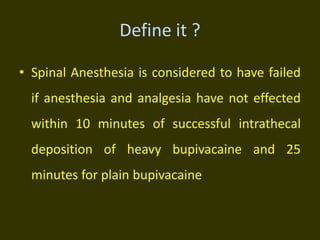
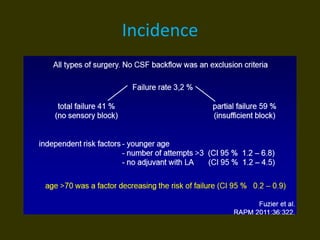
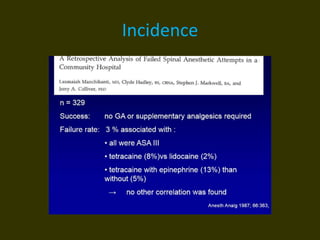
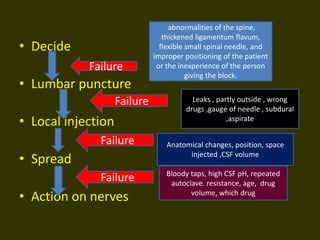
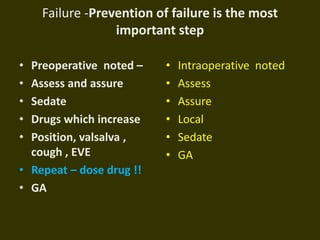
Failed spinal anesthesia can occur for several reasons:
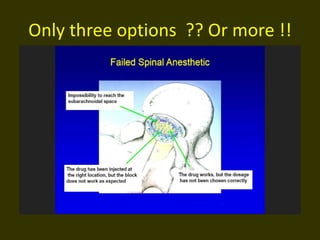
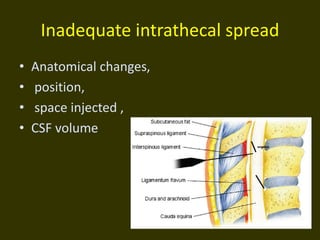
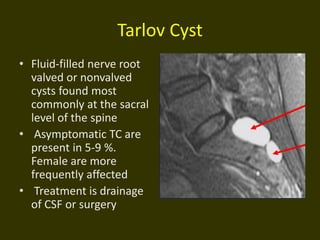
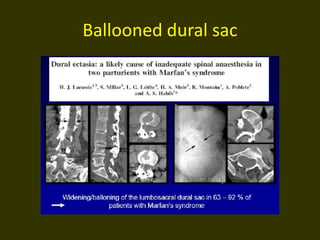
1. Anatomical abnormalities of the spine like thickened ligaments or spinal deformities can make proper needle placement difficult.
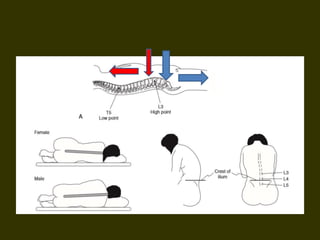
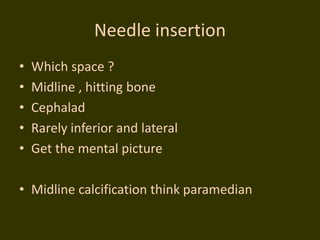
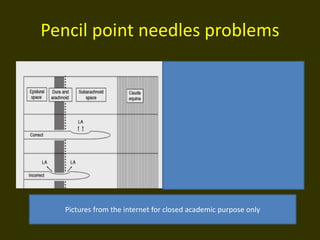
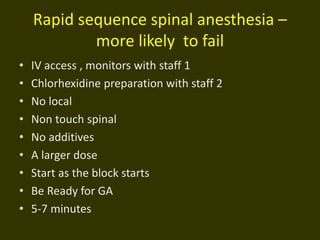
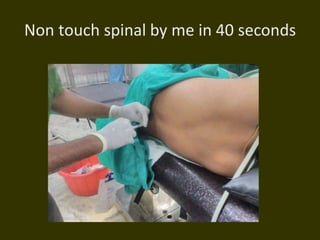
2. Technical errors like using too small of a needle, improper patient positioning, or inexperience of the practitioner performing the block can lead to failure.
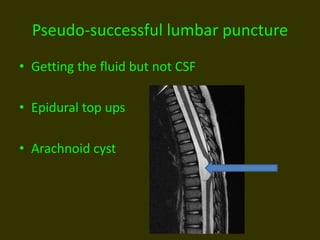
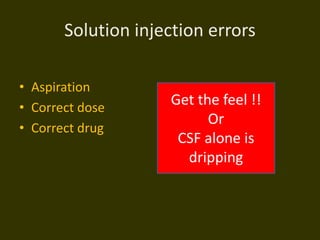
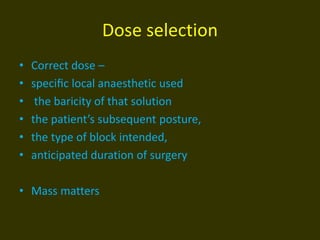
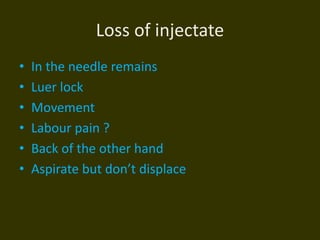
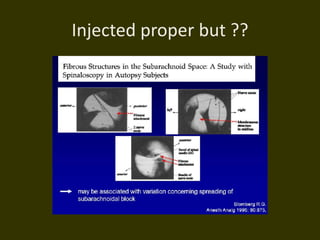
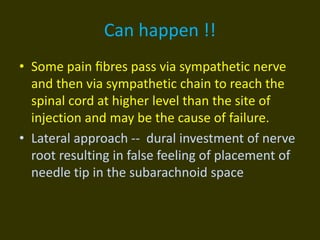
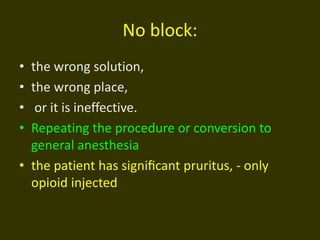
3. Injection issues such as injecting the anesthetic outside of the subarachnoid space, using the wrong drug or dose, bloody taps, or repeated autoclaving altering the drug properties may cause failure. Prevention through careful patient assessment, proper technique and addressing any identified risks is important to reduce failure rates.