Bone and joint infection in children
- 1. Bone And Joint Infection In Children Dr Sunil Agrawal, 1st year , MD Resident- Pediatrics
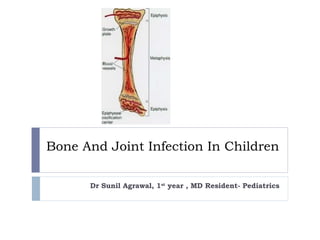
- 2. Introduction Bone infections in children are relatively common and important because of their potential to cause permanent disability. Early recognition and prompt institution of appropriate medical and surgical therapy minimize permanent damage. The risk is greatest if the physis (the growth plate of bone) is damaged.
- 5. Content- 1.Osteomyelitis 2.Septic arthritis • Causative Organism • Epidemiology • Pathogenesis • Clinical Feature • Diagnosis • Lab Findings • Imaging • Treatment • Complications • Prognosis
- 6. Data of TUTH Septic Arthritis Osteomyelitis Male Female Male Female Neonate 0 1 0 0 <5 years 5 2 4 0 >5 years 3 1 3 1 Adolocent 2 0 4 0 Total 10 4 11 1 Total Admission: 26 Males: 21 Females: 5
- 7. Etiology of Osteomyelitis and Septic Arthritis Infant 0-2 months Staphylococcus aureus Streptococcus agalactiae Gram-negative enteric bacteria Candida <5 y Staphylococcus aureus Streptococcus pyogenes Streptococcus pneumoniae Kingella kingae Haemophilus influenzae type b >5 y S. aureus S. Pyogenes Adolescent Neisseria gonorrhoeae
- 8. Epidemiology The median age 6 yr.∼ Incidence = 1:5,000 Boys > Girls No predilection for any Race (Except Sickle cell disease – Blacks) In Previously healthy children- mostly hematogenous. Minor closed trauma - common preceding event ( 30% cases)∼ Infection of bones can follow penetrating injuries or open fractures. Following orthopedic surgery. Impaired host defenses increases the risk of skeletal infection.
- 9. MOST COMMON CLINICAL ASSOCIATION MICROORGANISM Frequent microorganism in any type of osteomyelitis Staph. aureus Common in nosocomial infection Enterobacteriaceae, Pseudomonas aeruginosa, candida spp. Foreign body–associated infection Coagulase-negative staphylococci or other skin flora, atypical mycobacteria Decubitus ulcers Streptococci and/or anaerobic bacteria Populations in which tuberculosis is prevalent Mycobacterium tuberculosis Exposure to kittens Bartonella henselae Immunocompromised patients Aspergillus spp., Candida albicans, or Mycobacteria spp. Microorganisms Isolated fromPatients with Osteomyelitis
- 10. Pathogenesis In the metaphysis, nutrient arteries branch into non-anastomosing capillaries under the physis make a sharp loop before entering venous sinusoids draining into the marrow ( Hair-pin Ends) Blood flow, sluggish and provides an ideal environment for bacterial seeding Relative paucity of phagocytic cells in this area
- 11. Pathogenesis- In neonates and young infants Transphyseal blood vessels connect the metaphysis and epiphysis commonly pus from the metaphysis enters the joint space Result in abnormal growth and bone or joint deformity Joint involvement takes place when the metaphysis is intra- articular as in hip, ankle, shoulder, and elbow joint or when subperiosteal pus ruptures into the joint space
- 12. Pathogenesis- In child >18 months age Spread through the cortex. Porous metaphyseal cortex provides easy assess for the exit of exuate or pus Elevates the periosteum (thick periosteum loosly adherent to the cortex) Subperiosteal pus collection(further impairing blood supply to the cortex and metaphysis) Enough periosteal destruction soft tissue abcess.→
- 13. Pathogenesis…In later childhood and adolescence The growth plate closes, hematogenous osteomyelitis more often begins in the diaphysis and can spread to the entire intramedullary canal. Closed plate is relativley resistant to spread of infection. The periosteum becomes more adherent, favoring pus to decompress through the periosteum The fluid formed seeks the path of least resistance from the metaphysis
- 14. Clinical Features Age - greater in infants and toddlers than in older children Sex - boys > girls, usually 2 : 1 Signs and symptoms are highly dependent on the age of the patient The initial s/s are often subtle The hallmark of osteomyelitis is fever plus localised bony tenderness Neonates may exhibit pseudoparalysis or pain with movement of the affected extremity- Diaper changes Half of neonates do not have fever and may not appear ill
- 15. Clinical Features… Signs and symptoms Older infants and children are more likely to have fever, pain, and localizing signs such as edema, erythema, and warmth With involvement of the lower extremities, limp or refusal to walk Careful Physical examination may reveal focal bony tenderness.
- 16. Distribution of Affected Bones in Acute Hematogenous Osteomyelitis • Usually only a single site of bone or joint involvement, the exception is osteomyelitis in neonates. • Several bones are infected in <10% of cases; BONE % Femur 23-28 Tibia 20-24 Humerus 5-13 Radius 5-6 Phalanx 3-5 Pelvis 4-8 Calcaneus 4-8 Ulna 4-8 Metatarsal ∼2 Vertebrae ∼2 Sacrum ∼2 Clavicle ∼2 Skull ∼1
- 17. Diagnosis Children with acute bone pain and systemic signs of sepsis should be considered to have acute hematogenous Osteomyelitis until proved otherwise. Diagnosis may be established if a patient fulfills two of the following criteria: 1. Bone aspiration yield pus 2. Bacterial culture of bone or blood positive 3. Presence of the classical s/s of acute osteomyelitis 4. Radiographic changes typical for osteomyelitis.
- 18. LABORATORY FINDINGS No specific laboratory tests. Elevations in peripheral WBC, ESR, and CRP – ESR-Nonspecific acute phase reactant Increased 48-72 hrs Increased in 90% of cases Not affected by antibiotic tx CRP- Increased in 98% of cases Blood culture- Positive in 30-50% Decreased with antibiotic 48 hours to get most organisms
- 19. Radiology Plain xray Sensitivity 43-75% Specificity 75-83% Soft tissue swelling 48hrs Periosteal reaction 5-7days Osteolysis 7-14 days of infection(need 30-50% bone loss) Magnetic Rsonance Imaging (MRI) Computed Tomography (CT) Radionuclide Study
- 20. Plain radiography Bone changes - not seen for at least 10-14 days after the onset of infection. • Plain radiographs-normal in the first 7 to 10 days • Soft tissue swelling with loss of the normal soft tissue planes is seen before bone changes become apparent •Periosteal elevation or thickening - new bone formation, pus, or reactive edema from adjacent soft tissue infection
- 24. Brodie’s abscess, central oval lucency surrounded By reactive sclerosis usually within or close to the Metaphysis and the lesion may extend across the physis.
- 26. Garré sclerosing osteomyelitis, or chronic nonsuppurative sclerosing osteomyelitis, is a form of chronic osteomyelitis. Mild inflammation and infection lead to subperiosteal bone deposition. It is frequently asymptomatic. The characteristic radiographic appearance is an area of periosteal proliferation surrounded by successive layers of condensed cortical bone (arrows), described as an onion skin appearance.
- 27. Radionuclide imaging… Radionuclide imaging can be valuable in suspected bone infections especially if multiple foci are suspected Bone scans in acute haematogenous osteomyelitis have a sensitivity of 84% to 100% and a specificity of 40% to 96%. (N Susan Stott, Journal of Orthopaedic Surgery; Review article: Paediatric bone and joint infection) Can detect osteomyelitis within 24–48 hr after onset of symptoms The sensitivity in neonates is much lower owing to poor bone mineralization
- 28. A) Plain radiographs of the ankle demonstrate deep soft tissue swelling inferior to the medial malleolus. B) A technetium 99m bone scan shows increased uptake in the distal tibia in the blood flow and bone uptake (four hour) phases. Early Osteomyelitis, with pain and fever Bone Scan… Tc99 24-48hrs +ve Decreased uptake in early phase d/t increased pressure
- 29. Ultrasound can detect features of osteomyelitis several days earlier Xray (predominately in children). Acute osteomyelitis is recognized by elevation of the periosteum by a hypoechoic layer Soft tissue abscesses related to chronic osteomyelitis are identified as hypoechoic or anechoic fluid collections, which may extend around the bony contours. Finally, cortical erosions can become apparent on US MRI have comparable positive predictive value to radionuclide imaging in acute osteomyelitis particularly useful in the evaluation of vertebral osteomyelitis and diskitis
- 32. Bone Aspiration A bacteriologic diagnosis is made by culturing the involved bone or pus, once a clinical diagnosis of acute osteomyelitis is established. Useful to determine whether an abscess is present. The organism detection rate is increased to 75% to 80% by aspiration of the affected bone K. kingae may need to be identified by polymerase chain reaction Also useful in determining the future course of therapy of the child
- 33. Differential Diagnosis Trauma Cellulitis Myositis and pyomyositis Leukemia Neuroblastoma with bone involvement Primary bone tumors (Ewing sarcoma) Septic arthritis
- 34. Classification- Acute hematogenous Osteomyelitis Subacute hematogenous Osteomyelitis Chronic Multifocal Osteomyelitis Parameters Subacute Acute WBC Frequently normal Frequently elevated ESR Frequently elevated Frequently elevated Blood Cultures Rarely Positive 50% Positive Bone Cultures 60% Positive 90% Positive Localization Diaphysis, metaphysis, epiphysis, cross physis Metaphysis Pain Mild to Moderate Severe Systemic Illness No Fever, malaise Loss of function No or minimal Marked Prior antibiotics 30%-40% Occasional Initial radiograph Frequently abnormal Bone normal
- 35. Treatment Acute Osteomyelitis Collaborative efforts of pediatricians, orthopedic surgeons, and radiologists Medical and surgical treatment Antibiotics Emperical Antibiotics, Antistaphylococcal agent (Methicillin sensitive Staphylococcus aureus is still the most common organism although the incidence of methicillin resistant S. aureus in the community is rising)
- 36. Treatment Antibiotics In NEONATES -I.V antibiotics Oxacillin or nafcillin (150 – 200 mg/kg/24 hrs in q6h IV) + BSA like Cephotaxime (150-225 mg/kg/24 hr divided q8h IV) provide coverage for the S. aureus, group B streptococcus, and gram- negative bacilli. If MRSA suspected vancomycin is substituted for nafcillin In Neonate with Central Line , the possibility of nosocomial bacteria (Pseudomonas) or fungi (Candida) In older infants and children, the principal pathogens - S. aureus and streptococcus. Adjust according to culture reports.
- 37. If MRSA accounts for ≥10% of community S. aureus isolates, Vancomycin - gold standard agent – especially in critically ill. Clindamycin (30-40 mg/kg/day q8hr - resistance is ≤10% among community S. aureus isolates and the child is not severely ill. Cefazolin or nafcillin for MSSA. Penicillin is first-line therapy -S. pneumoniae, group A streptococcus. Cefotaxime or ceftriaxone is recommended for Resistant Pneumococci or Salmonella spp
- 38. Treatment… In special situations like SCD a broad-spectrum cephalosporin such as cefotaxime is used in addition to an antistaphylococcal drug For immunocompromised patients, Combination therapy, such as with vancomycin and ceftazidime, or with piperacillin-clavulanate and an aminoglycoside Supportive treatment Rest Immobilization of affected limb
- 39. IV to Oral Changing antibiotics from the IV route to oral administration when a patient's condition clearly has improved and the child is afebrile for ≥48-72 hr, may be considered. -lactam drugs for susceptible staphylococcal or streptococcalβ infection cephalexin Oral clindamycin in clindamycin-susceptible CA-MRSA or for patients who are seriously allergic or cannot tolerate -lactamβ antibiotics.
- 40. Duration of antibiotic therapy Most infections- eg S. aureus, minimal duration is 21-28 days, if prompt resolution of signs and symptoms (within 5-7 days) and the CRP and ESR have normalized; a total of 4-6 wk of therapy may be required. For group A streptococcus, S. pneumoniae, or H. influenzae type b, treatment duration maybe shorter. A total of 7-10 postoperative days of treatment is adequate for Pseudomonas osteochondritis when thorough curettage of infected tissue has been performed. Immunocompromised patients, mycobacterial or fungal infection -require prolonged courses of therapy.
- 41. Indication of Surgical Treatment Abscess collection (Subperiosteal , soft tissue, or intramedullary) Patient is not responding to appropriate antibiotic therapy after a negative bone aspiration (If a child with acute hematogenous osteomyelitis does not show symptomatic improvement with decrease in swelling and tenderness after 36-48 hrs of appropriate antibiotic treatment, the bone should be aspirated again and consideration given to surgical drainage) In subacute Osteomyelitis when debridement is necessary (granulation tissue within the cavity even though no pus) Radiographic lesion, sequestrum
- 42. Complications Bone abscess Bacteremia Fracture Loosening of the prosthetic implant Overlying soft-tissue cellulitis Draining soft-tissue sinus tracts Growth disturbance
- 43. Prognosis Improvement in signs and symptoms is rapid when timely intervened. Failure to improve or worsening by 72 hr requires review of antibiotic therapy, the need for surgical intervention, or the correctness of the diagnosis. Recurrence of disease and development of chronic infection after treatment occur in <10% of patients.
- 44. Septic Arthritis An infection of a synovial joint which may occur in all age groups in children Has a specific infantile form affecting the infant from birth to the first year of life Relatively uncommon
- 45. Septic Arthritis More common in infants and toddlers than in older children Half of all cases occur by 2 yr of age and three fourths of all cases occur by 5 yr of age Immuno-compromised hosts may have a higher incidence
- 46. Pathogenesis Results from hematogenous seeding of the synovial space Organisms enter the joint space by direct inoculation or extension from a contiguous focus. The synovial membrane (rich vascular supply and lacks a basement membrane) providing an ideal environment for hematogenous seeding. Cytokines stimulate chemotaxis of neutrophils into the joint space, proteolytic enzymes and elastases are released by neutrophils cartilage damage Increased pressure in joint space from can compromise the vascular supply and induce pressure necrosis of the cartilage.
- 47. Pathogenesis…. May be associated with acute osteomyelitis esp in the proximal femur Routes of Infection- Usually hematogenous Trauma (penetrating injuries) Post procedure (arthroscopy, prosthetic joint surgery, intra- articular steroid injection, and orthopedic surgery)
- 48. Pathology Acute inflammatory reaction. Degradation of the articular cartilage begins within 8 hours of infection. In neonates, metaphyseal osteomyelitis is often associated with septic arthritis due to the presence of transphyseal blood vessels that disappear by age 6 to 12 months Sixty to 100% of neonates with septic arthritis will have adjacent osteomyelitis
- 49. CLINICAL MANIFESTATIONS Hot, swollen joint painful on any movement indicates a septic arthritis until proved otherwise In neonate, present as a pseudo-paralysis of one limb Erythema and edema of the skin and soft tissue overlying the site of infection are seen earlier in suppurative arthritis than in osteomyelitis Joint kept at position of ease.
- 50. Distribution of Affected Joints in Acute Suppurative Arthritis BONE % Knee ∼40 Hip 22-40 Ankle 4-13 Elbow 8-12 Wrist 1-4 Shoulder ∼3 Interphalangeal <1 Metatarsal <1 Sacroiliac <1 Acromioclavicular <1 Metacarpal <1 Toe ∼1
- 51. Investigations The investigations are similar to those required in osteomyelitis Blood culture Aspiration of the joint fluid for Gram stain and culture, definitive diagnostic technique and provides the optimal specimen for culture to confirm the diagnosis Elevations of WBCs, ESR, and CRP are very sensitive for joint infections but are nonspecific
- 52. Synovial fluid analysis – Cell Counts >50,000-100,000 cells/mm3 generally indicate an infectious process. Synovial fluid characteristics of septic arthritis can suggest infection but are not sufficiently specific to exclude infection. Infected Fluid Appearance / Clarity: Turbid to very turbid (N- Clear and colorless) Viscosity: Greatly reduced (similar to water) (N-Very viscous) Leukocytes / cubic cm: 15,000- >200,000 (N : Average 63; Range: 13-180.) usually >50,000 and >100,000 is virtually diagnostic Percent polymorphoneuclear: 50-100% (N-<25%) 90% almost always indicates infection Mucin clot: Poor to very poor (N-Good) Glucose level difference versus plasma: >40 mg/100ml less than plasma (N- Within 10 mg/100ml of plasma concentration)
- 53. Differential Diagnosis Depends on the joint or joints involved and the age of the patient Hip toxic synovitis, Legg-Calvé-Perthes disease, slipped capital femoral epiphysis, psoas abscess, and proximal femoral, pelvic, or vertebral osteomyelitis as well as diskitis Knee distal femoral or proximal tibial osteomyelitis, pauciarticular rheumatoid arthritis, and referred pain from the hip Others like trauma, cellulitis, pyomyositis, sickle cell disease, hemophilia, and Henoch-Schönlein purpura, also Reactive arthritis, Acute rheumatic fever (multiple joints involved)
- 54. Radiographic Evaluation Plain Xrays Widening of the joint capsule, soft-tissue edema, and obliteration of normal fat lines Ultrasonography helpful in identifying effusions in deep joints such as the hip may serve as an aid in performing hip aspiration CT MRI Both are useful in confirming the presence of joint fluid in patients with suspected osteoarthritis infections MRI may be useful in excluding adjacent osteomyelitis Radionuclide studies In suppurative arthritis, three-phase imaging with technetium-99 methylene diphosphonate shows symmetric uptake on both sides of the joint, limited to the bony structures adjacent to the joint
- 55. Treatment The infection should be considered an abscess that requires drainage for eradication of the infection Appropriate antibiotic therapy The dosase of antibiotics are same as for acute osteomyelitis The duration is shorter as antibiotics reach the infected joint readily and in high concentration Normalization of ESR and CRP in addition to a normal examination supports discontinuing antibiotic therapy Total length of treatment is generally 2-4 weeks
- 56. Hip joint An infection of the hip joint is an emergency, as potential for the development of avascular necrosis of the femoral head. Aspiratiion through Fluroscopy guided For joints other than the hip, daily aspirations of synovial fluid may be required • If fluid continues to accumulate after 4–5 days, arthrotomy is needed
- 57. APView of Left Hip showing avascularnecrosis left head of femur
- 58. Treatment Antibiotic Therapy: The initial empirical antibiotic therapy- In neonates, nafcillin or oxacillin + broad-spectrum cephalosporin, such as cefotaxime for the S. aureus, group B streptococcus, and gram-negative bacilli. If MRSA is a concern, vancomycin is selected . Small premature infant or has a central vascular catheter Pseudomonas aeruginosa or coagulase-negative staphylococci or fungi (Candida) should be considered. In older infants and children with septic arthritis, empirical therapy to cover for S. aureus, streptococci, and K. kingae includes cefazolin or nafcillin
- 59. Clindamycin and vancomycin are alternatives when treating CA-methicillin-resistant S. aureus infections. For immunocompromised patients, combination - vancomycin and ceftazidime or with extended-spectrum penicillins and -β lactamase inhibitors with an aminoglycoside. Adjunct therapy with dexamethasone for 4 days with antibiotic therapy appeared to benefit children with septic arthritis in one study but has not been studied in children with CA-MRSA septic arthritis.
- 60. Duration When the pathogen is identified sensitive Abx If a pathogen is not identified and patient's condition improving, therapy is continued with initial Abx. If a pathogen is not identified and patient's condition is not improving re-aspiration or the possibility of a noninfectious condition should be considered. Duration of antibiotic therapy is individualized depending on the organism isolated and the clinical course. 10 to 14 days is usually adequate for streptococci, S. pneumoniae, and K. kingae; longer therapy may be needed for S. aureus and gram-negative infections.
- 61. In selected patients, obtaining a plain radiograph of the joint before completing therapy can provide evidence (typically periosteal new bone) of a previously unappreciated contiguous site of osteomyelitis that would likely prolong antibiotic treatment. Oral antibiotics can be used to complete therapy once the patient is afebrile for 48-72 hr and is clearly improving
- 62. Monitoring of patient Failure to improve or worsening by 72 hr requires review of the appropriateness of the antibiotic therapy the need for surgical intervention the correctness of the diagnosis Failure of either of acute-phase reactants to follow the usual course should raise concerns about the adequacy of therapy Recurrence of disease and development of chronic infection after treatment occur in <10% of patients.
- 63. Some other Bone and joint infection Gonococcal Arthritis- within 2 wks of urethral discharge- usu. heals without pus- t/t penicillin, ceftriaxone Syphilis of joint- Congenital, Acquired Fungal Infections- OM, Madura foot.
- 64. Summary The numbers of bone and joint infections resulting from vaccine-preventable infections, such as Hib and S. pneumoniae, have decreased in recent years. S. aureus remains an important cause of pyogenic arthritis and osteomyelitis. Prevalence of CA-MRSA is increasing. Transition from intravenous to oral antibiotic therapy remains the treatment of choice for uncomplicated pediatric bone and joint infections if the family is reliable and close follow-up can be ensured.
- 65. References 1. Nelson textbook of Paediatrics – 19th edition 2. Maheshwori Essential Pediatrics 3. Diagnosis and Management of Osteomyelitis PETE R J. CAREK, M.D., M.S., LORI M. DICKERSON, PHARM.D., and JONATHAN L. SACK, M.D. 4. Bone and joint infections in children- Pediatrics in review Internet. http://emprocedures.com/arthrocentesis/analysis.htm
- 66. THANK YOU
Editor's Notes
- the behavior of boys might predispose them to traumatic events.
- Local swelling and redness with osteomyelitis may mean that the infection has spread out of the metaphysis into the subperiosteal space
- The x-ray of the distal tibia demonstrates periosteal elevation (left-image arrowhead) and osteolysis (right-image arrowhead) findings consistent with osteomyelitis. The x-ray shown demonstrates osteomyelitis of the metacarpal head (arrow) secondary to a closed-fist injury (courtesy of David Effron). Radiographic evidence of bone destruction finally becomes apparent by 10 to 21 days.
- Radiographs show a central oval lucency surrounded by dense reactive sclerosis usually within or close to the metaphysis and the lesion may extend across the physis Chronic abscess resulting from incomplete resolution of acute osteomyelitis and isolation of the infection by sclerotic bone Brodie abscess A Brodie abscess is a subacute osteomyelitis that occurs in children and young adults from hematogenous spread. Disease onset is usually insidious with only mild symptoms, usually pain or ache, and no systemic response. The delay in disease progression is thought to be secondary to a strong host-pathogen response. It most commonly involves the distal tibia and appears as a rounded area of lucency (arrow). It may progress to a chronic localized abscess. Treatment with antibiotics or surgery usually results in a complete cure, but there is controversy over when to proceed with procedural intervention.
- Osteomyelitis causes increased vascularity, inflammation, and increased osteoblastic activity, resulting in an increased concentration of 99mTc.
- Plain radiographs of the knee are unremarkable. B) T1 weighted MRI demonstrates marked decrease in signal intensity in the medial metaphysis and epiphysis of the distal femur. There is some involvement of the soft tissue. C) These findings are more pronounced in a T1 weighted MRI with gadolinium. Patients with sickle cell disease are at increased risk for bacterial infection, and osteomyelitis is the second most common infection. S aureus is still the most common microorganism responsible for infection, but Salmonella and Serratia species and Proteus mirabilis represent a disproportionate share compared with the general populace. The T1-weighted MRI shown demonstrates decreased signal within the metatarsal (arrow) in a patient with sickle cell disease due to osteomyelitis. MRI is the best imaging study for osteomyelitis (yellow arrow), and may also reveal diskitis (blue arrow), abscess, and/or involvement of the cord (red arrow).
- Course of therapy – if no pus(cellulitis) – only antibiotics, if pus – surgical drainage required
- including an antibiotic effective against CA-MRSA in the initial empirical antibiotic regimen is suggested.
- The oral regimen decreases the risk of complications related to prolonged intravenous therapy, is more comfortable for patients, and permits treatment outside the hospital if adherence to treatment can be ensured.
- Individualized depending on the organism isolated and clinical course. According to Maheshwori, Essential Pediatrics - <48 hr IV cefotax+ Amik for 2 weeks then Oral ->48hr – Surgical drainage
- Sequelae of skeletal infections might not become apparent for months or years long-term follow-up is necessary
- Proteolytic enzymes released from the synovial cells and chondrocytes also contribute to destruction of cartilage and synovium. Bacterial hyaluronidase breaks down the hyaluronic acid in the synovial fluid, making the fluid less viscous and diminishing its ability to lubricate and protect the joint cartilage. Synovial and cartilage destruction results from a combination of proteolytic enzymes and mechanical factors.
- manifested by glycosaminoglycan and collagen breakdown mediated via polymorphonuclear cells and cytokines secreted by the chondrocytes
- Joints of the lower extremity constitute 75% of all cases of suppurative arthritis. The elbow, wrist, and shoulder joints are involved in about 25% of cases, and small joints are uncommonly infected. Suppurative infections of the hip, shoulder, elbow, and ankle in older infants and children may be associated with an adjacent osteomyelitis of the proximal femur, proximal humerus, proximal radius, and distal tibia because the metaphysis extends intra-articularly
- Quantity : Average is 1.1cc. Range: 0.13 to 3.5 cc. Appearance / Clarity : Clear and colorless (one should be able to read a newspaper through the fluid) Viscosity : Very viscous Cell count : Average 63; Range: 13-180. Differential : Red blood cells: Zero Percent polymorphonuclear leukocytes: Average: 6.5%; Range 0-25 Lymphocytes: Average: 24.6%; Range 0-78 Monocytes: Average: 6.5%; Range 0-25 Mucin clot : Good Crystals : None Uric acid : Same as in plasma Glucose level difference versus plasma : Within 10 mg/100ml of plasma concentration
