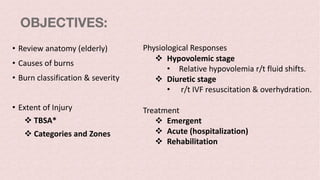
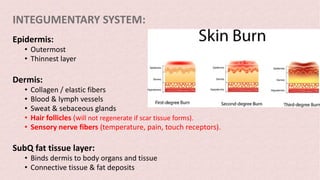
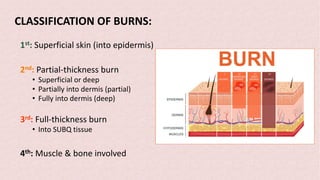
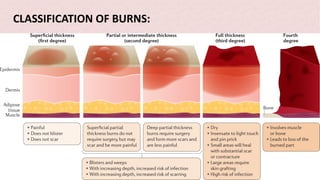
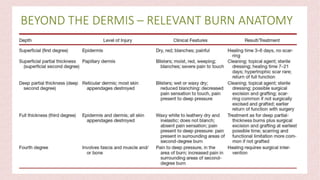
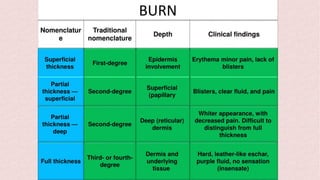
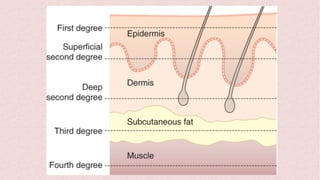
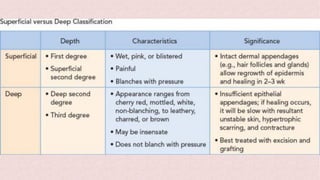
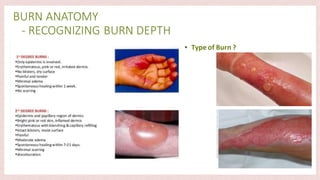
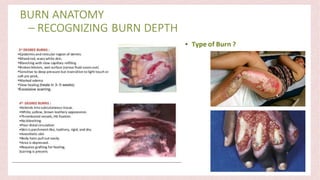
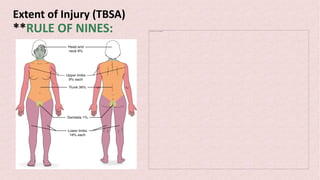
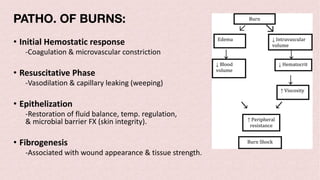
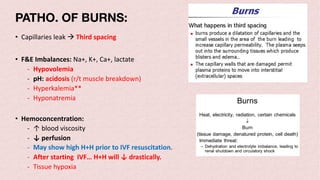
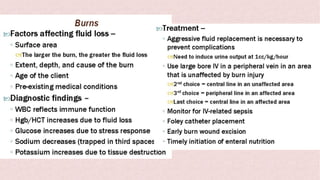
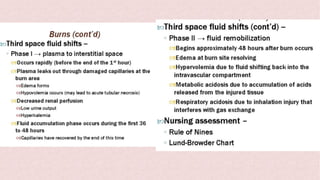
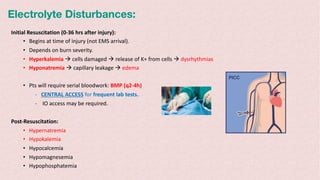
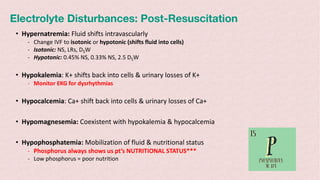
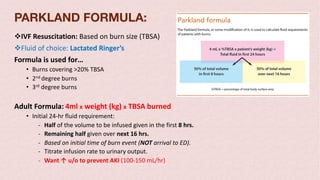
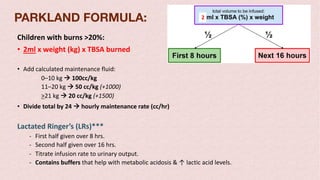
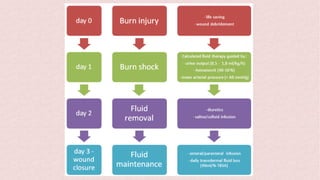
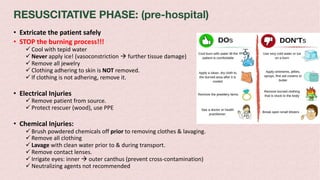
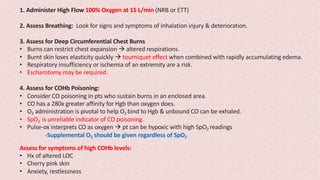
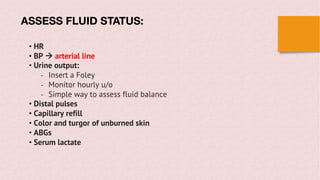
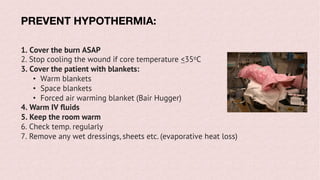
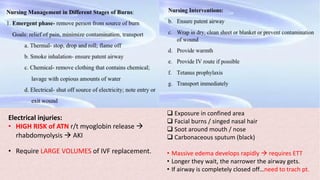
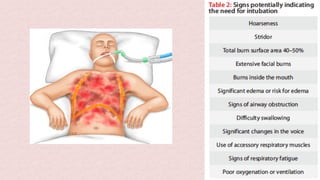
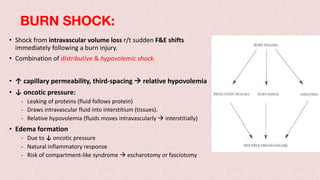
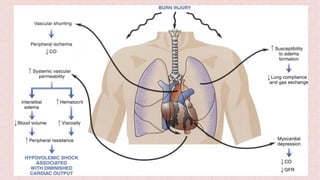
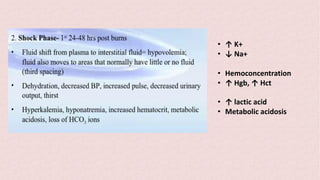
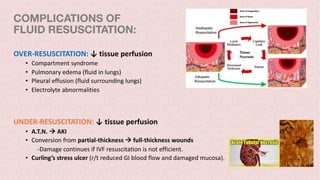
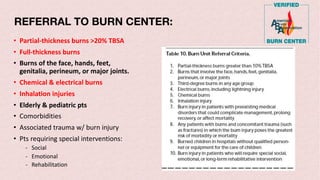
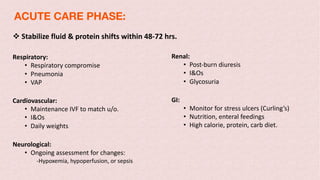
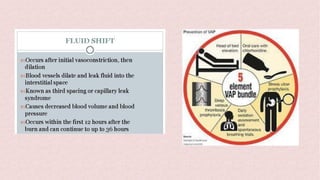
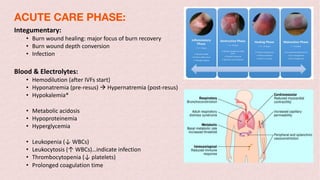
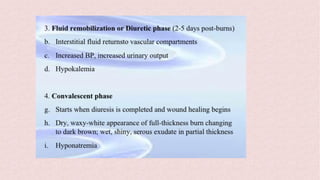
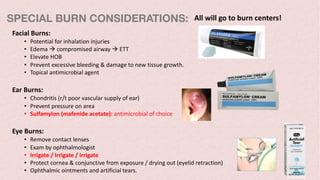
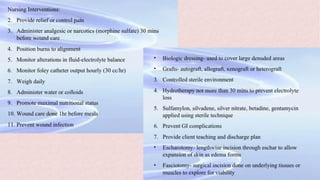
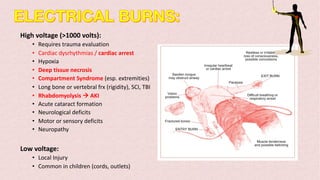
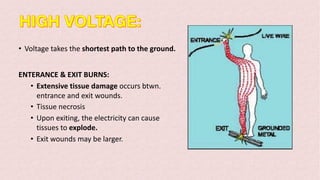
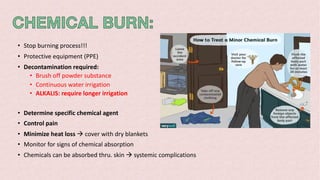
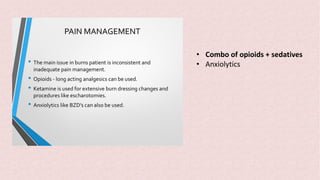
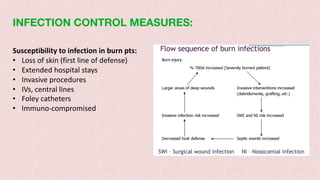
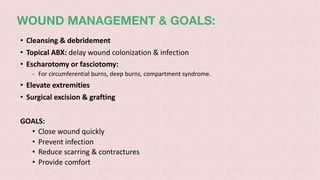
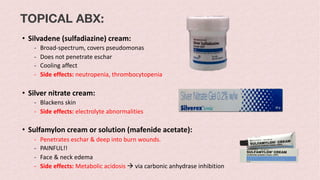
Burns can cause devastating physical and emotional effects. Classification is based on depth of skin damage from 1st to 4th degree. Severe burns increase risks of infections, loss of mobility, and multi-organ damage. Treatment involves stabilizing fluid and electrolyte shifts, administering IV fluids based on burn size, and preventing complications like shock, hypothermia, and infections. Patients with severe or complex burns may require referral to a specialized burn center.