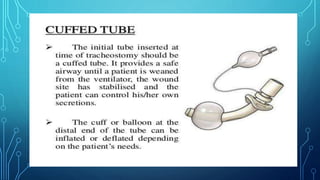
1) Endotracheal tubes and tracheotomy tubes maintain a clear airway, originally made of rubber but now plastic.
2) Tracheotomy involves making a small incision in the neck to insert a short tube into the trachea to ensure airflow.
3) Humidification methods include face masks, mouthpieces, tracheotomy masks, and humidifying T-tubes to introduce humidified air into the respiratory system.