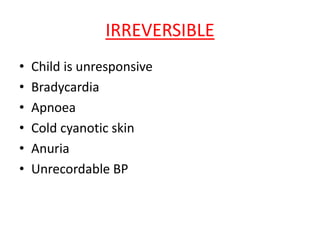
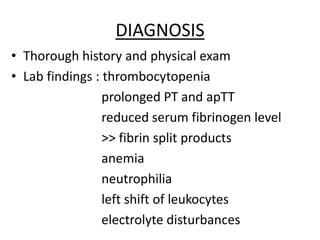
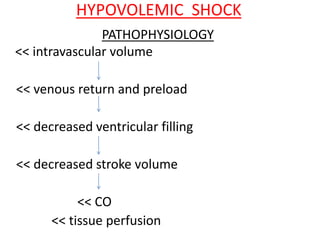
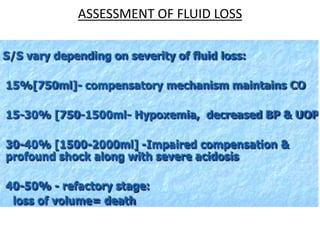
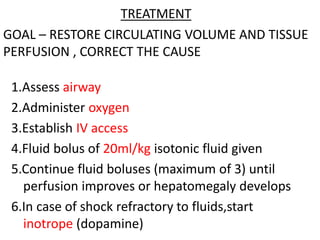
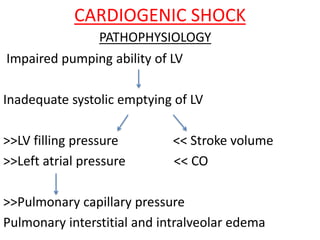
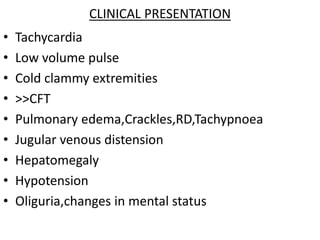
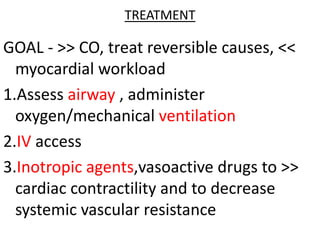
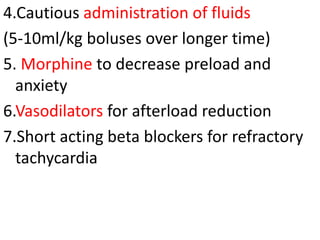
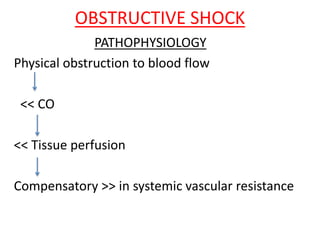
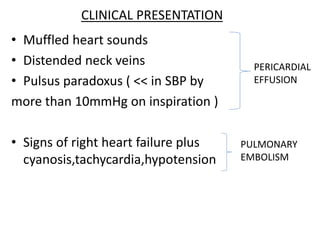
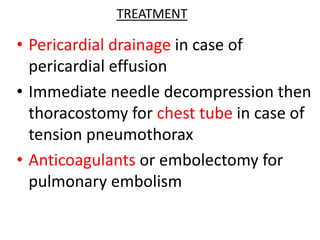
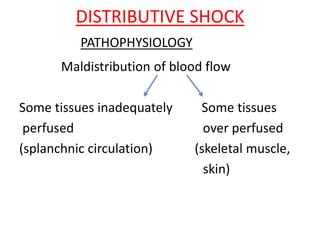
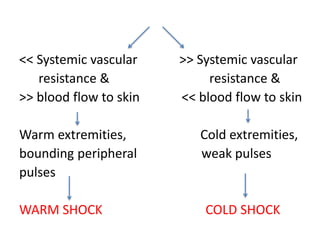
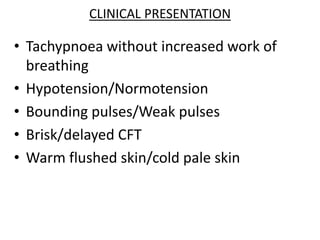
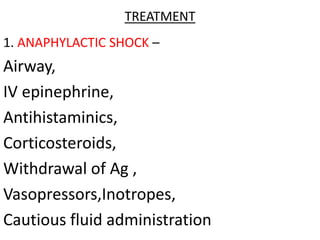
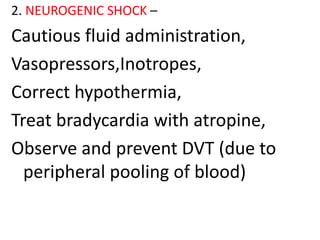
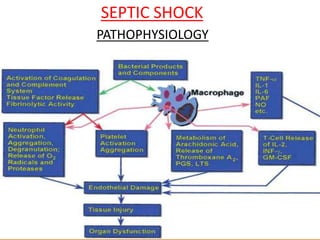
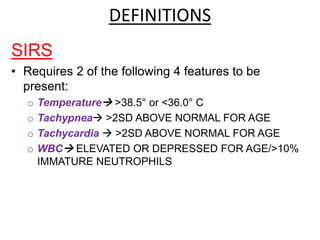
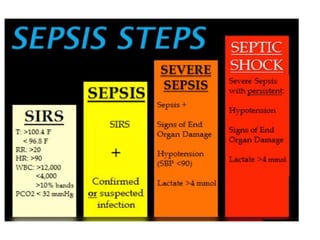
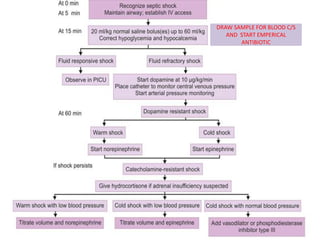
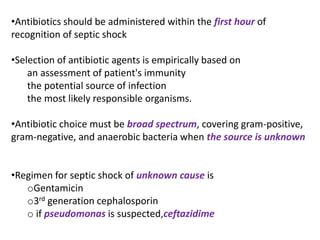
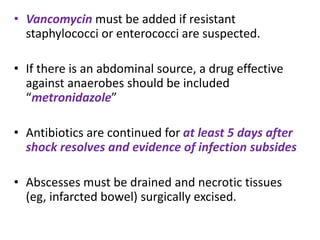
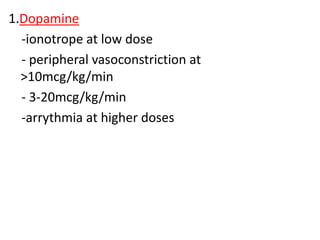
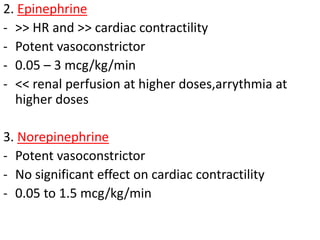
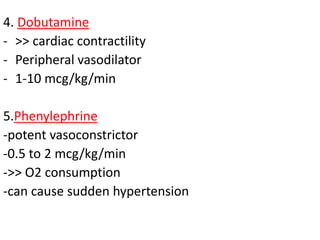
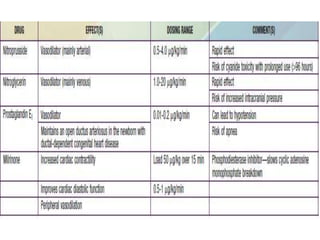
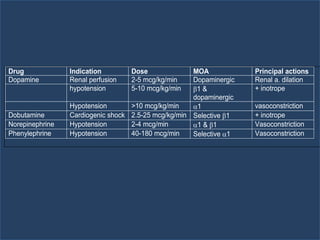
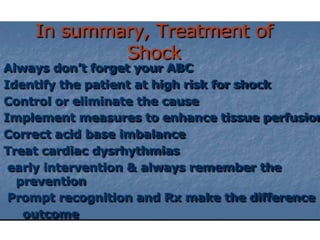
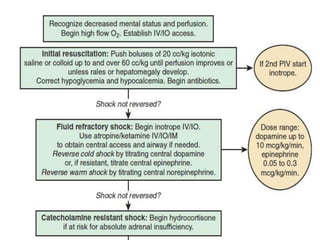
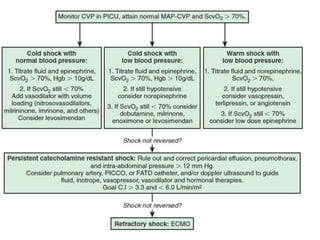
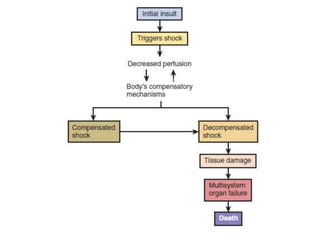
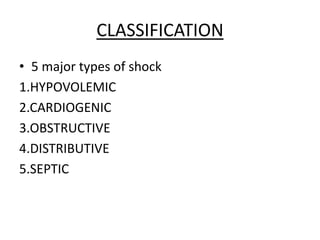
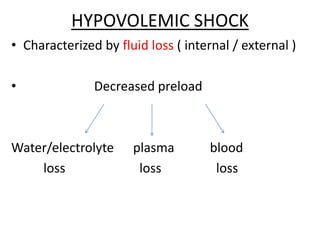
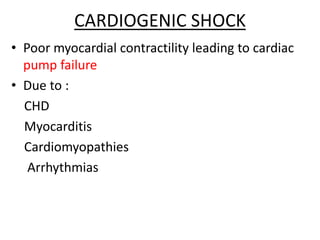
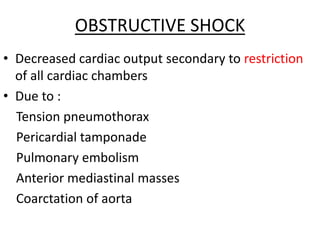
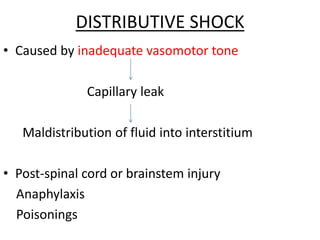
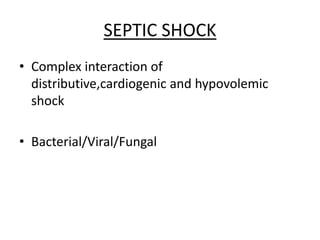
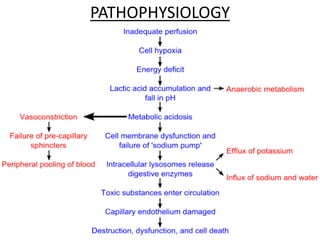
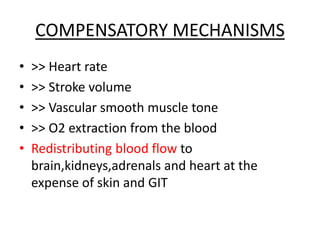
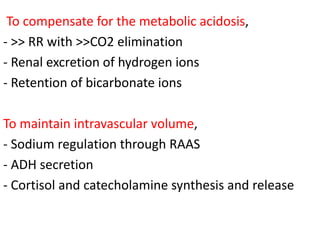
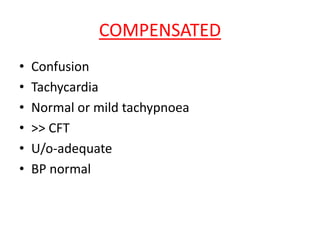
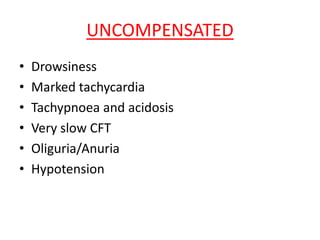
The document discusses various types of shock in children, encompassing five major classifications: hypovolemic, cardiogenic, obstructive, distributive, and septic shock. It details the pathophysiology, clinical manifestations, diagnosis, and treatment strategies for each type of shock. Key management steps are outlined, including fluid resuscitation, medication administration, and the importance of identifying and addressing underlying causes.
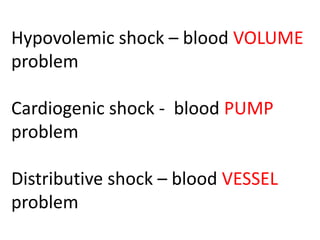
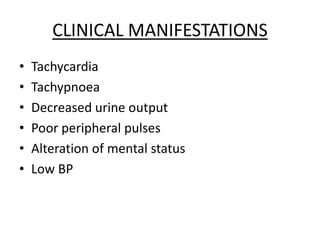
![HYPOTENSION FORMULA
Ages – 1 to 10 years
Hypotension is defined as SBP
< 70mmHg + [age in years X 2] mmHg](https://image.slidesharecdn.com/shockappu-141222090125-conversion-gate01/85/Shock-in-children-18-320.jpg)