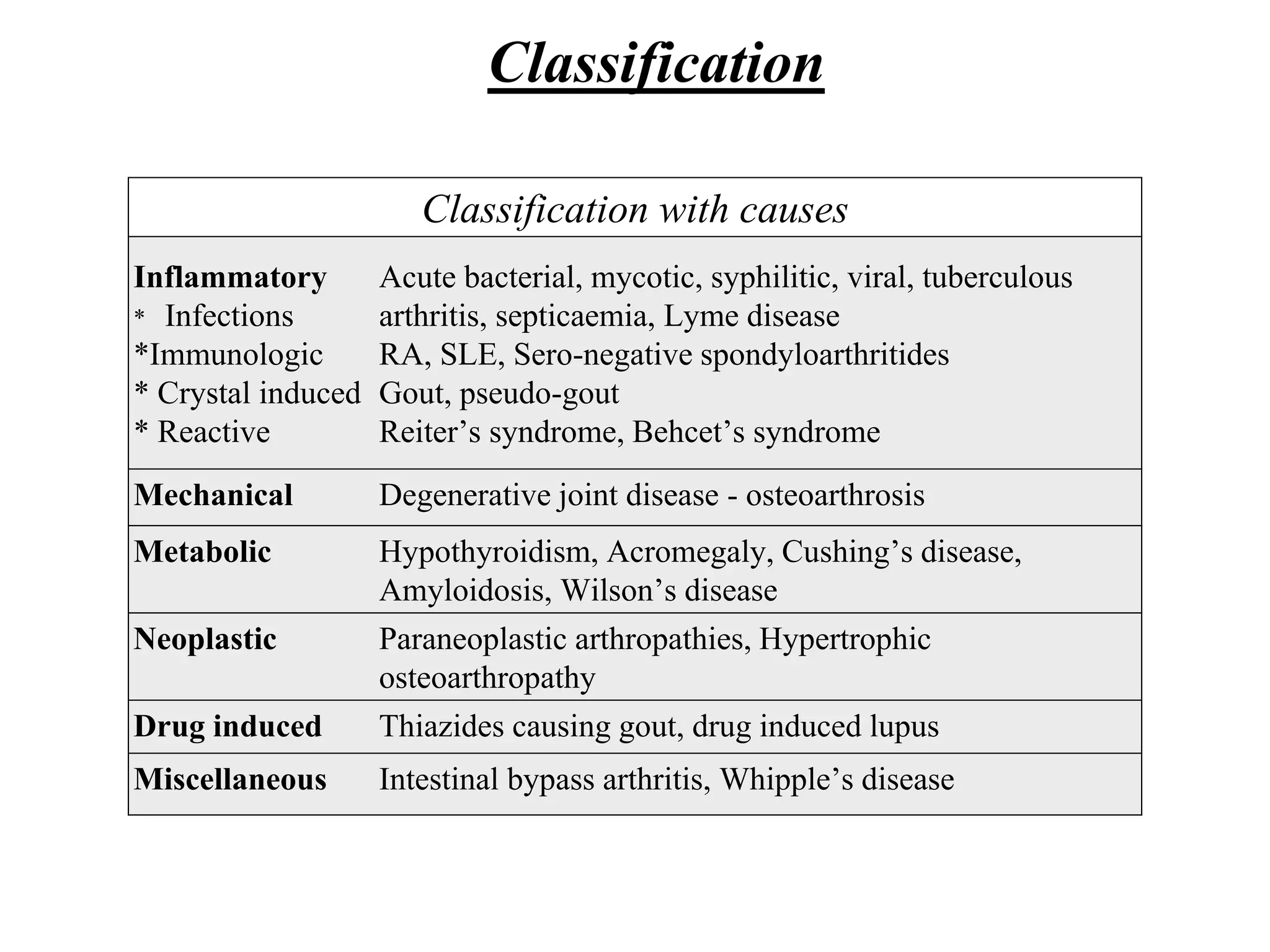
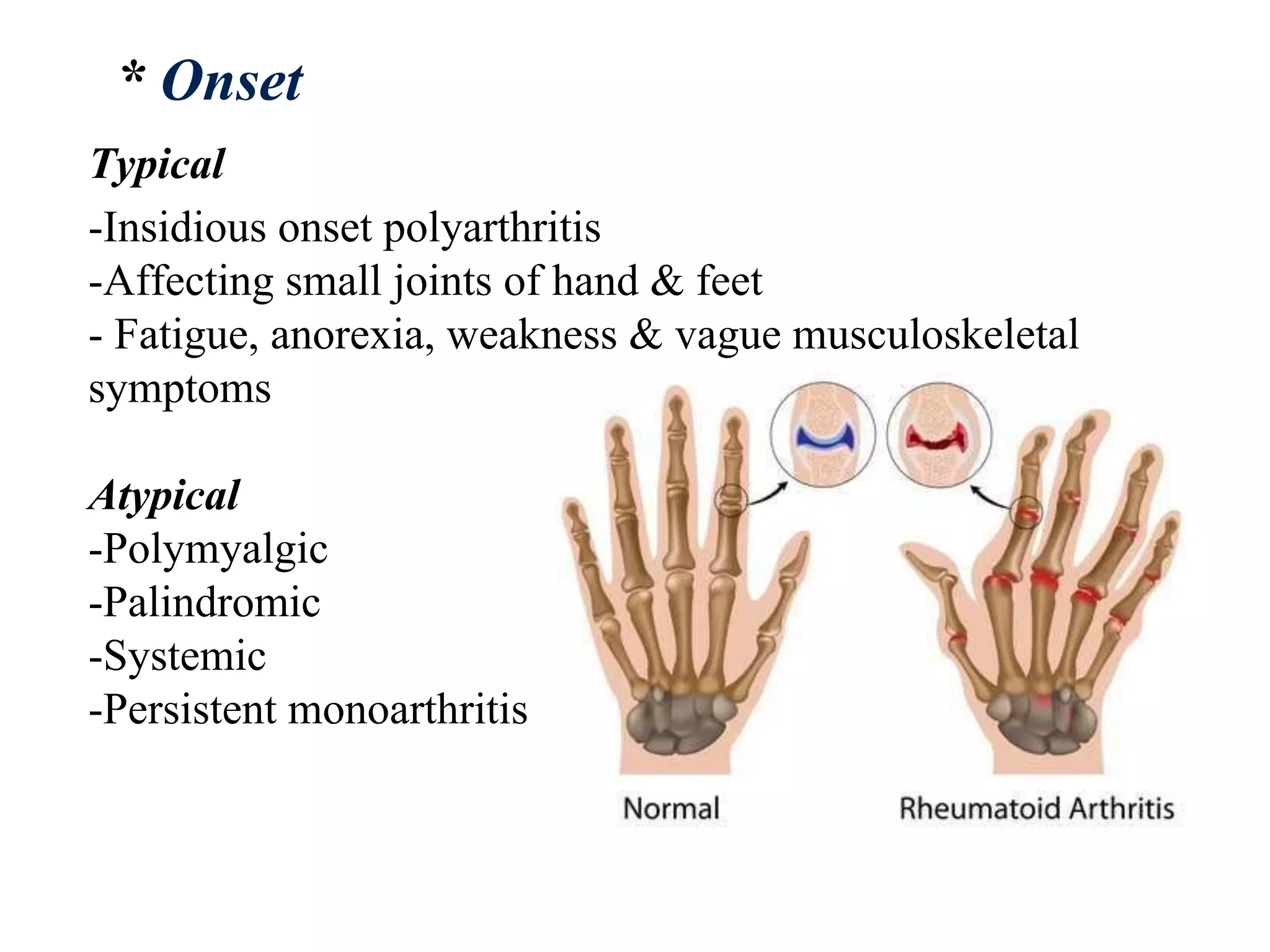
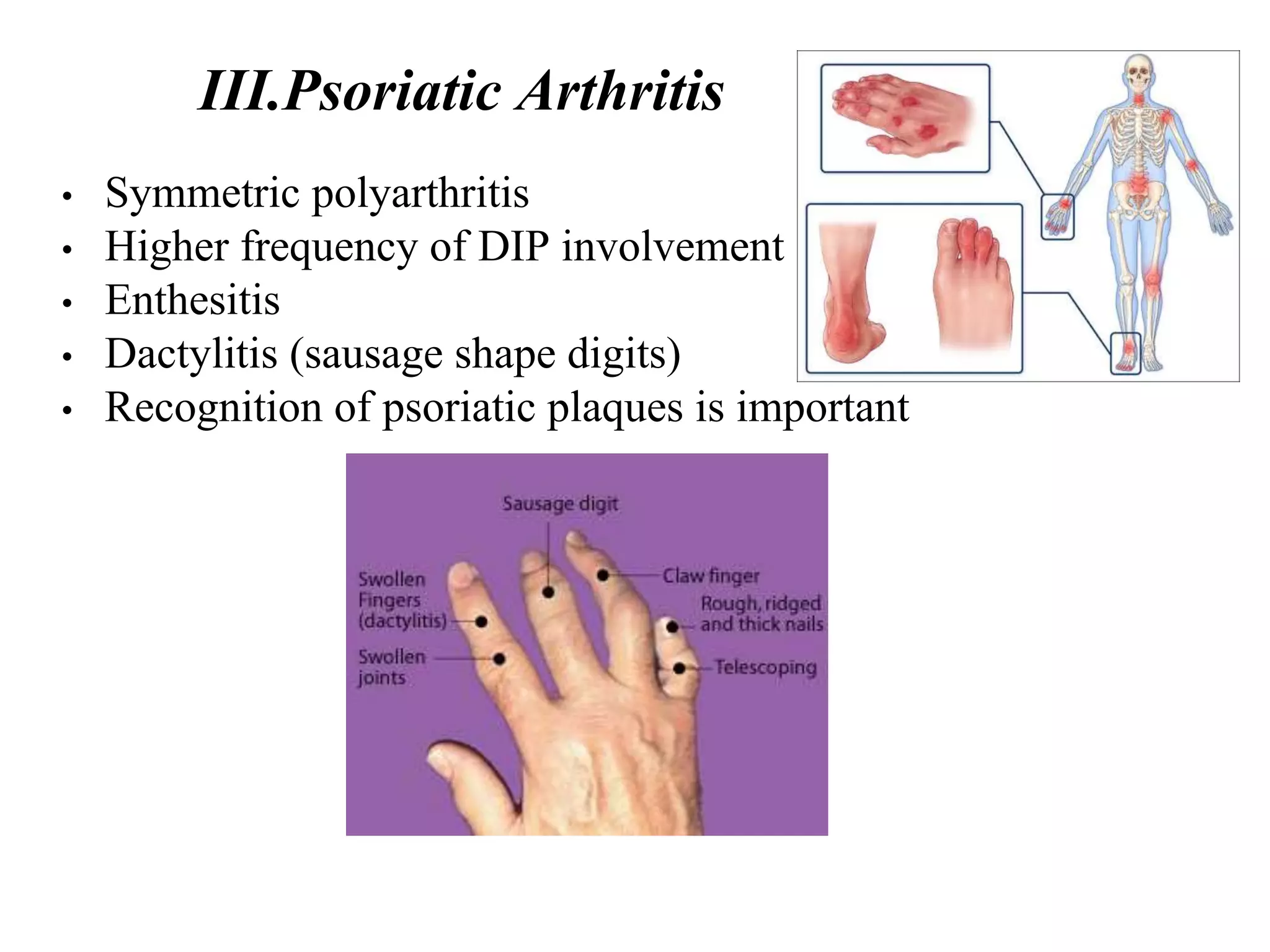
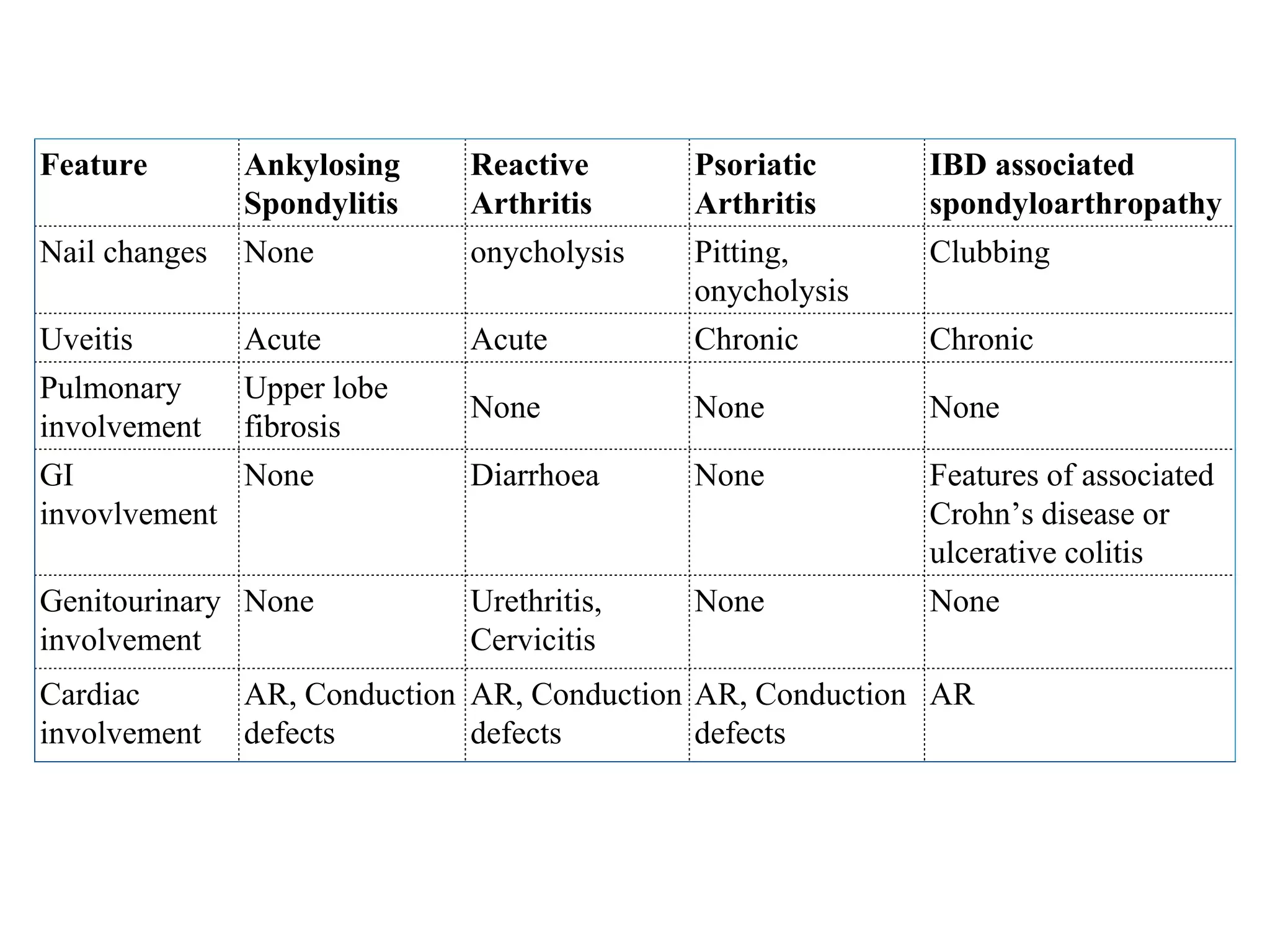
The document provides a comprehensive overview of polyarthritis, including its definition, classification, and various types such as rheumatoid arthritis and osteoarthritis. It discusses clinical features, symptoms, risk factors, and diagnostic criteria for different types of arthritis, emphasizing the prevalence and impact of these conditions. Additionally, it highlights the importance of assessing joint pain through various factors and explores associated diseases and syndromes.