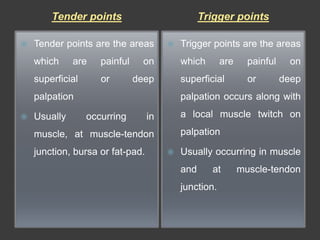
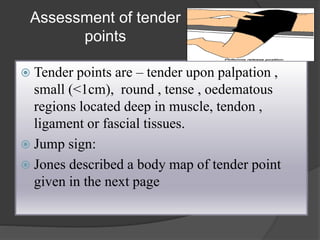
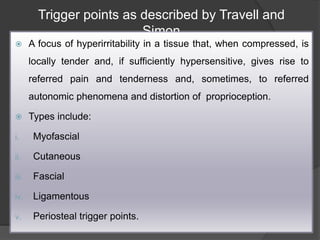
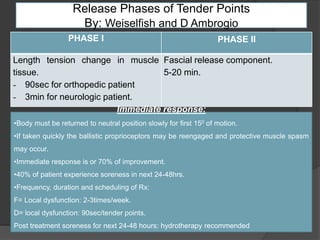
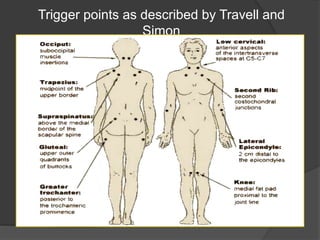
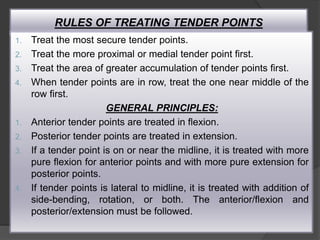
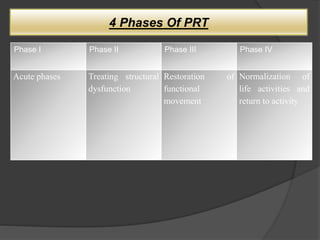
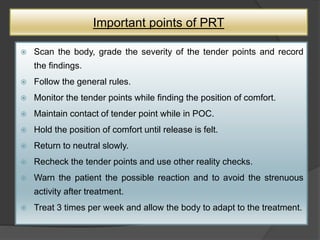
Positional Release Therapy (PRT) is an indirect manual technique developed by Dr. Lawrence Jones, designed to relieve musculoskeletal pain and dysfunction by placing the body in a comfortable position. The therapy focuses on tender points, identified as sensitive areas that indicate dysfunction, and aims to normalize muscle tension, improve range of motion, and enhance tissue circulation. PRT includes four phases and emphasizes a gradual return to neutral position to prevent protective muscle spasms following treatment.