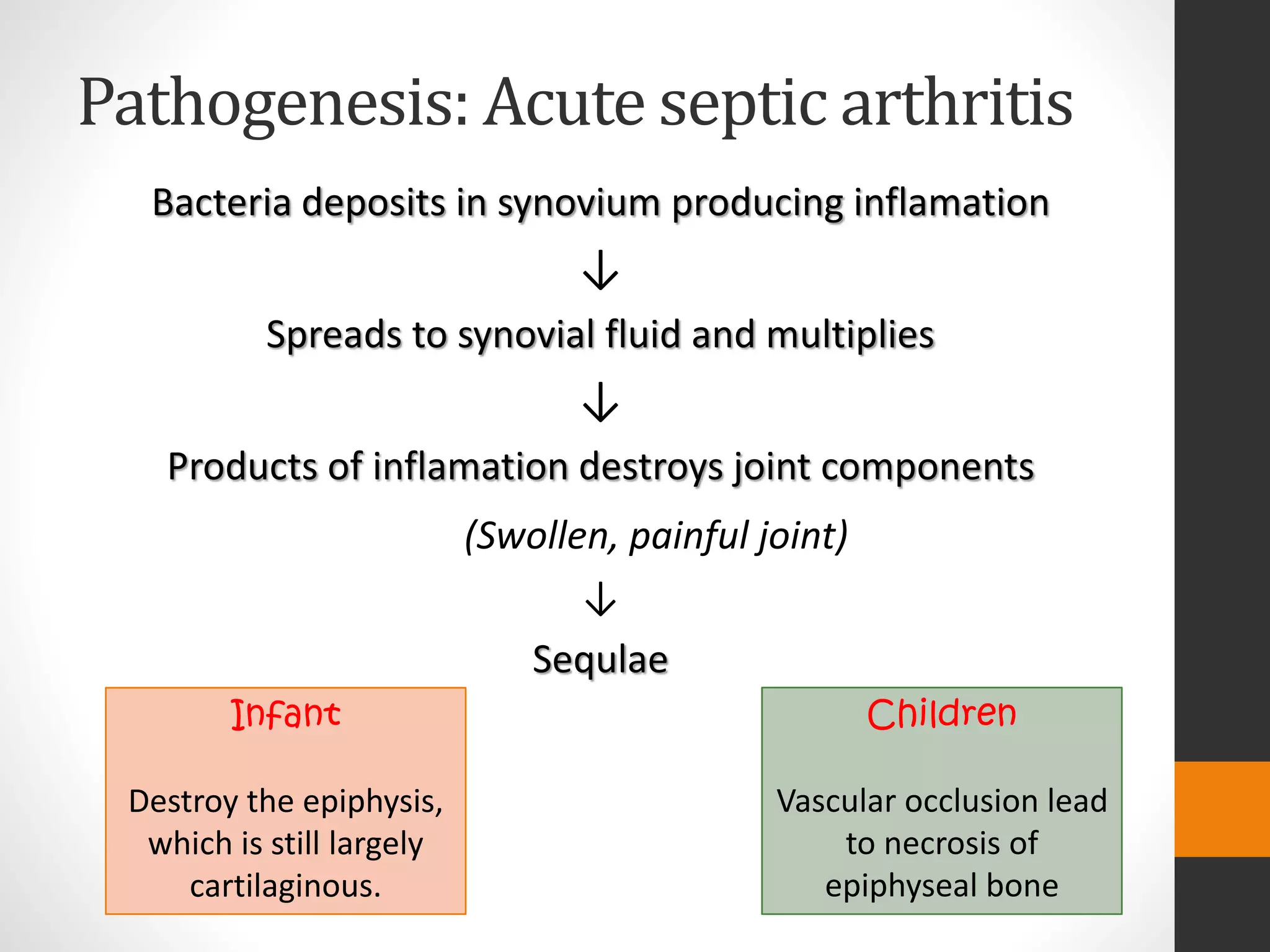
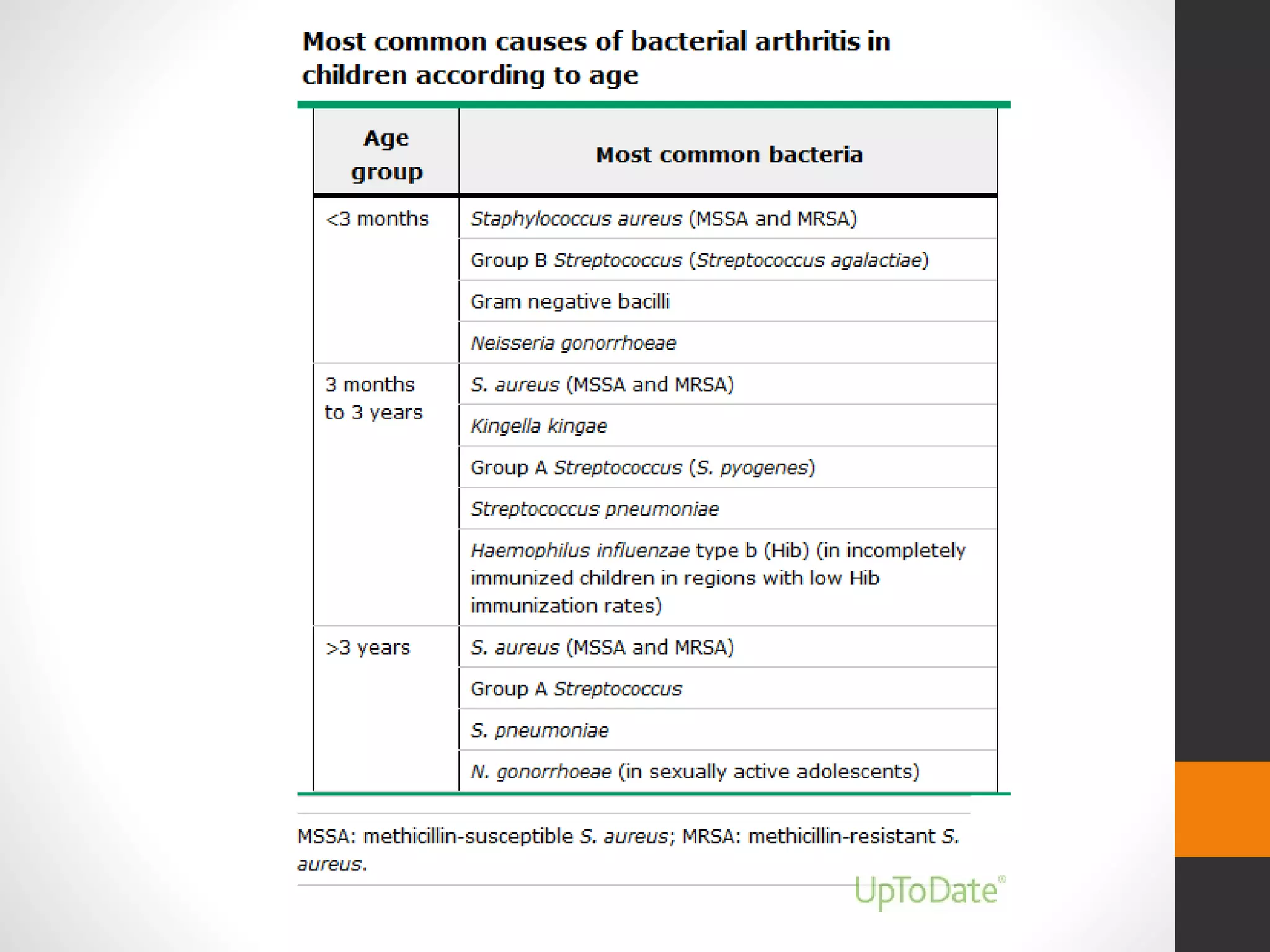
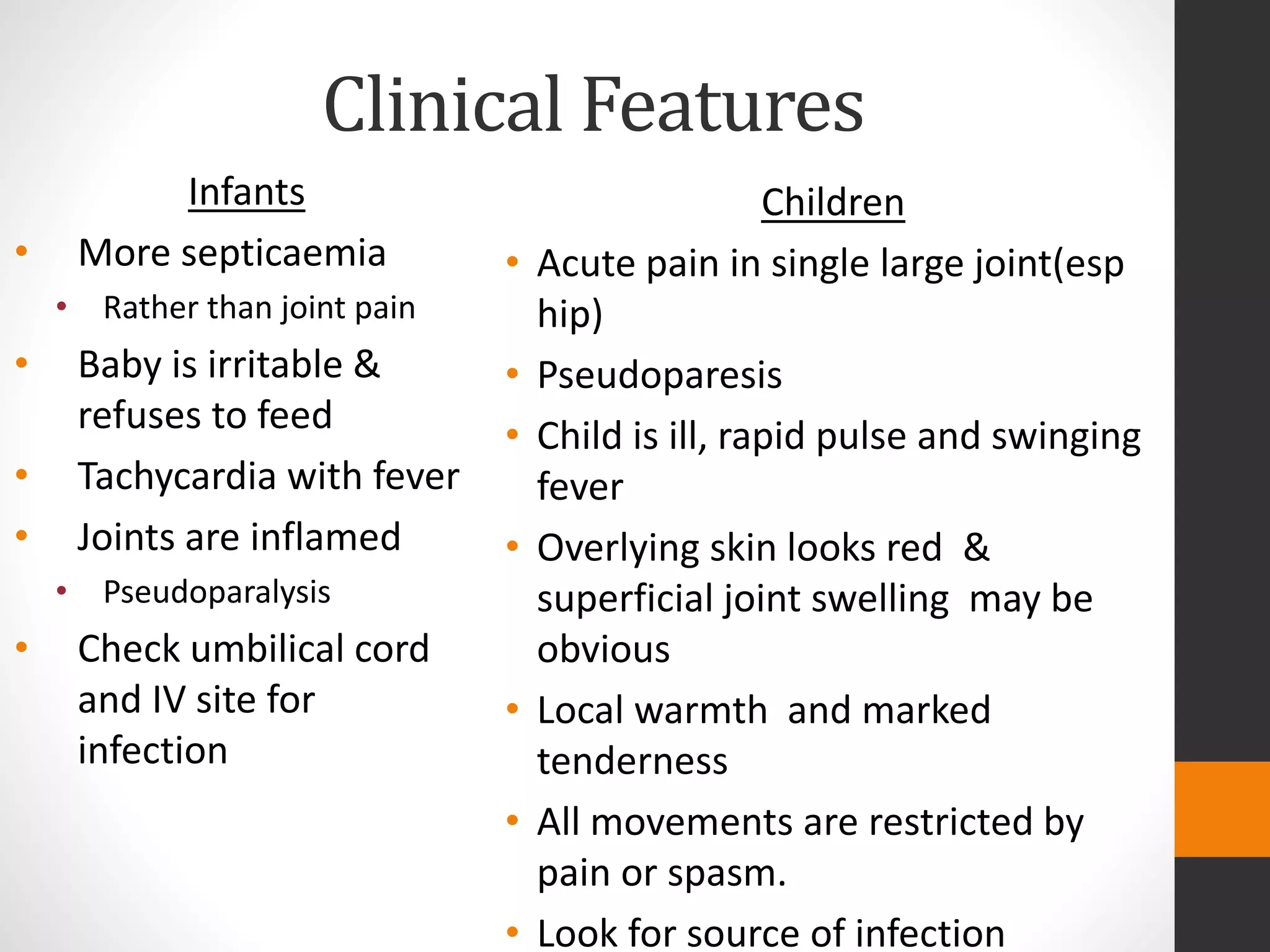
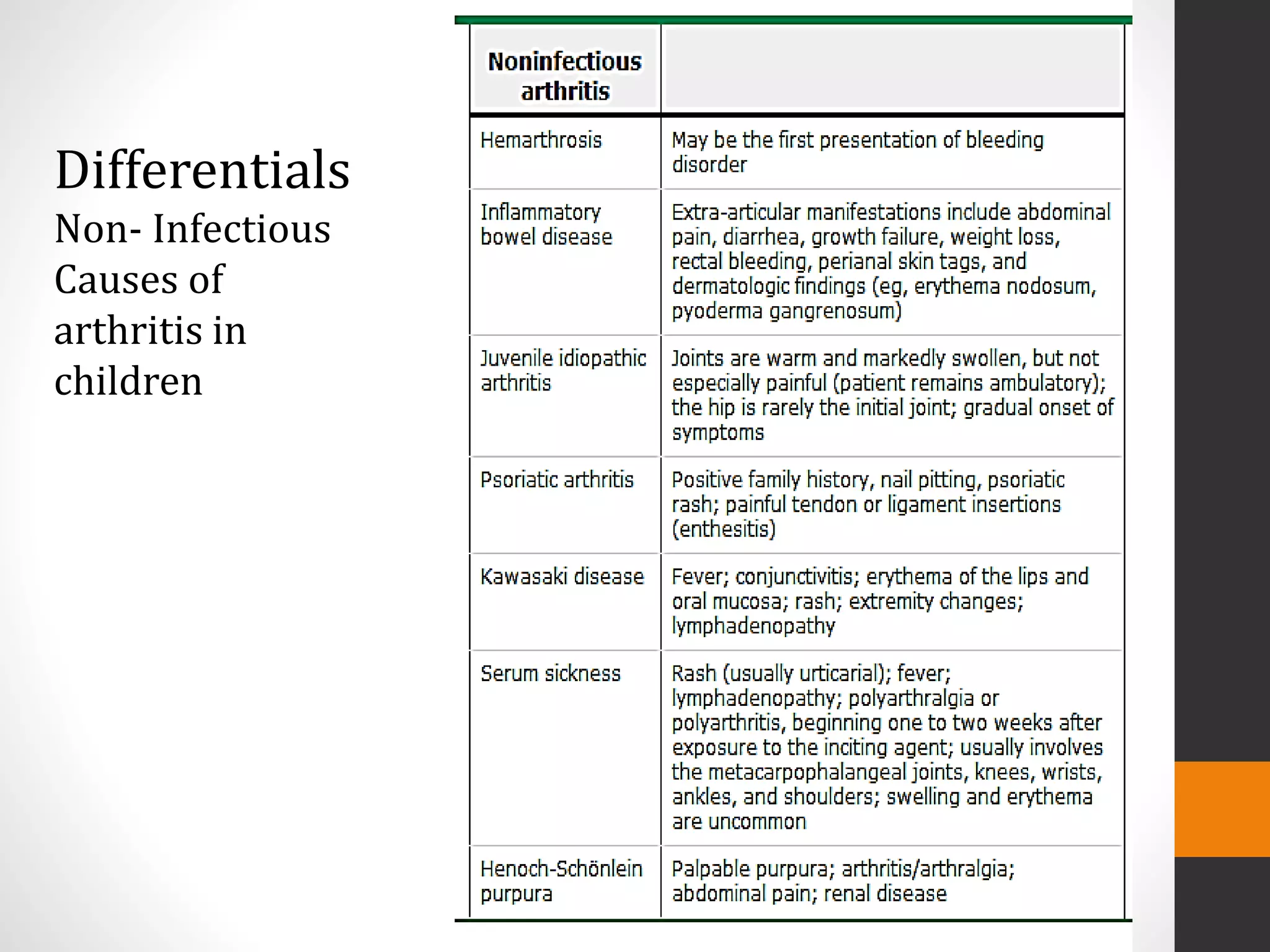
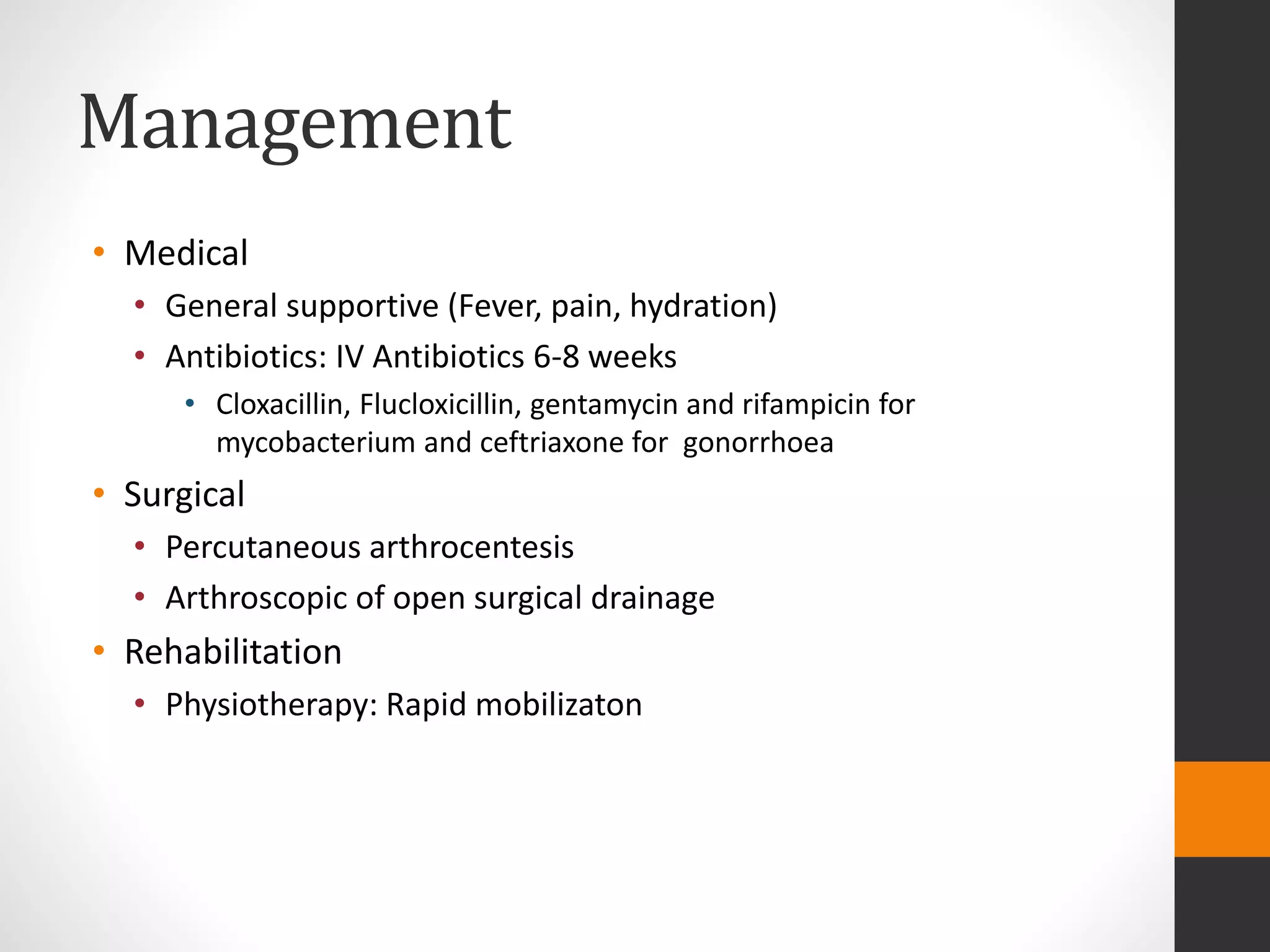
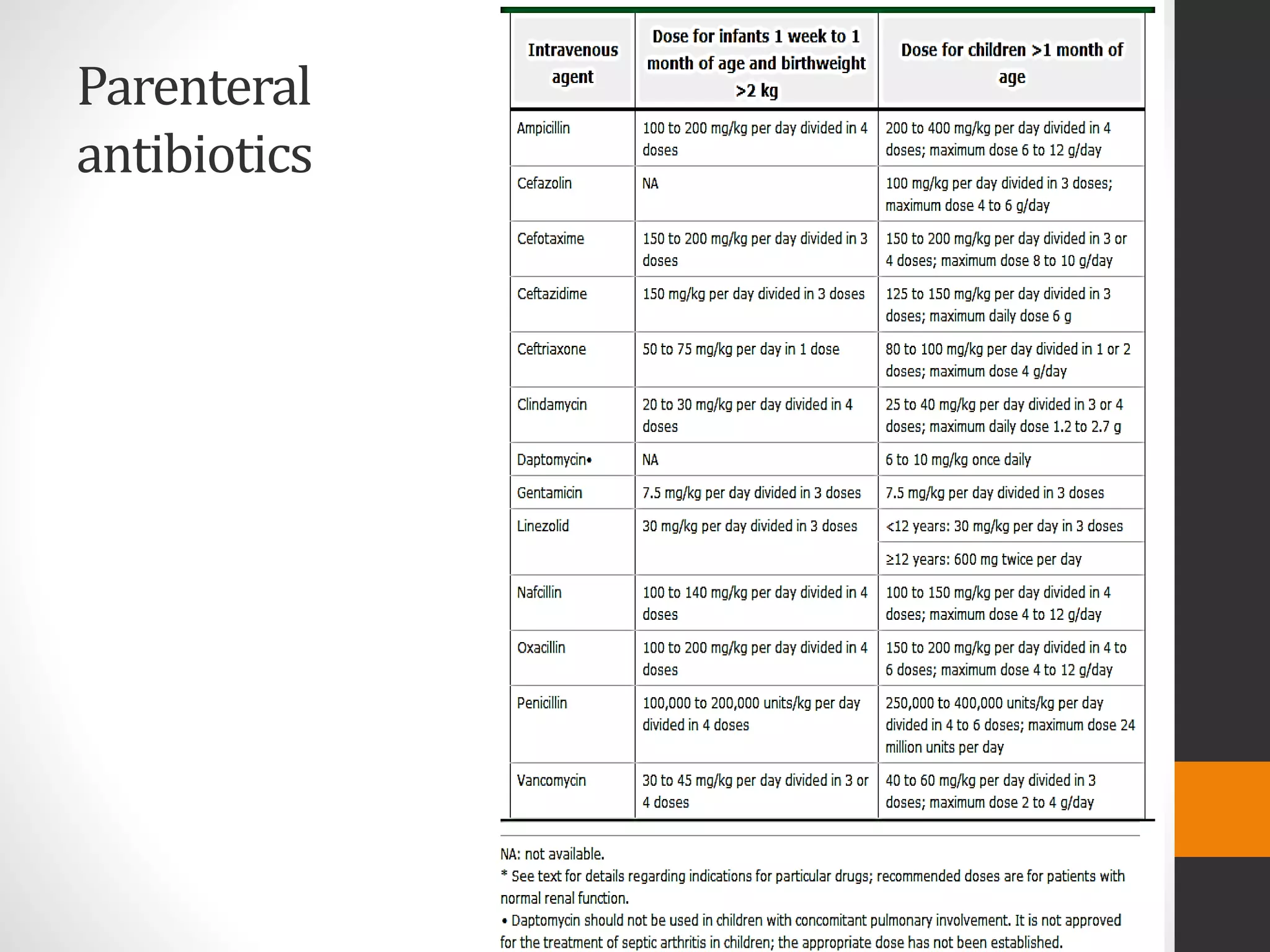
Paediatric septic arthritis is an infection of the joint space, most commonly caused by bacteria entering through the bloodstream. It can lead to destruction of joint components if not treated promptly. The diagnosis involves examining the affected joint for swelling, warmth and limited range of motion, as well as blood tests and imaging. Treatment consists of intravenous antibiotics for 6-8 weeks alongside surgical drainage and physiotherapy, with the aim of preventing long-term joint damage. Proper follow-up is important to monitor a child's development.