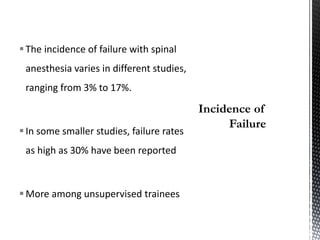
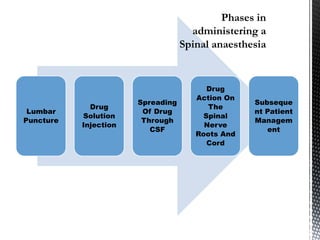
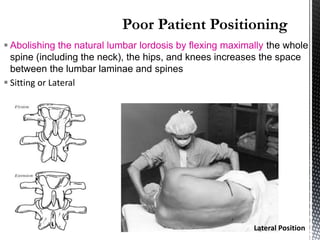
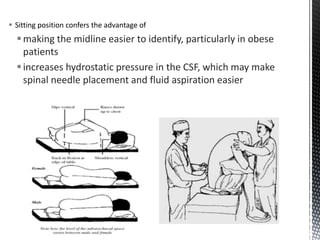
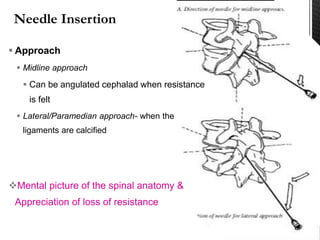
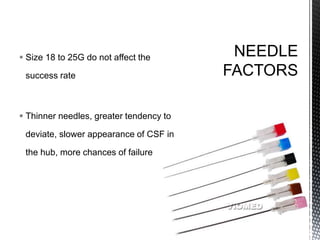
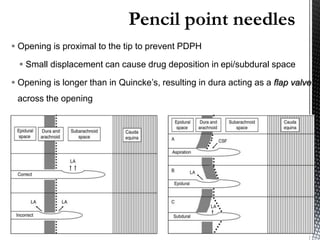
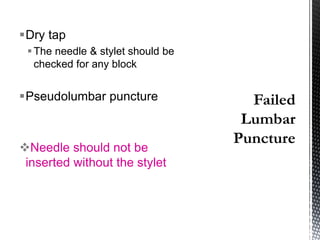
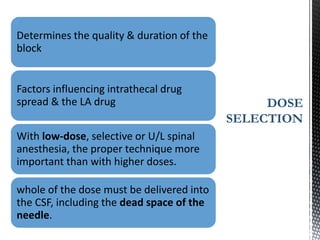
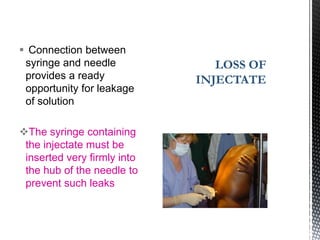
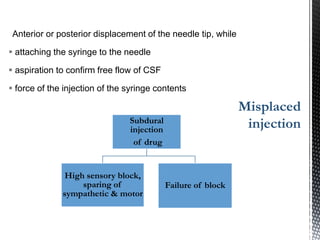
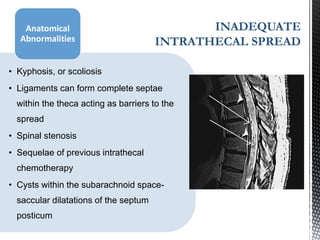
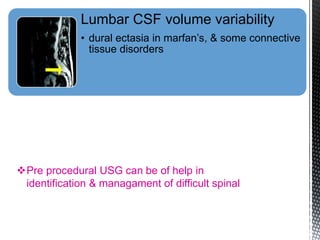
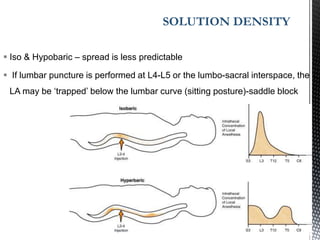
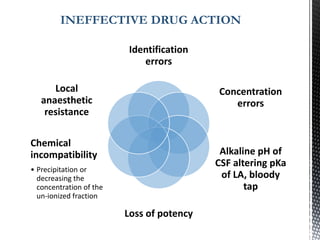
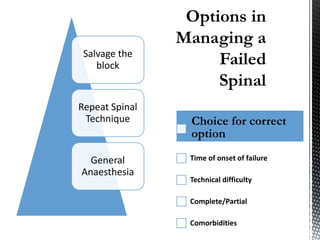
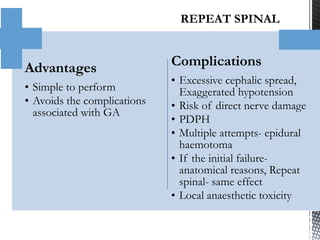
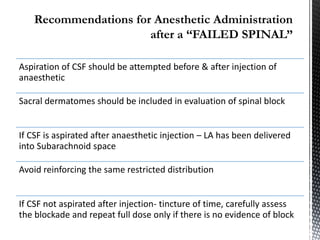
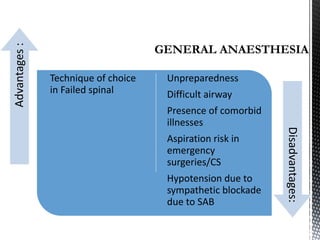
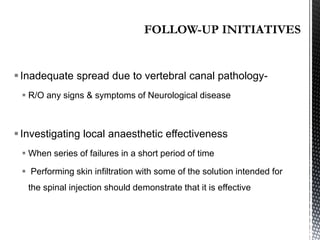
This document discusses failed spinal anesthesia. It defines failure as the surgery not being able to be performed under spinal anesthesia alone and needing general anesthesia. Failure rates are reported between 3-17% and up to 30% for trainees. Causes of failure include improper patient positioning, difficult lumbar puncture, issues with needle or drug placement, and anatomical abnormalities. Management depends on the extent of failure and includes repeating the spinal, using a lower dose, or switching to general anesthesia. Repeating spinal anesthesia carries risks and general anesthesia is preferable in some situations like emergency surgery. Proper technique is important to prevent failure.