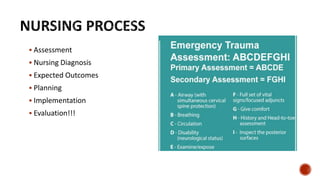
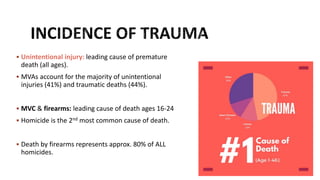
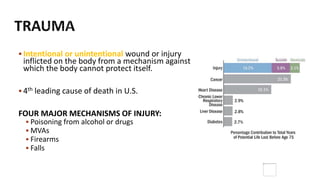
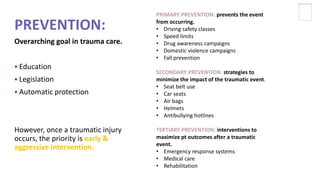
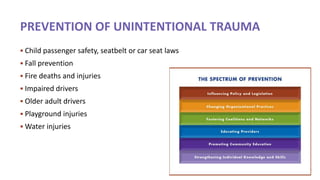
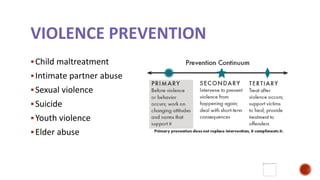
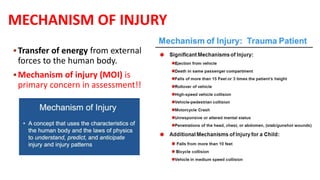
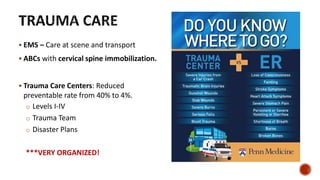
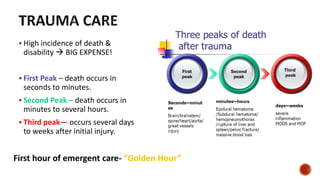
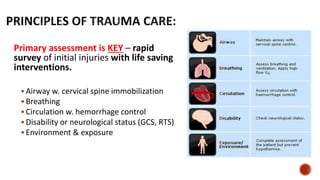
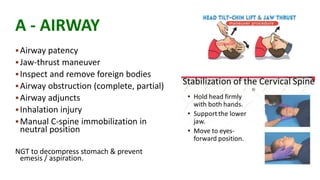
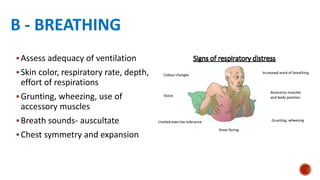
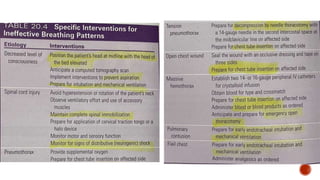
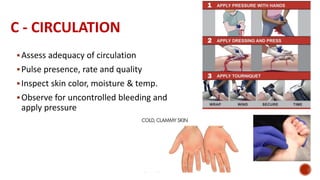
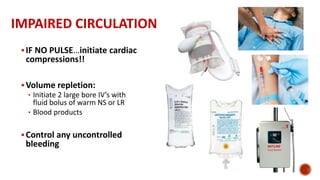
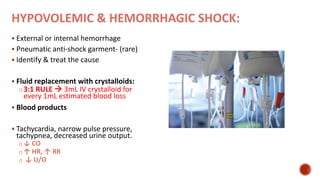
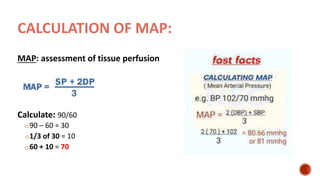
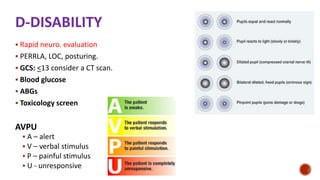
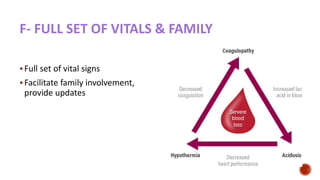
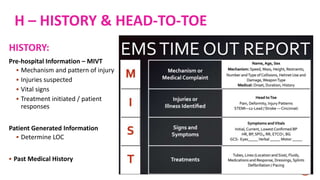
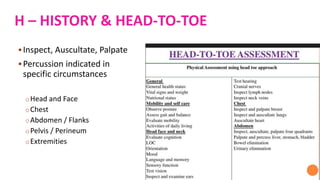
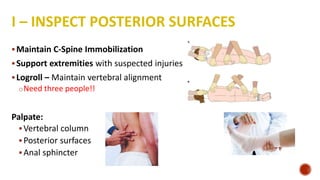
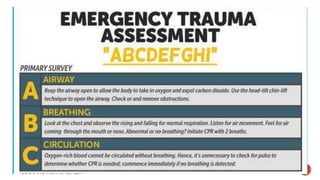
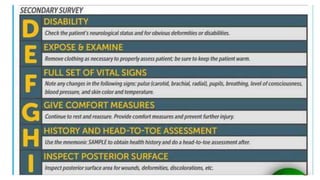
This document provides information on trauma care including mechanisms of injury, assessments of trauma patients, nursing interventions, and considerations in trauma patients. It discusses the primary and secondary survey process for trauma patients and identifying life-threatening injuries. Nursing priorities include establishing and maintaining a patent airway, ensuring adequate breathing and circulation, providing pain management and comfort measures. Special considerations are discussed for aging trauma patients, those with alcohol or drug use, and supporting family coping after a traumatic event.