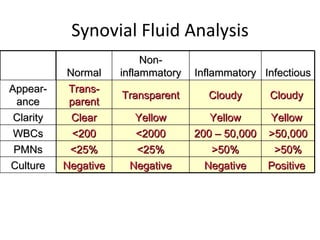
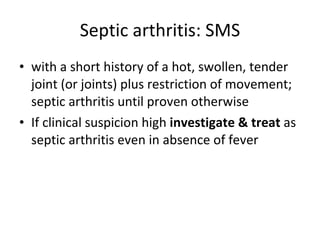
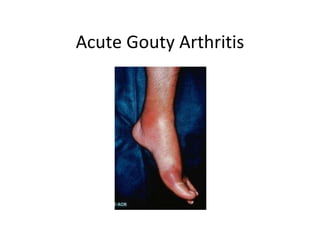
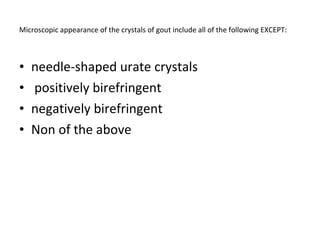
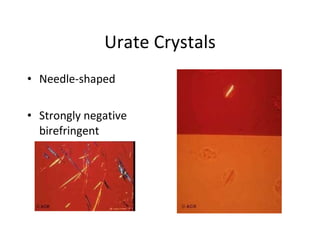
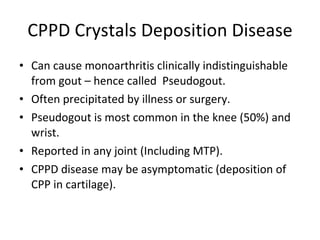
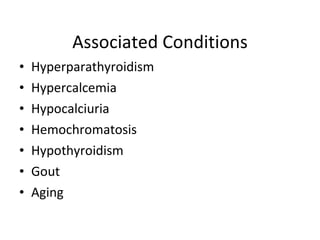
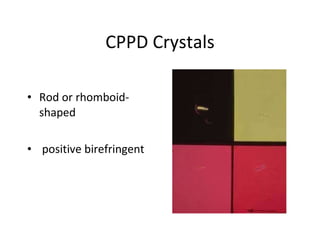
The document summarizes different types of arthritis including septic arthritis, gout, and crystal induced arthritis. It discusses the clinical features that distinguish articular from periarticular involvement as well as inflammatory from non-inflammatory arthritis. Diagnostic testing of synovial fluid such as cell count and microscopy for crystals is emphasized. Treatment of conditions like septic arthritis with antibiotics is outlined.