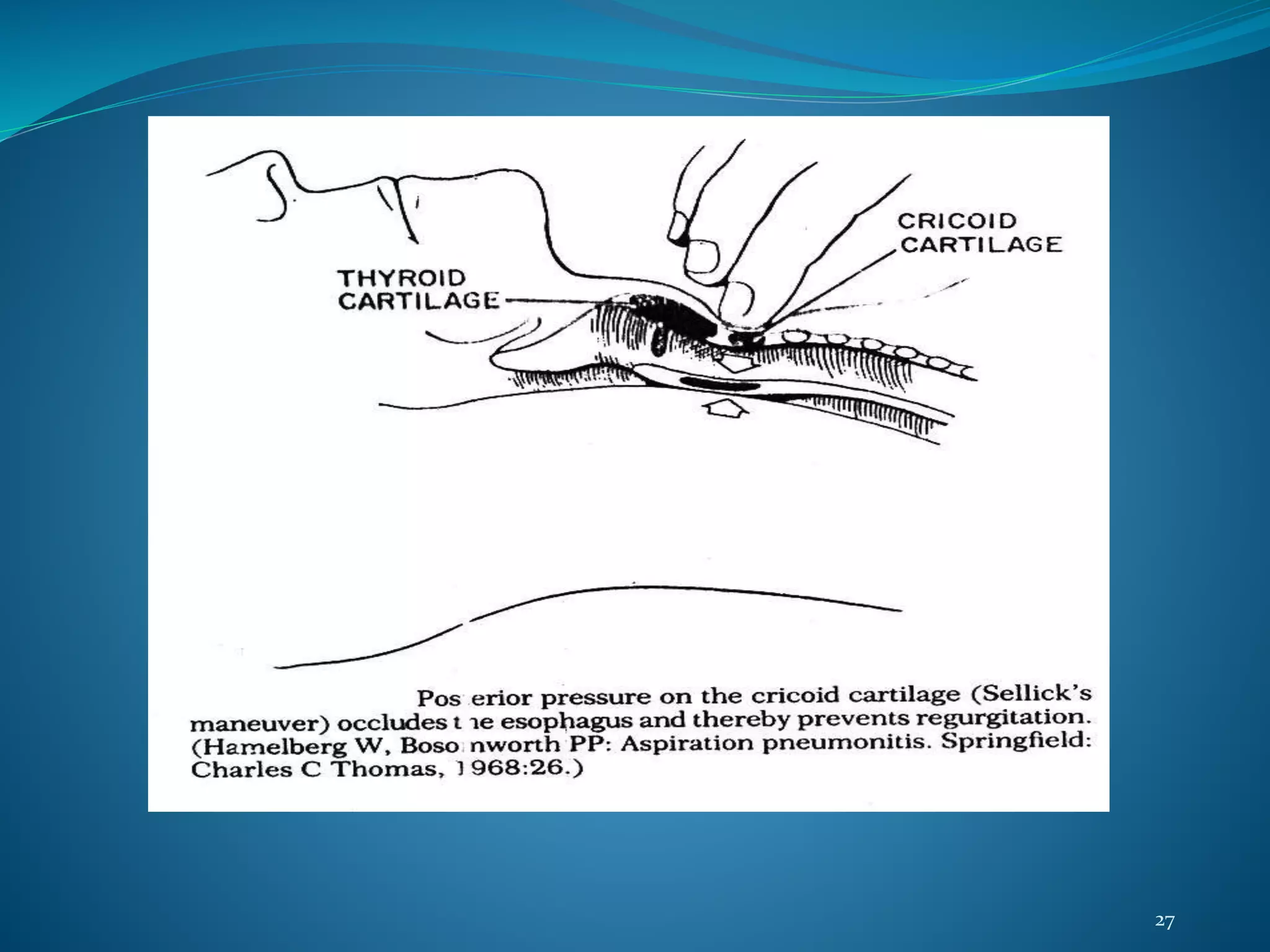
This document discusses aspiration, which is the misdirection of oropharyngeal or gastric contents into the larynx and lower respiratory tract. It covers several topics related to aspiration including gastric secretion, the lower esophageal sphincter, how aspiration occurs, types of injury (aspiration pneumonitis and pneumonia), signs and symptoms, risk factors, prevention, chemoprophylaxis, and treatment. The main points are that aspiration can cause chemical injury or infection in the lungs, risk factors include impaired consciousness and anatomical abnormalities, and prevention focuses on reducing gastric acidity and emptying contents before anesthesia.