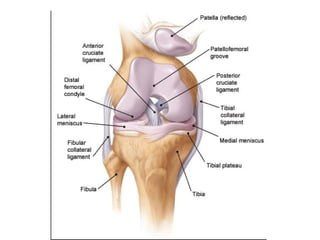
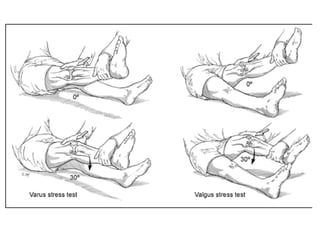
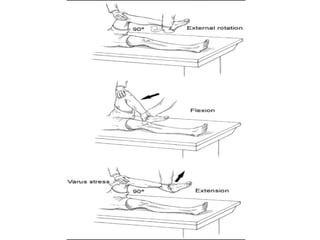
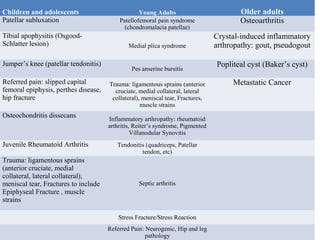
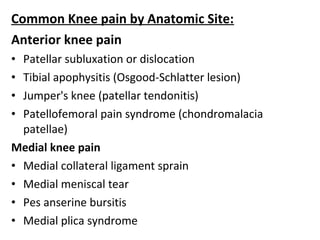
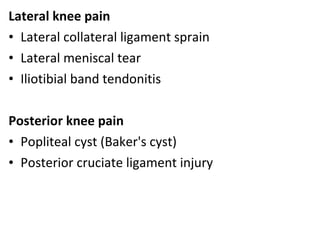
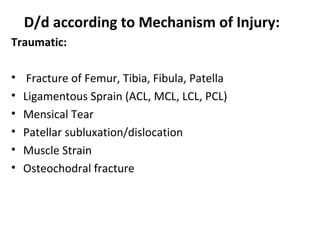
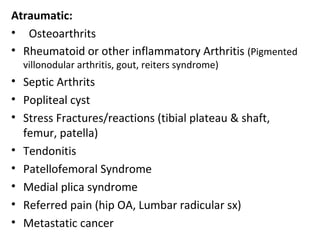
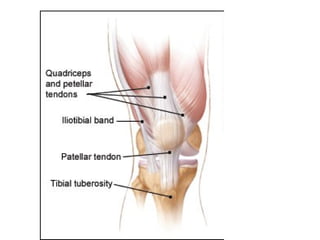
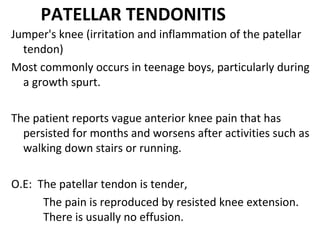
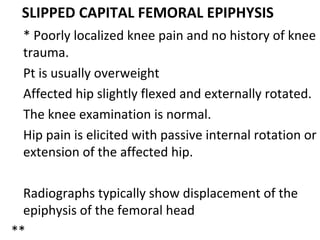
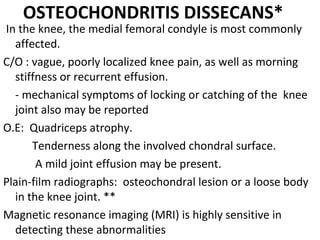
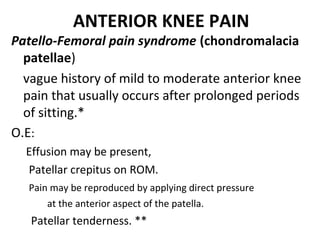
The document discusses the evaluation and diagnosis of knee pain, including its common causes and the specific symptoms associated with various knee injuries. It highlights the importance of a thorough medical history, physical examination, and diagnostic tests to accurately identify the source of pain, differentiating conditions by age group and mechanism of injury. Key examination techniques and interpretations of findings, along with common knee problems in children, adults, and older adults, are outlined to assist healthcare professionals in patient assessment.