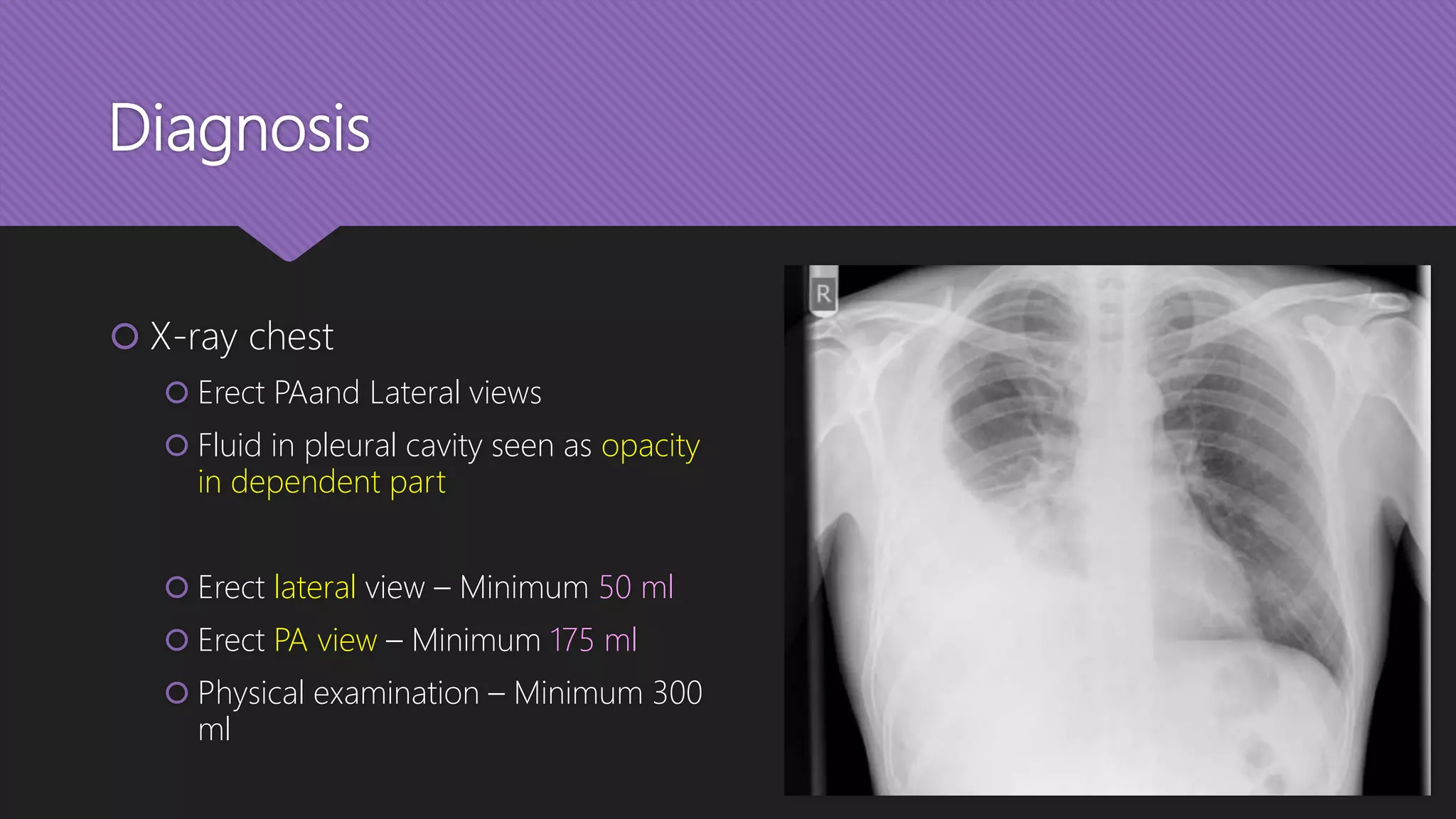
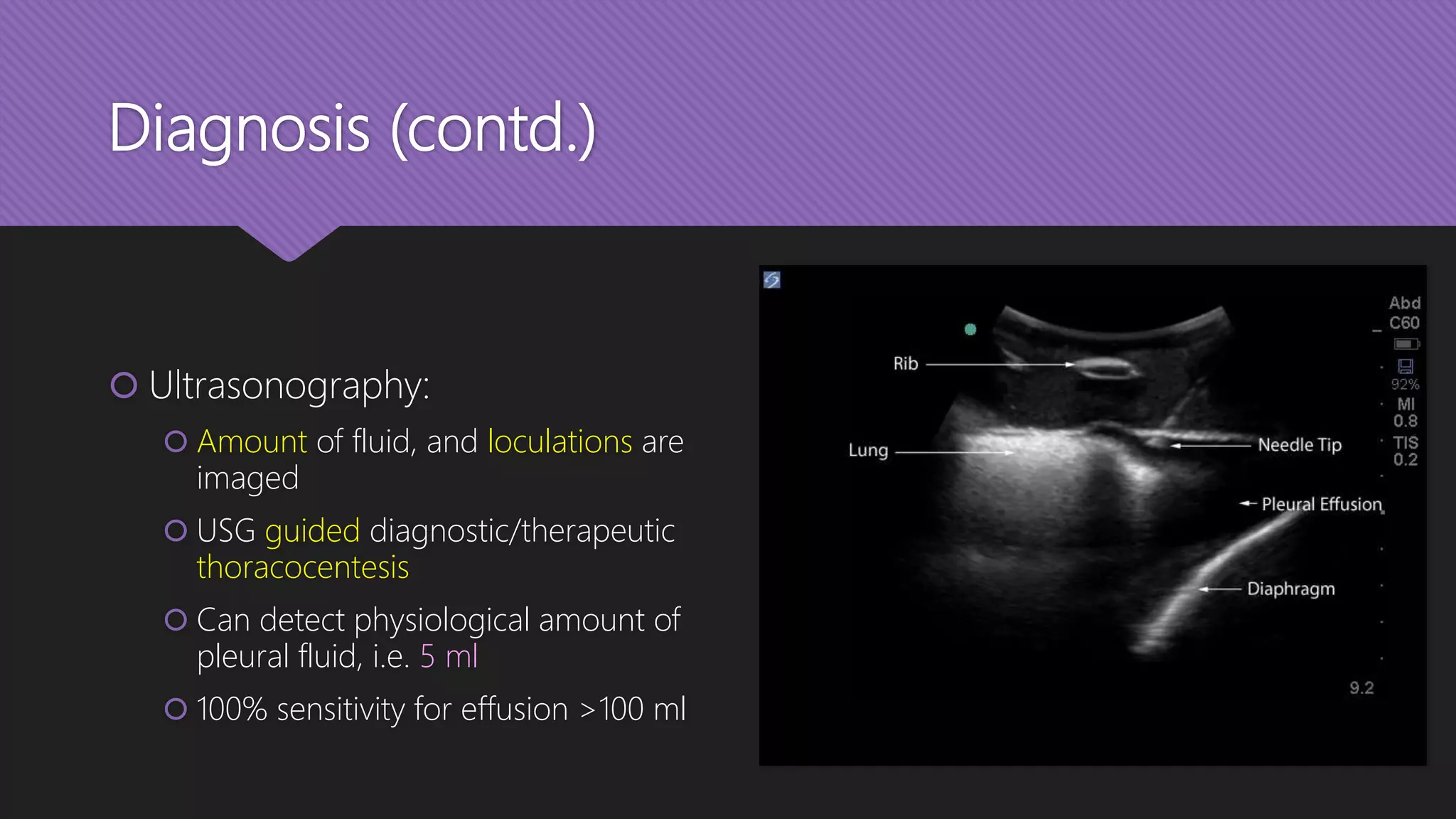
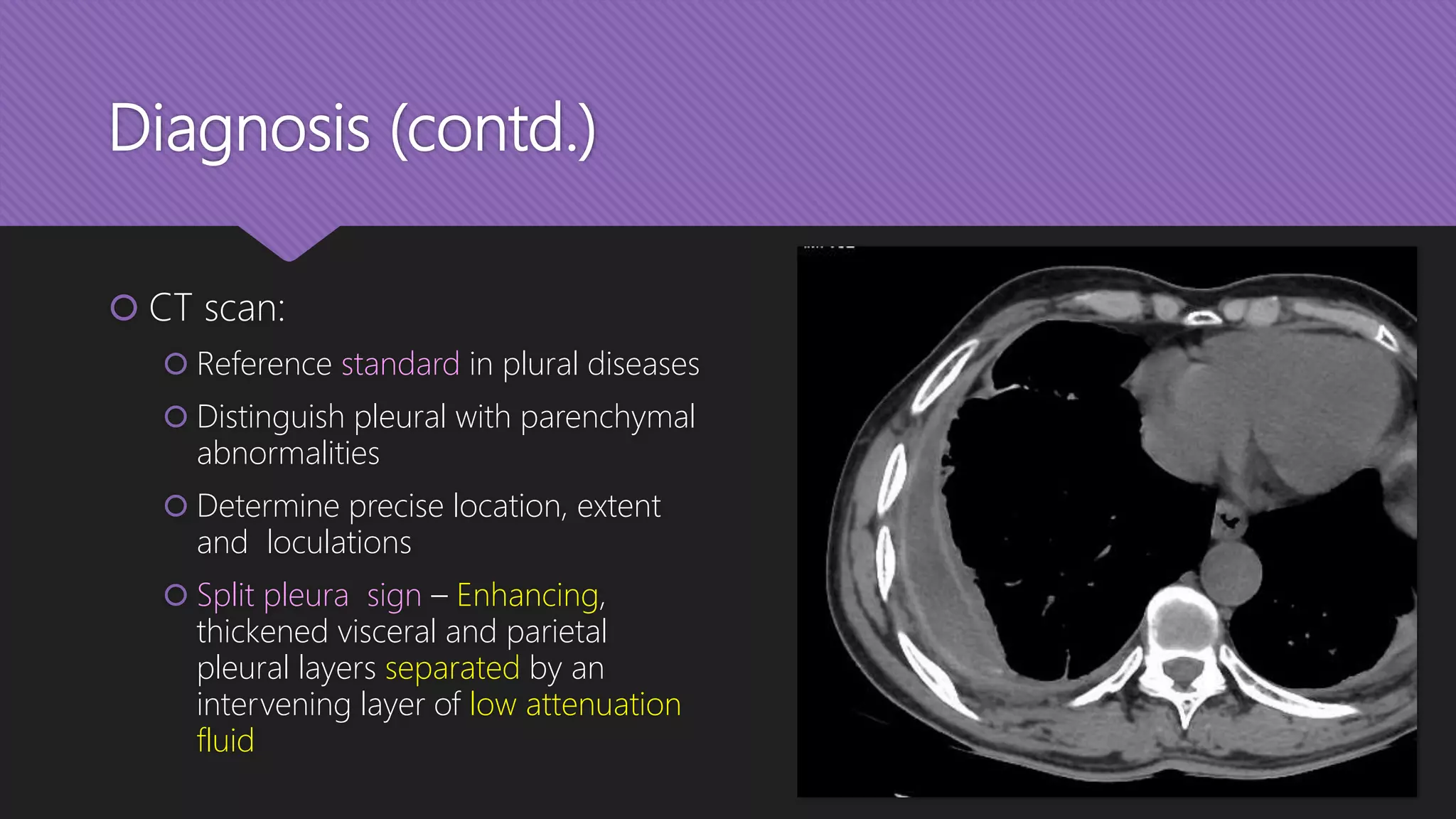
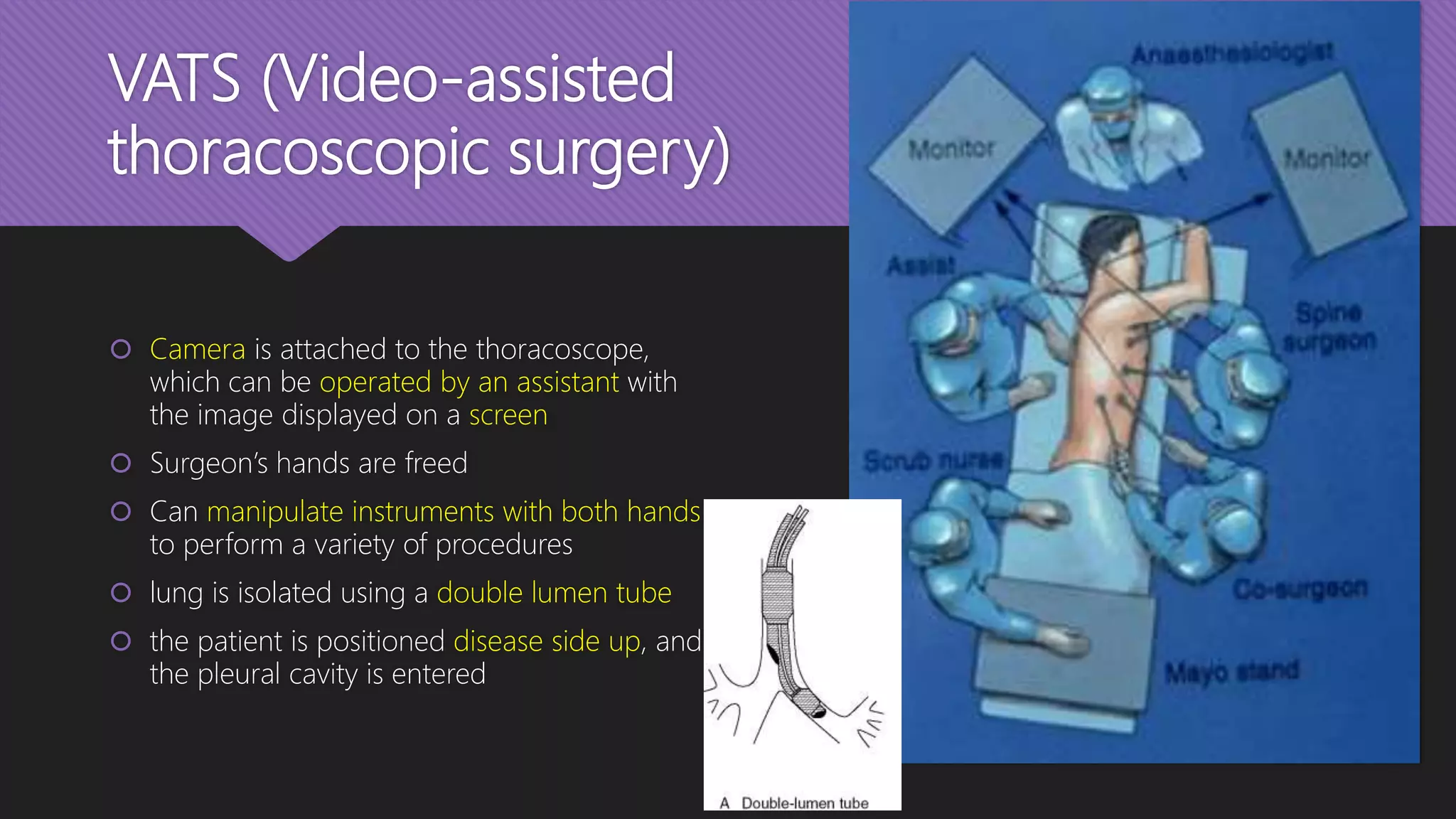
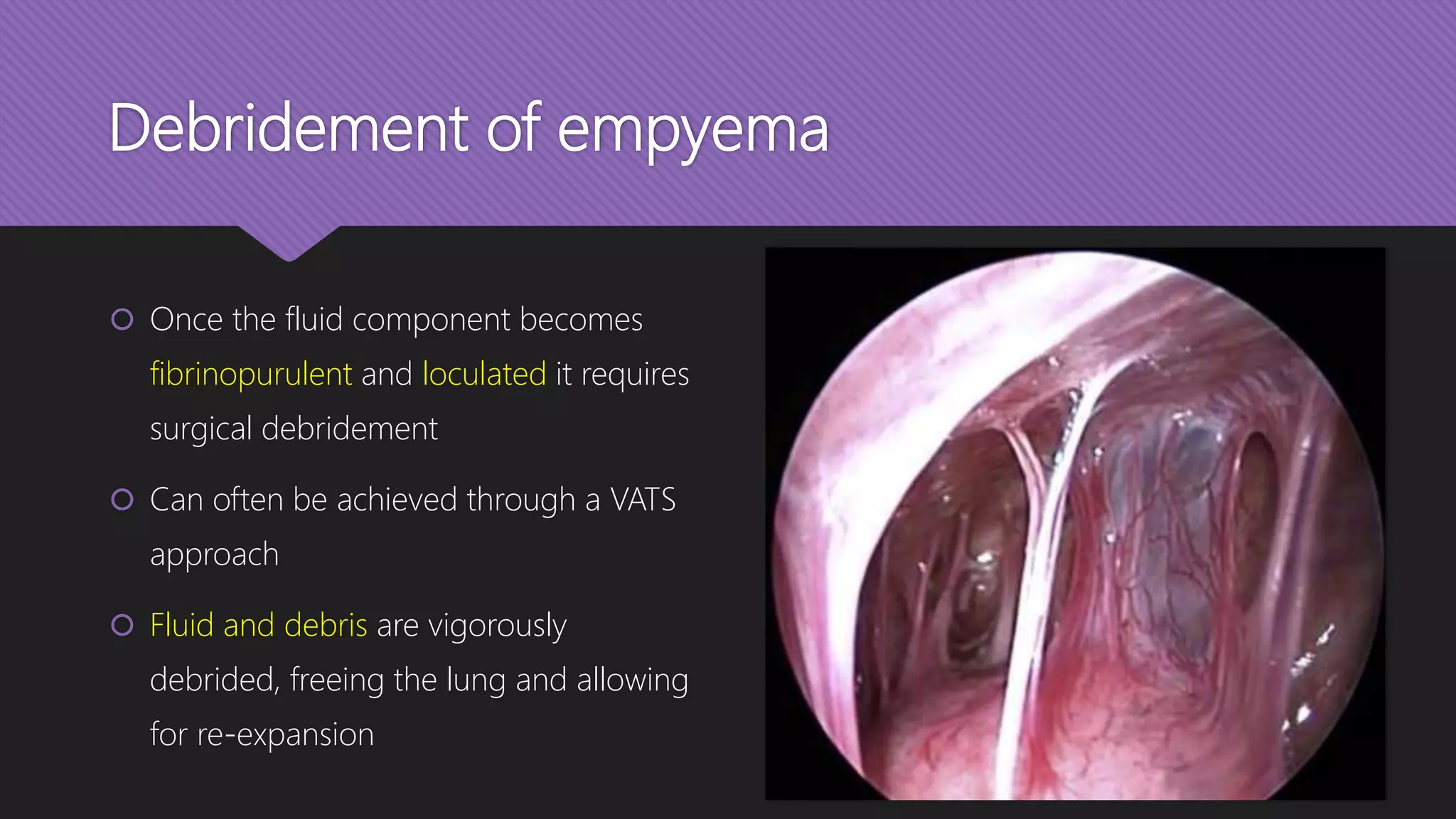
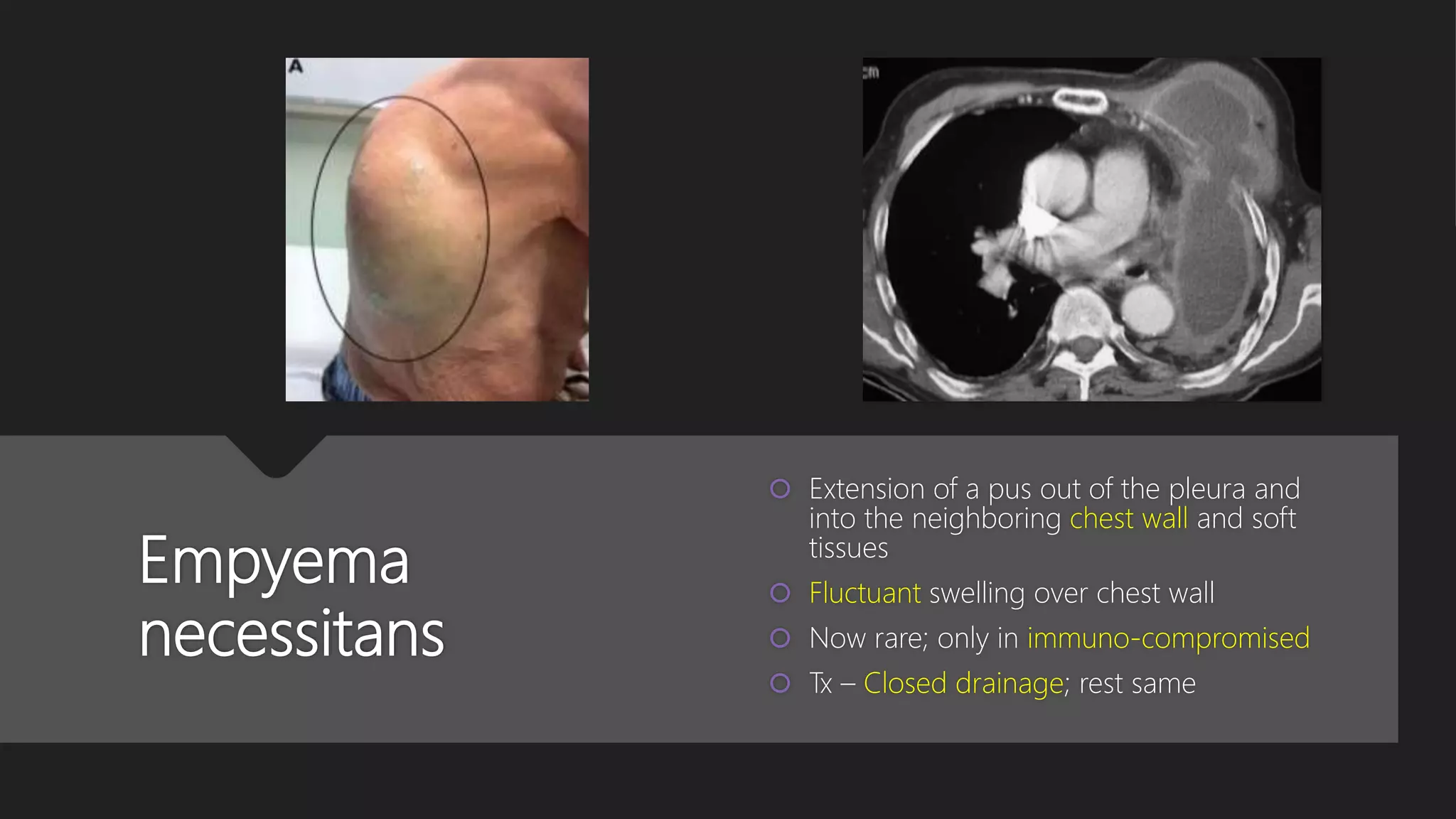
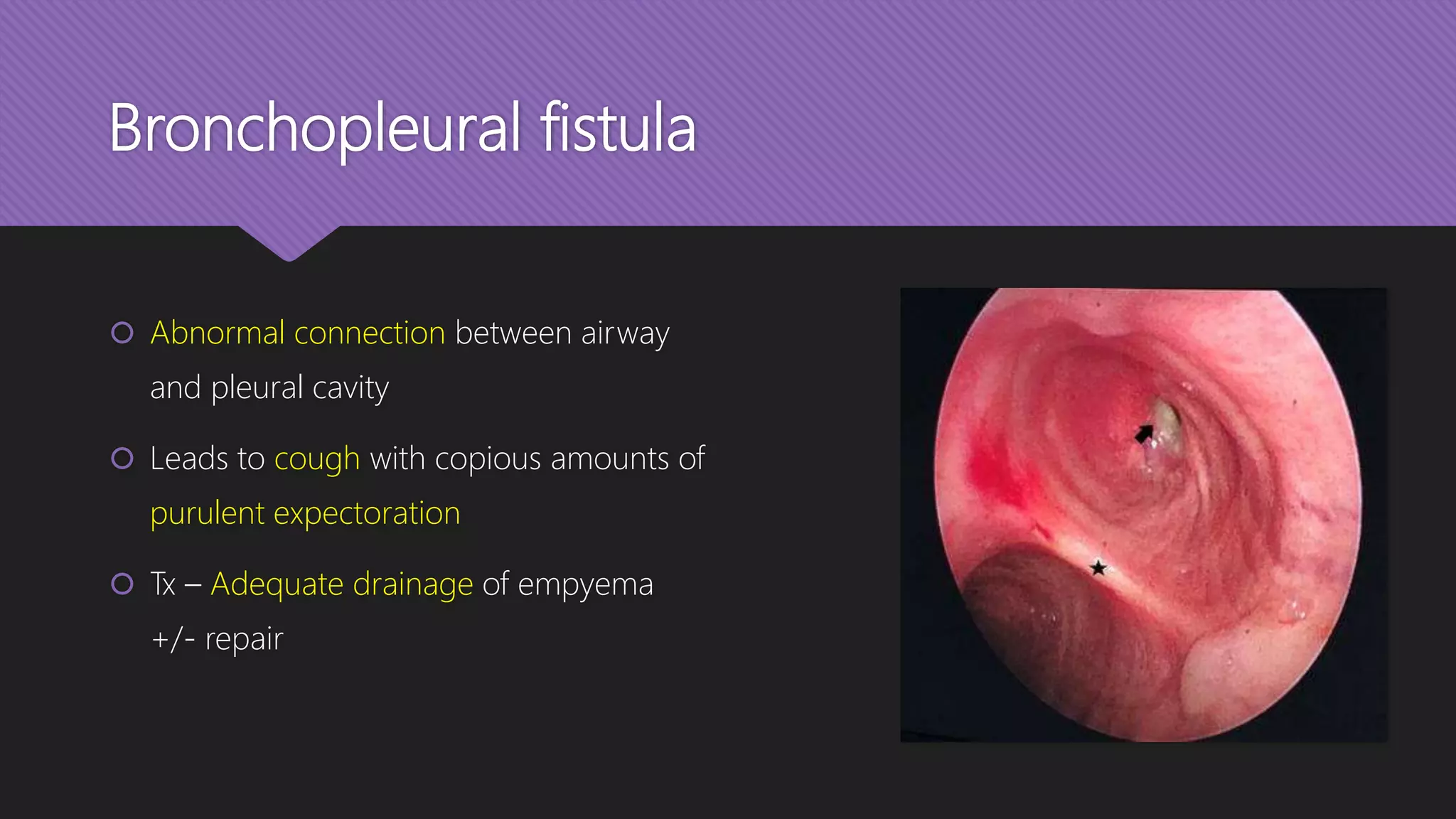
Empyema thoracis, characterized by pus in the pleural space, often follows unresolved pneumonia and can arise from various infections, trauma, or complications from thoracic surgery. It progresses through three phases: exudative, fibrino-purulent, and organizing, each requiring different diagnostic and treatment approaches, including antibiotics, drainage, and potential surgical intervention. Key clinical features include chest pain, fever, and dyspnea, with diagnosis supported through imaging and fluid analysis.