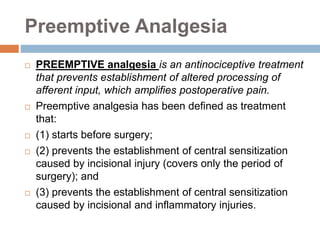
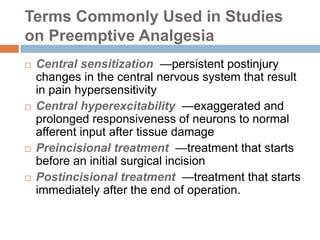
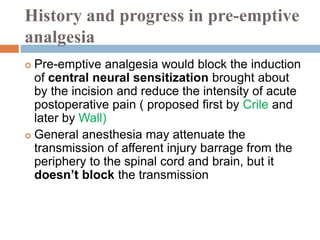
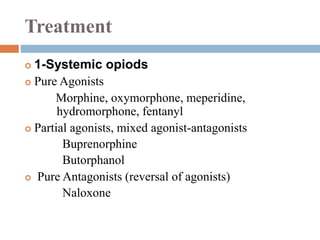
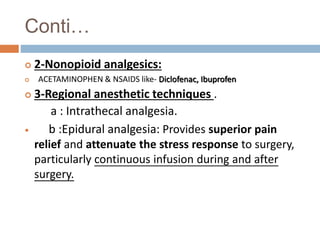
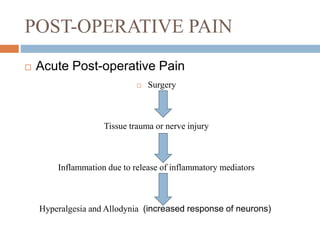
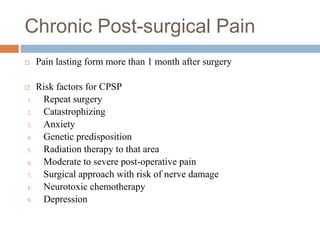
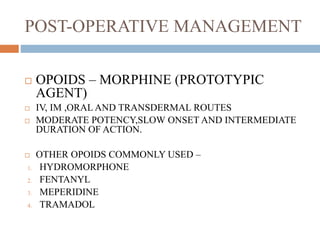
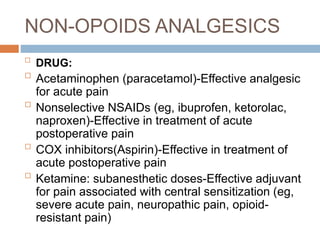
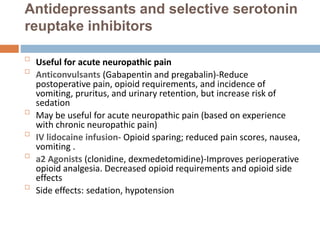
This document discusses preemptive analgesia, which aims to prevent central sensitization and reduce postoperative pain by administering pain medication before surgery. It defines preemptive analgesia and terms used in related studies. The history and use of preemptive analgesia is reviewed, along with various treatment options like opioids, nonopioid analgesics, regional anesthetic techniques, peripheral nerve blocks, and cryoanalgesia. Risk factors for chronic postsurgical pain are listed. Postoperative pain management includes opioids, nonopioids like acetaminophen and NSAIDs, antidepressants, anticonvulsants, IV lidocaine, and alpha-2 agonists to improve analgesia and reduce side effects.