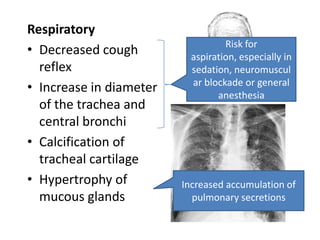
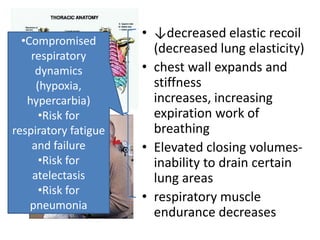
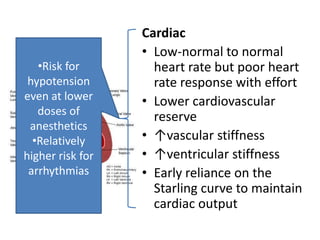
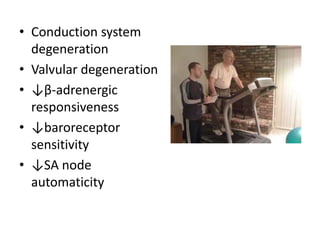
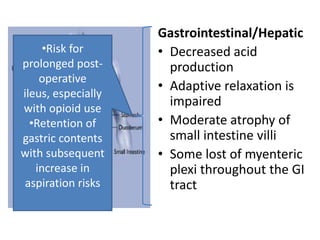
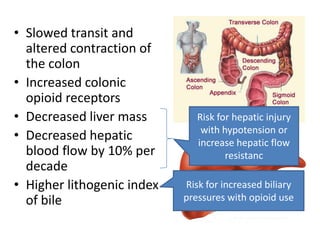
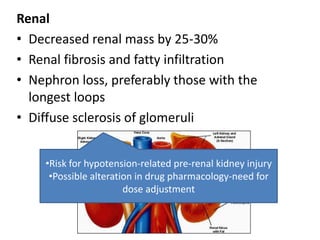
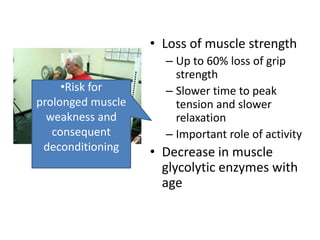
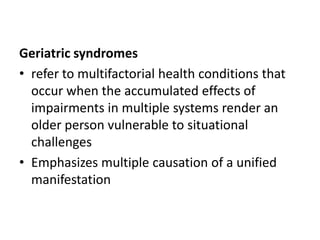
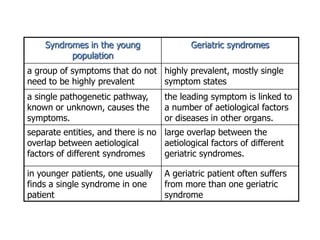
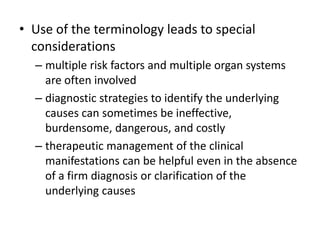
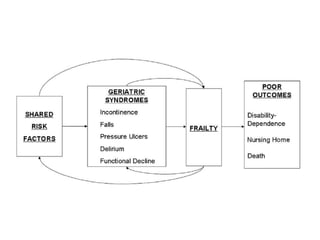
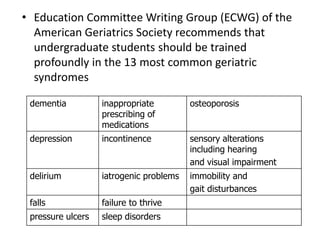
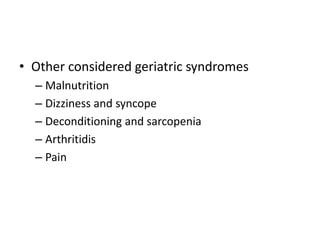
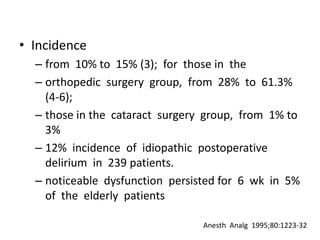
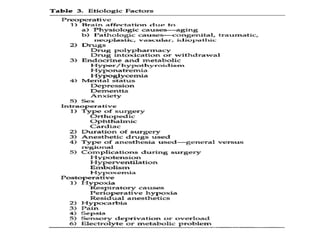
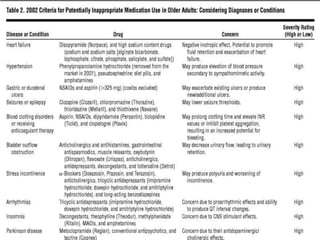
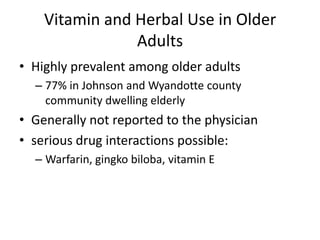
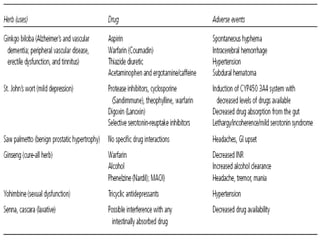
The document discusses anesthesia concerns in elderly patients, highlighting age-related physiological changes and the impact of comorbidities, particularly geriatric syndromes, on patient responses to anesthesia. It outlines various risks associated with respiratory, cardiac, gastrointestinal, hepatic, renal, and musculoskeletal systems as well as the potential for cognitive dysfunction post-anesthesia. Emphasizing the necessity for careful assessment and management, it notes the importance of considering these factors when preparing elderly patients for surgery.