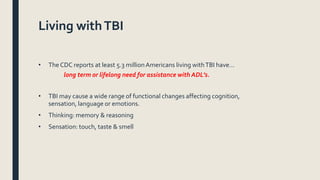
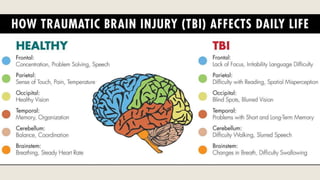
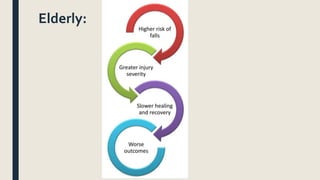
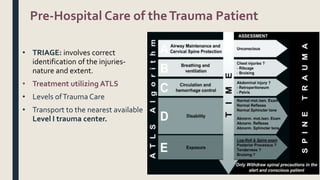
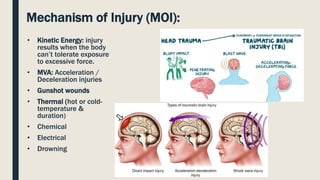
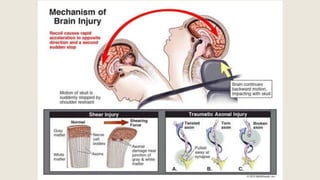
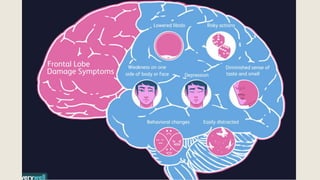
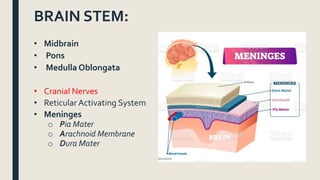
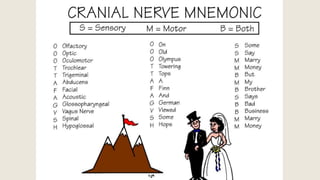
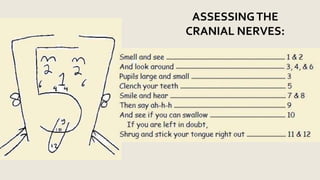
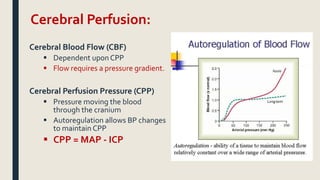
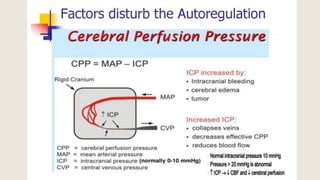
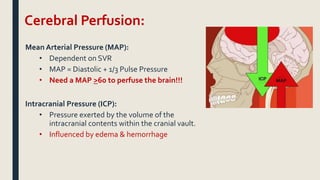
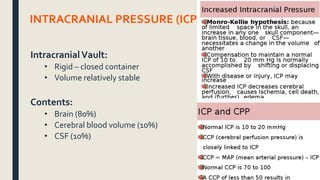
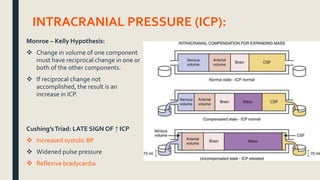
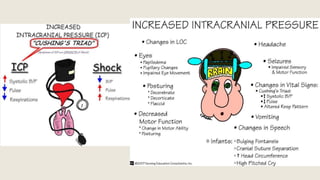
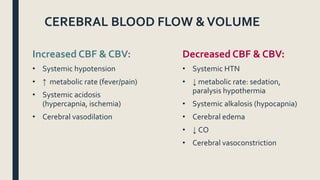
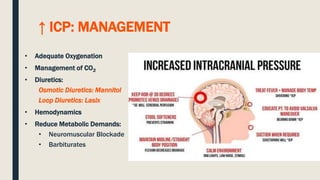
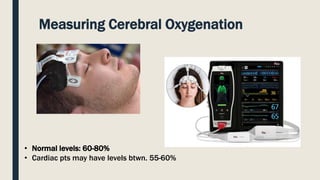
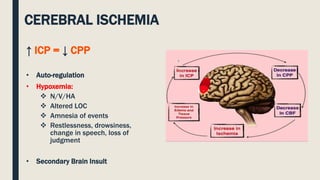
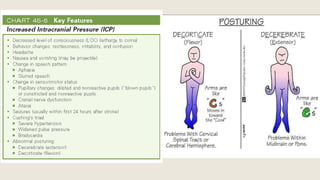
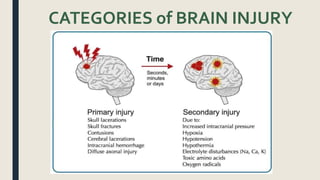
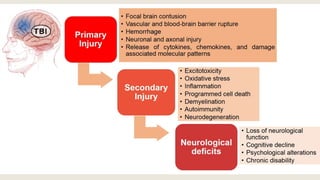
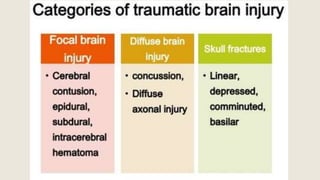
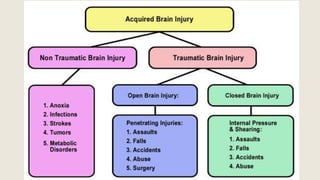
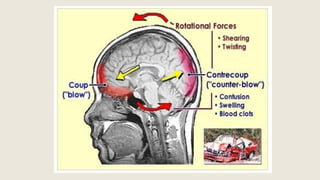
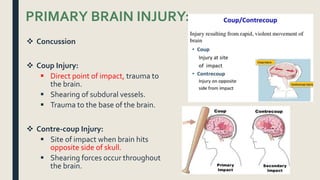
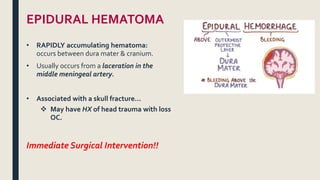
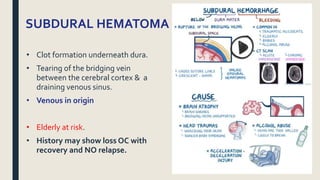
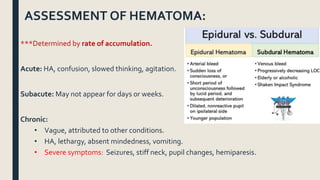
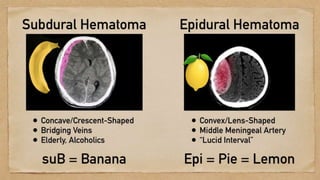
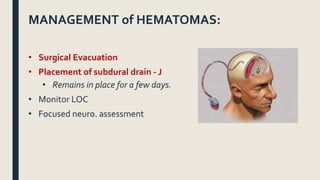
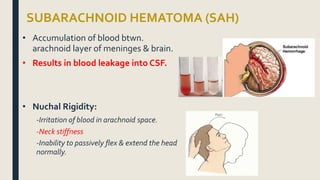
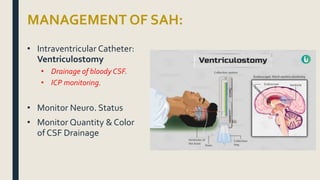
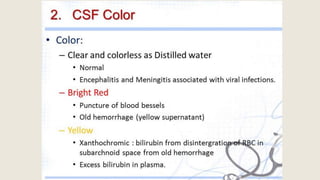
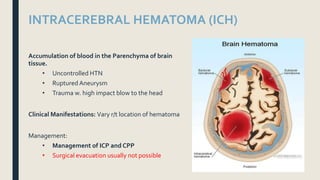
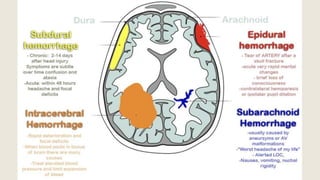
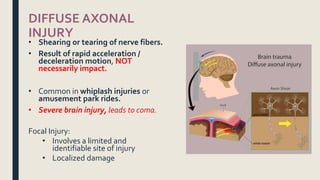
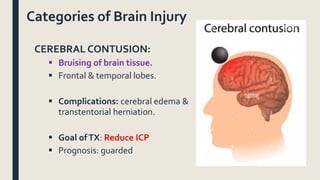
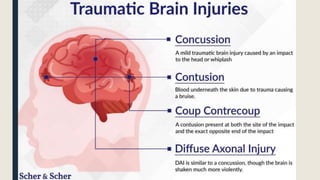
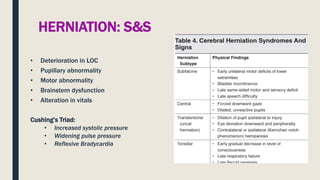
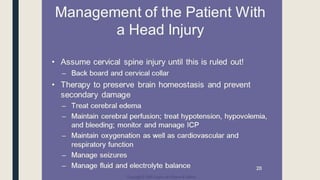
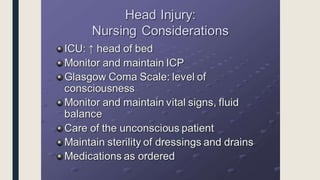
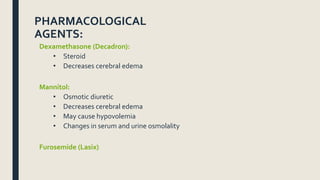
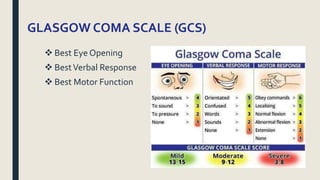
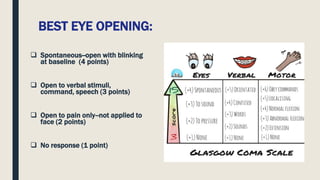
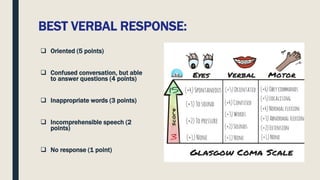
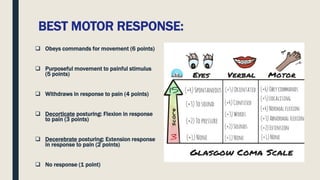
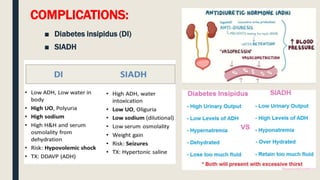
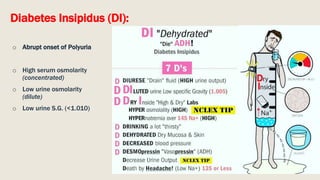
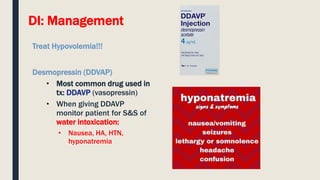
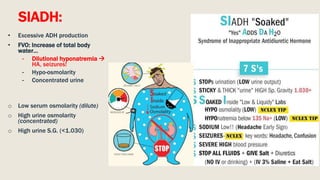
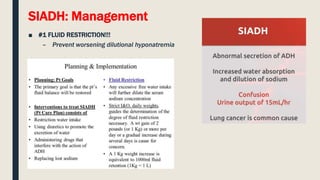
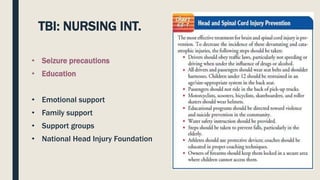
This document discusses traumatic head injuries, including causes, risk factors, pathophysiology, assessment, complications, and nursing management. It describes different types of brain injuries such as concussions, hematomas, herniations, and diffuse axonal injury. Key points include identifying high risk groups for TBI, assessing neurological status using the Glasgow Coma Scale, monitoring for increased intracranial pressure, and treating complications like diabetes insipidus and SIADH. Nursing focuses on maintaining cerebral perfusion, minimizing stimuli, and addressing psychosocial needs through education and support.