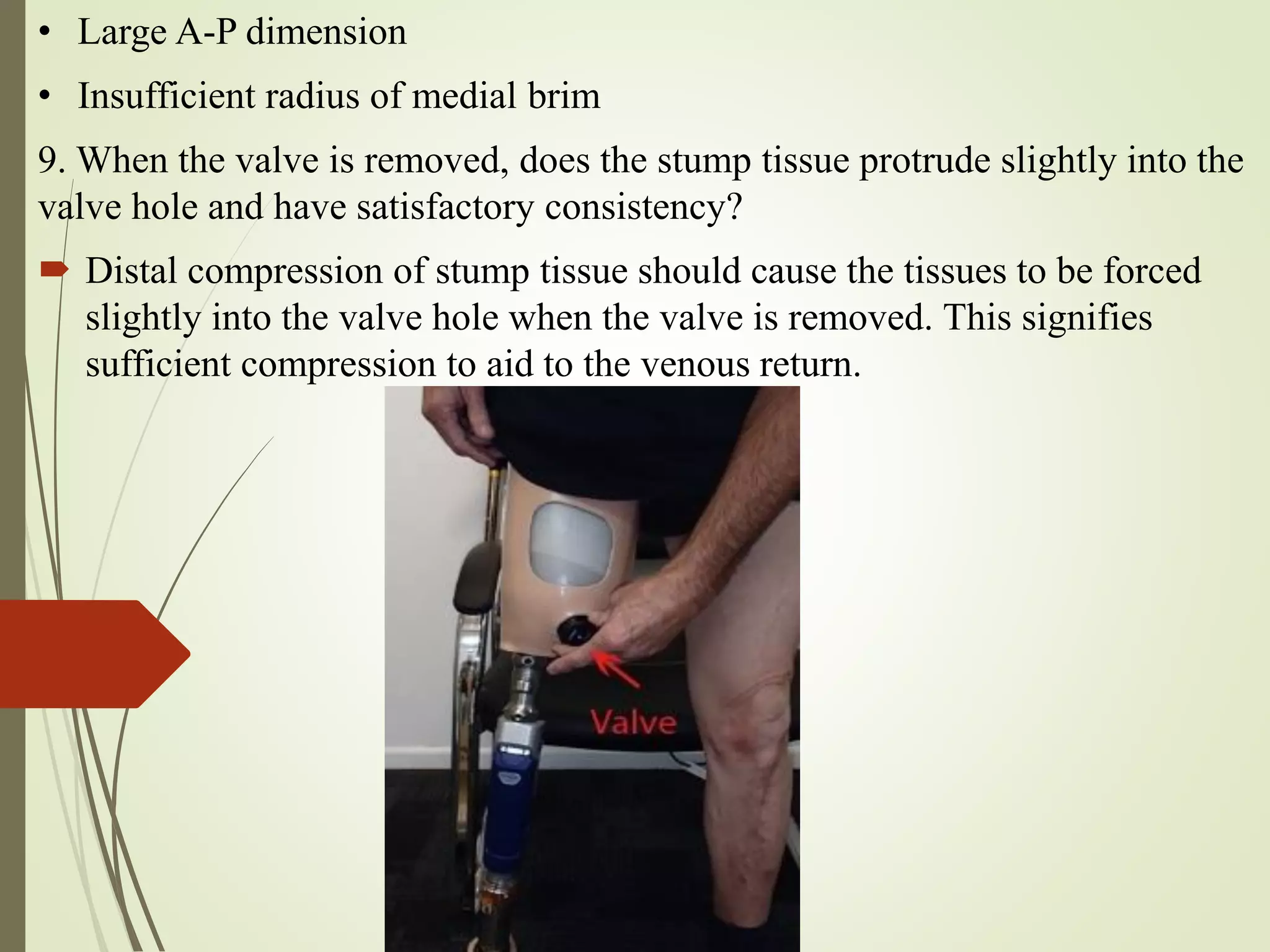
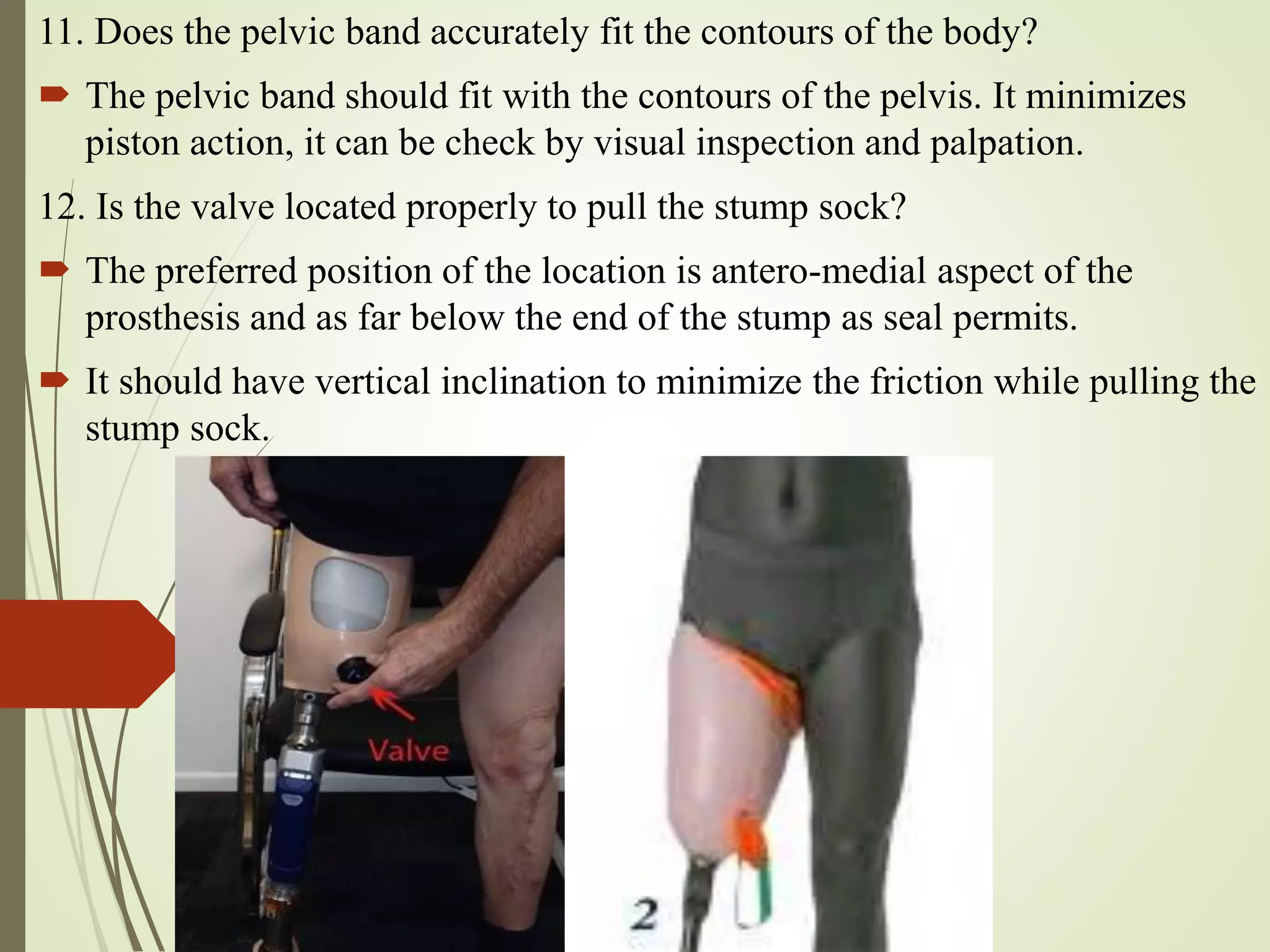
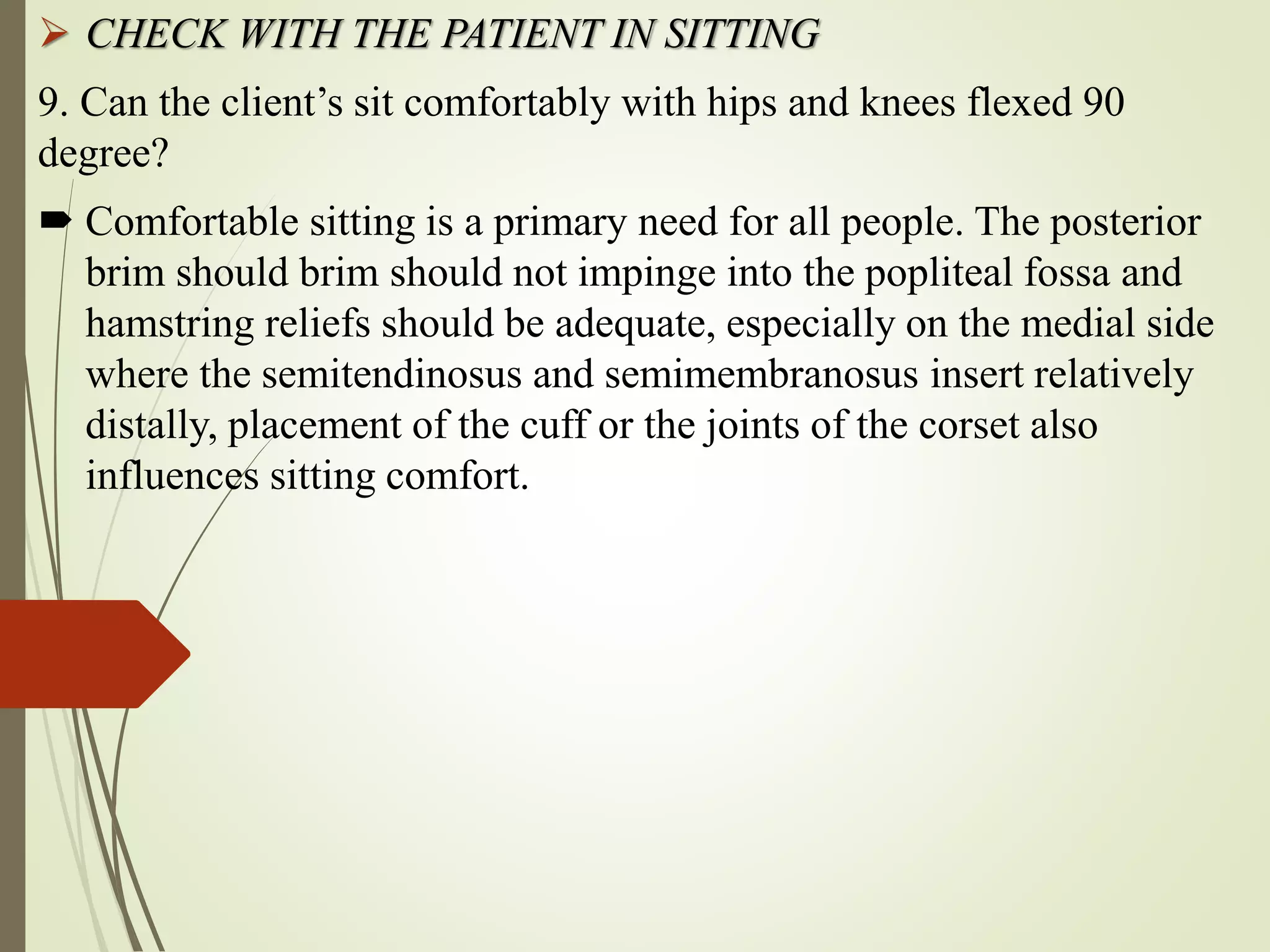
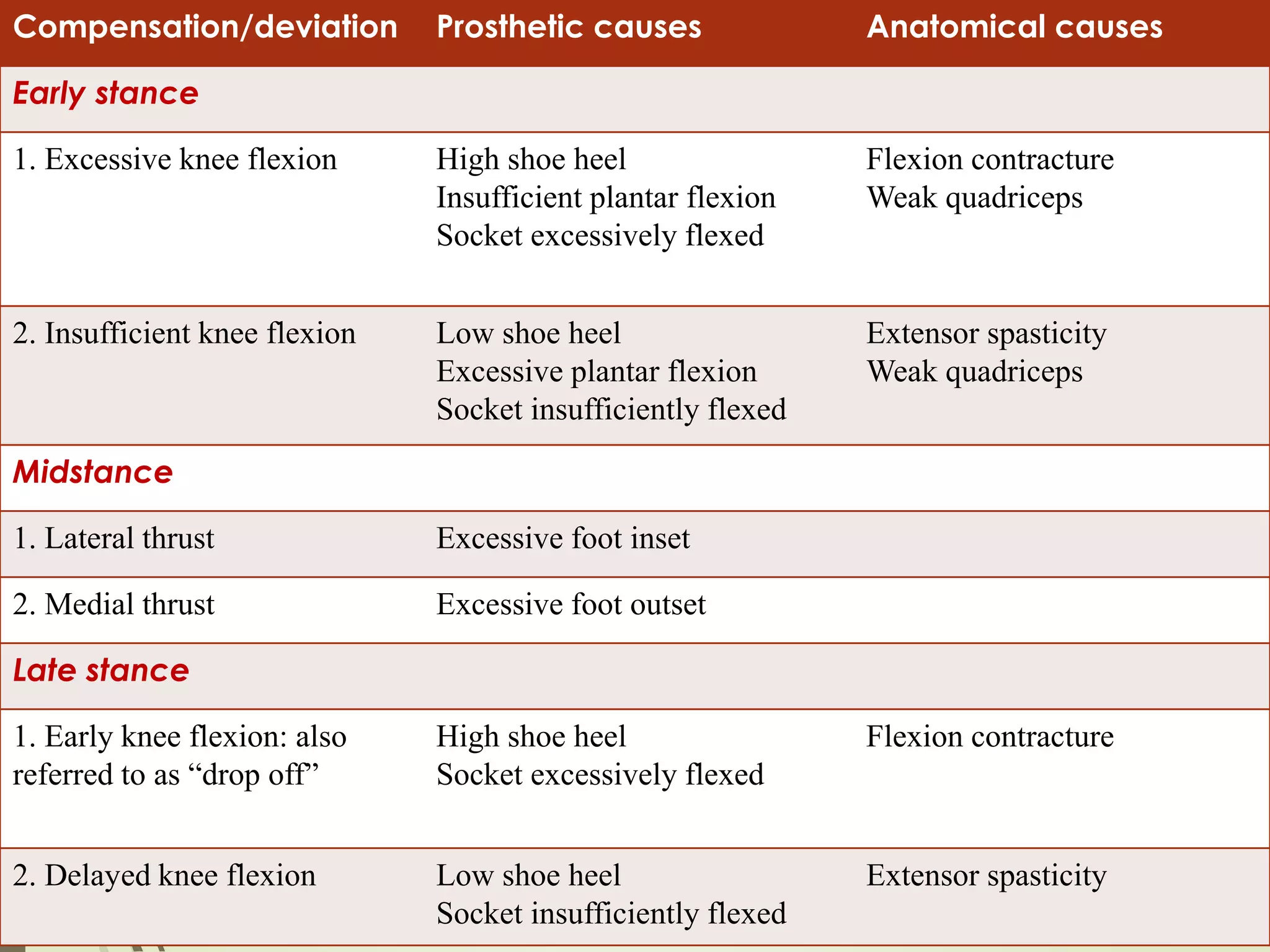
This document provides guidance on checking various aspects of a lower limb prosthesis. It discusses checking the prosthesis and patient's stump in general, as well as when sitting, standing, walking, and with the prosthesis removed. Checks include ensuring proper fit and alignment of socket components, comfort and stability of the patient, and identification of any potential issues. The document focuses on checkouts for above knee prosthetics but also briefly discusses below knee prosthetics. The goal of prosthetic checkouts is to assess proper functioning and make any necessary adjustments before training the patient.