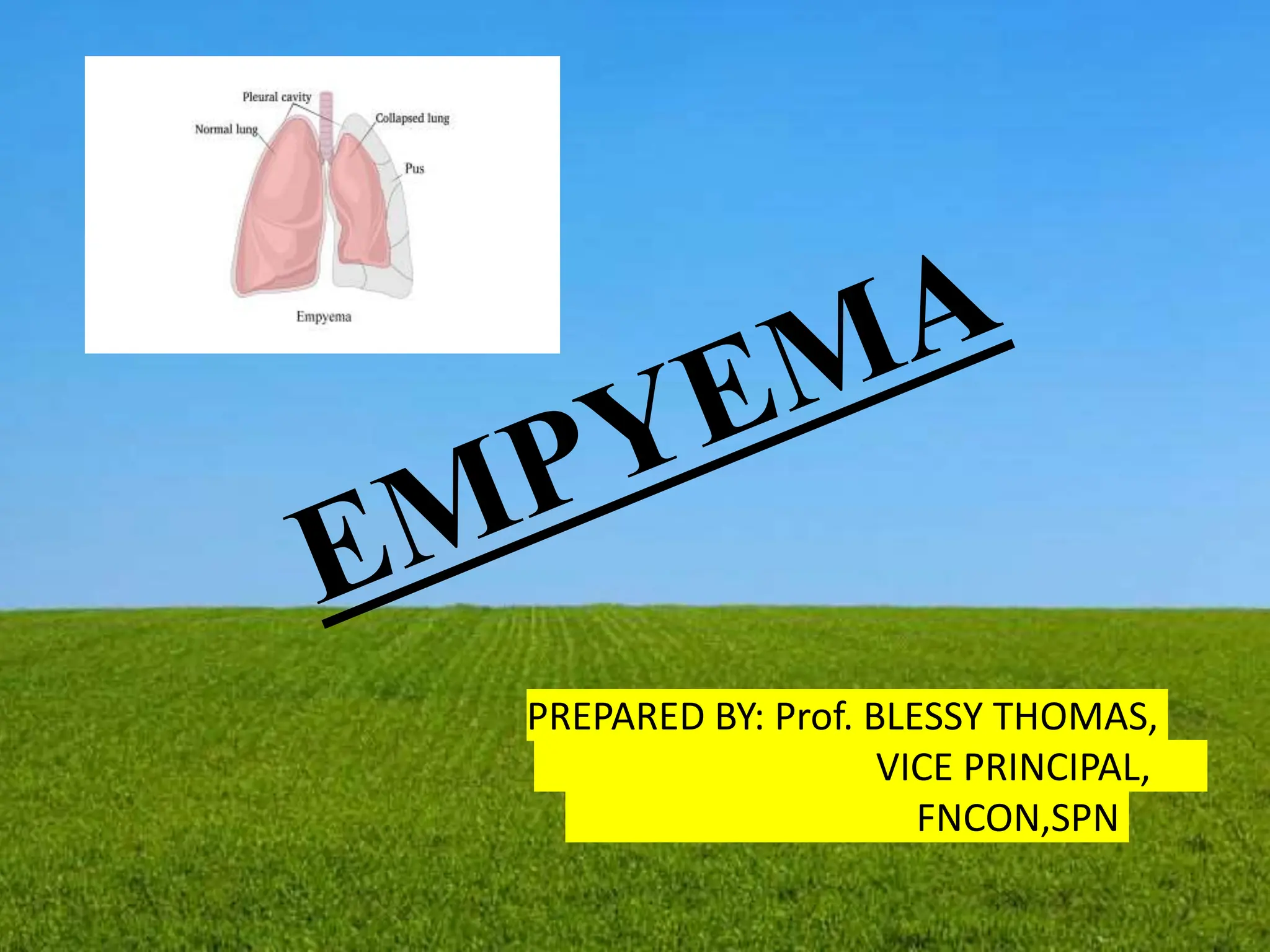
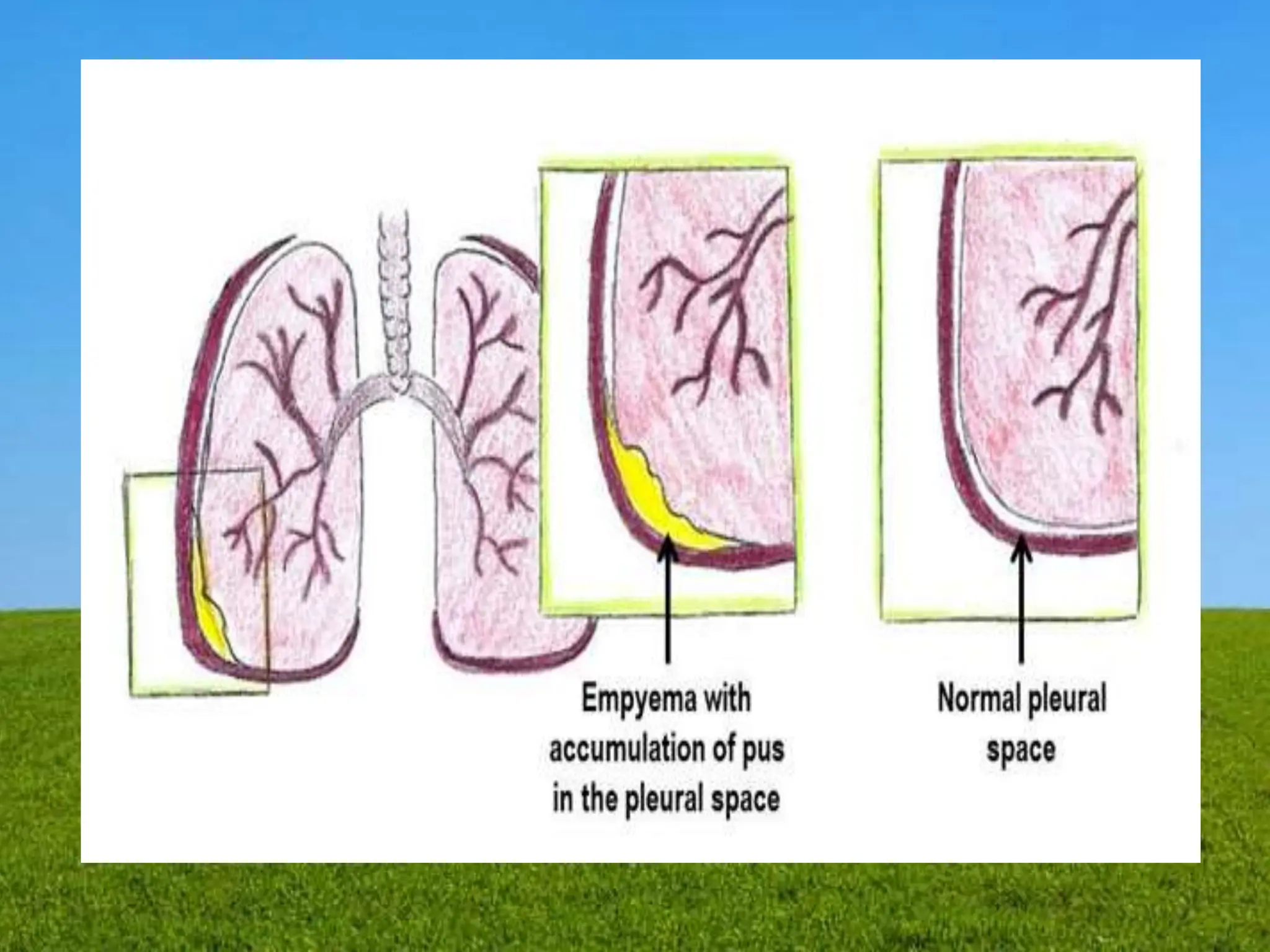
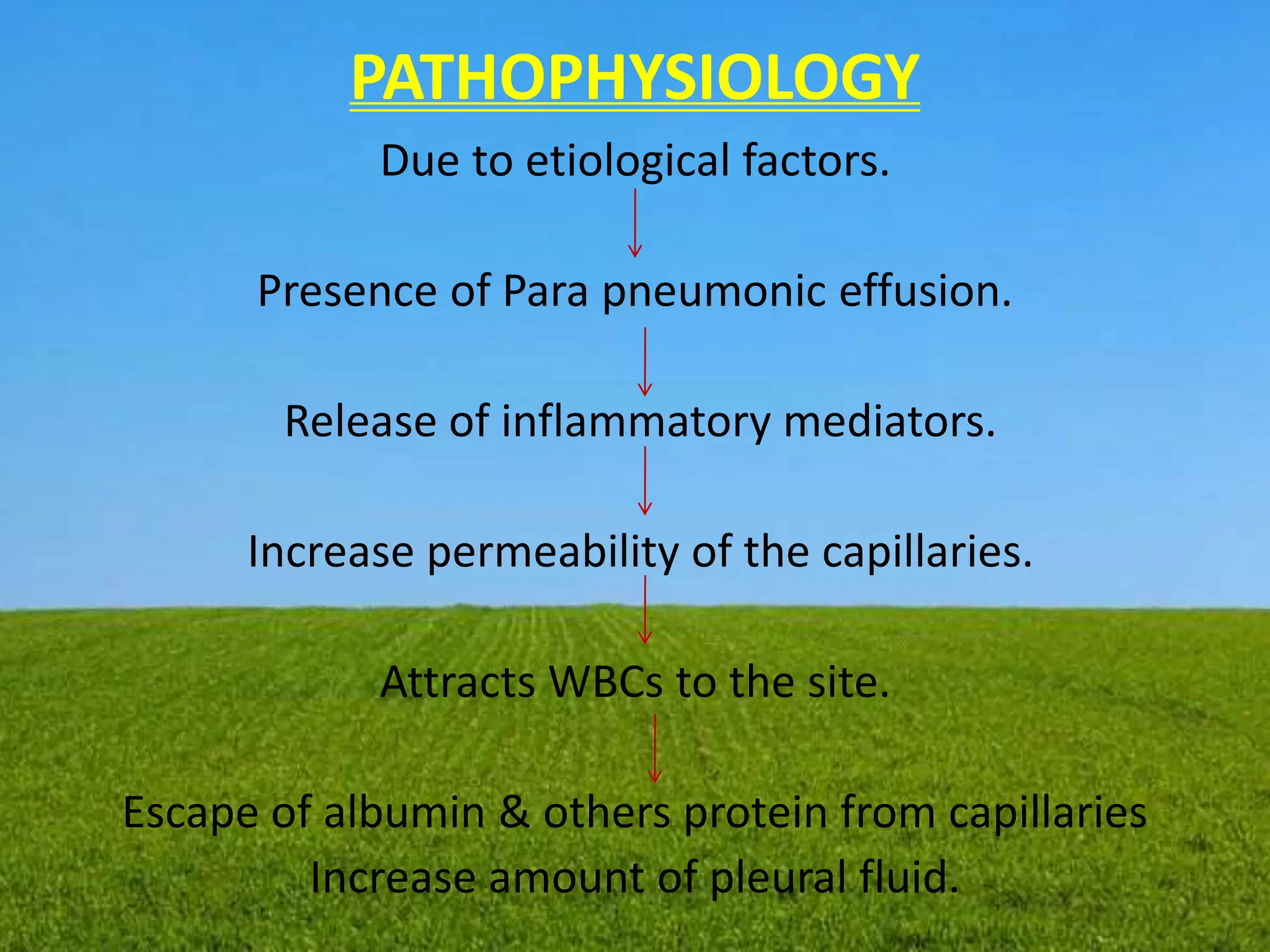
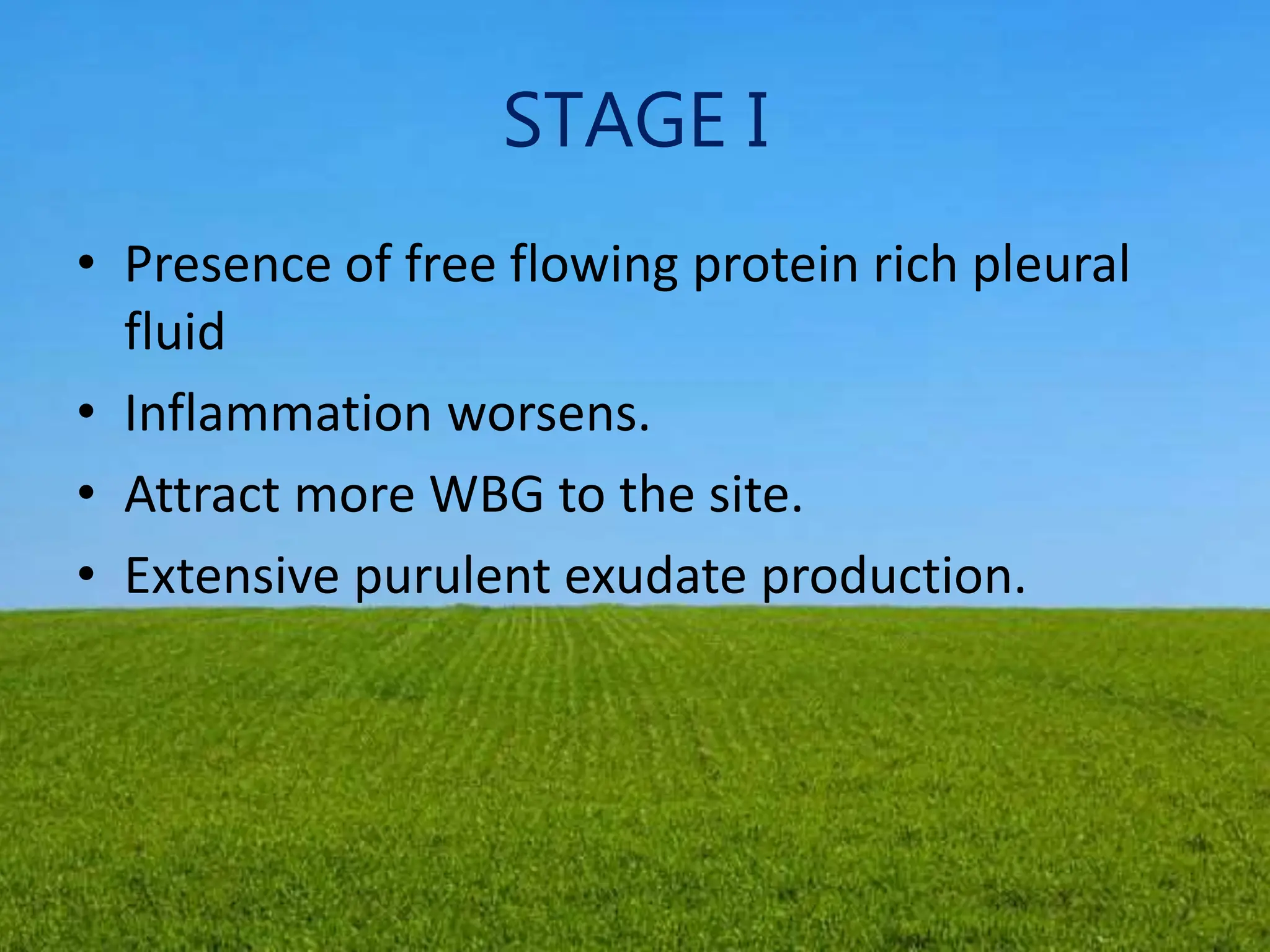
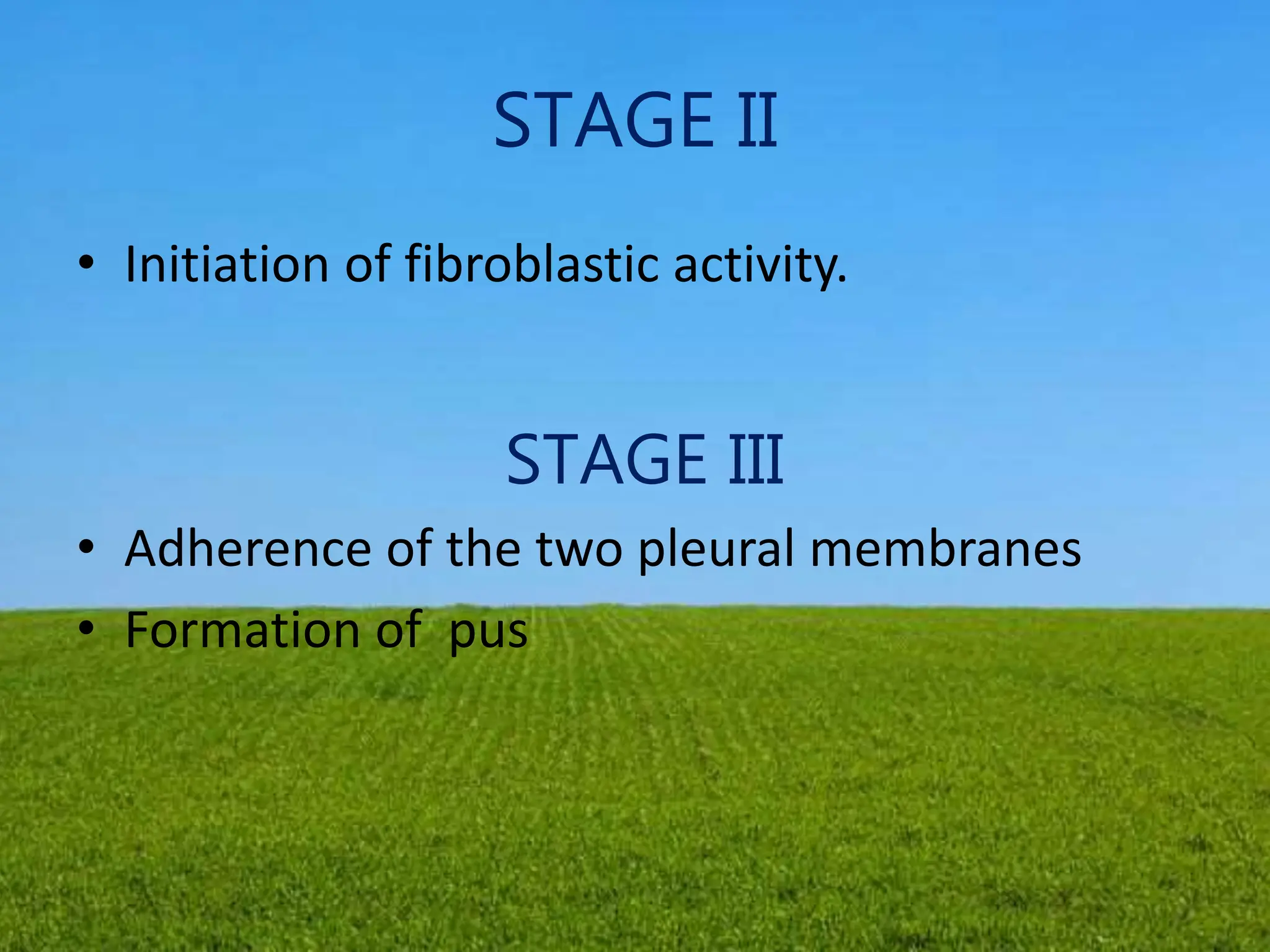
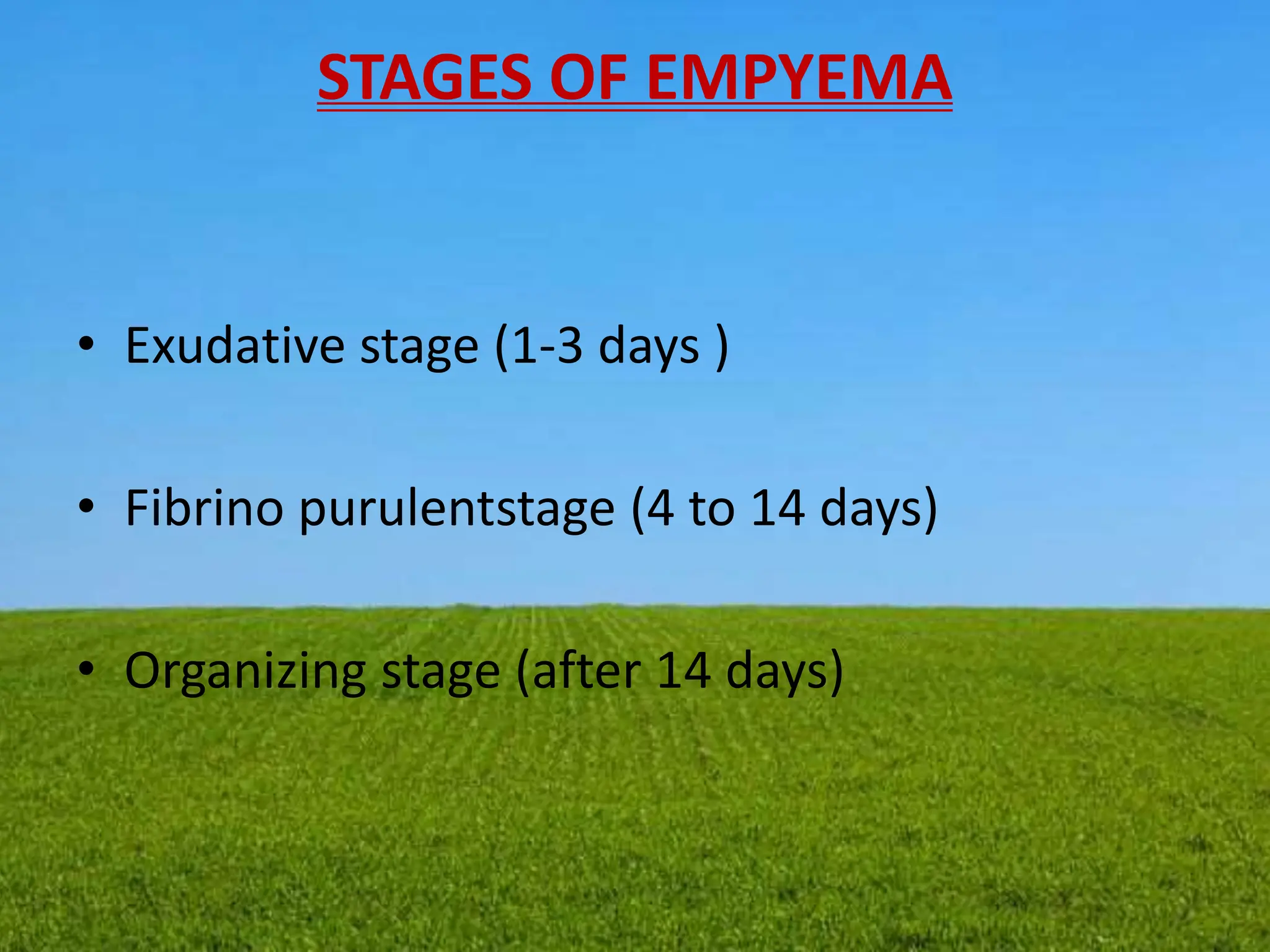
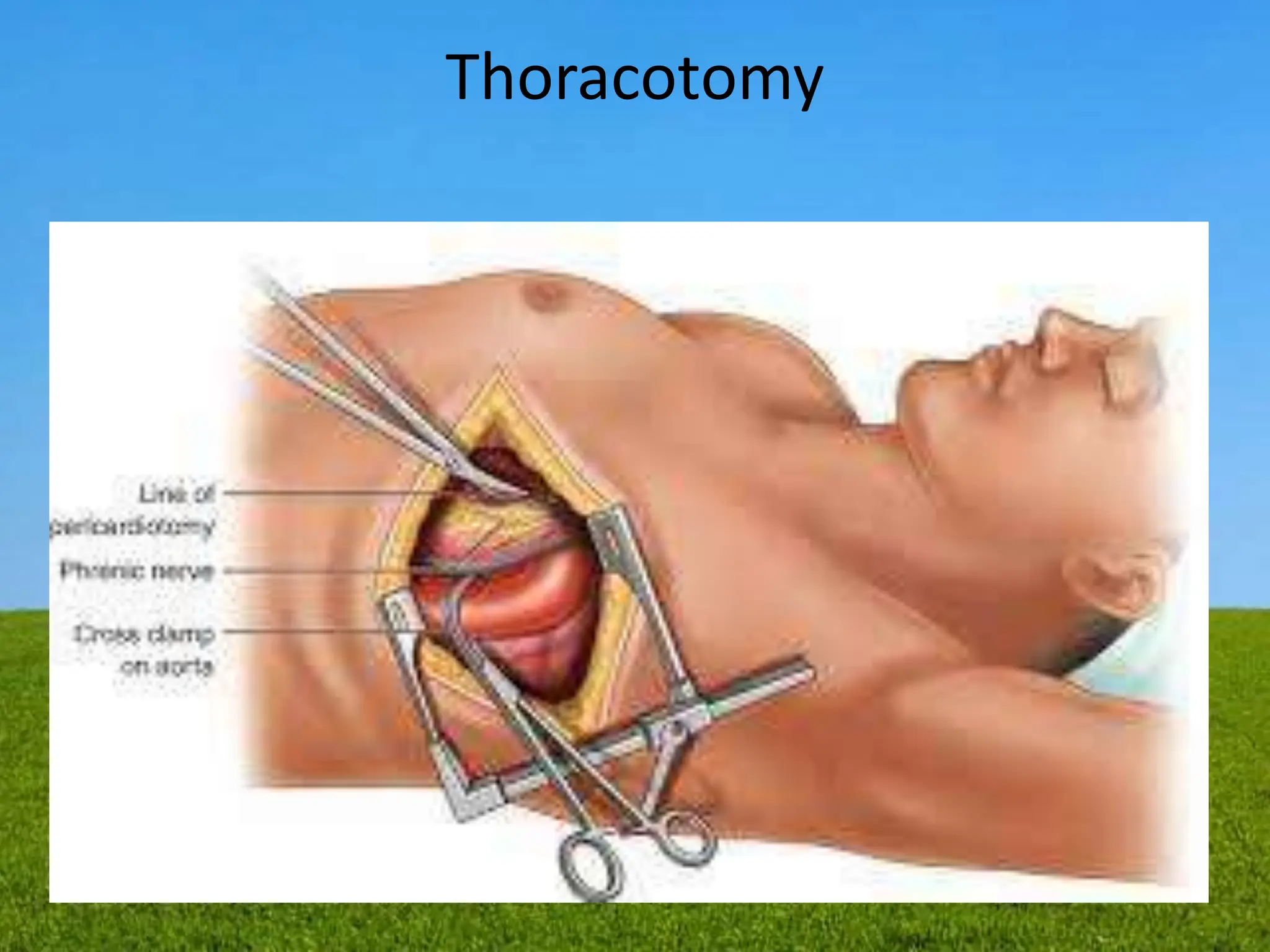
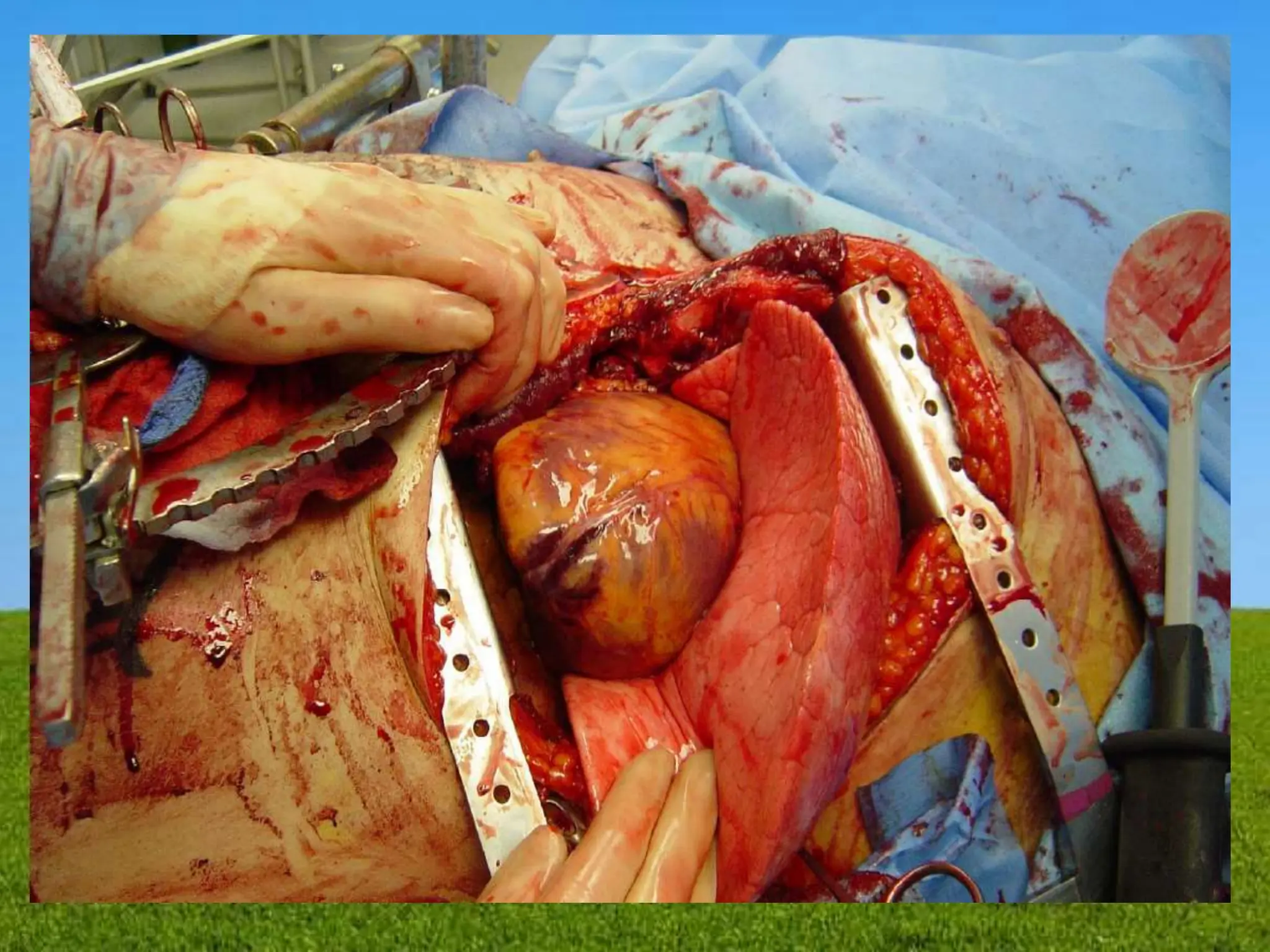
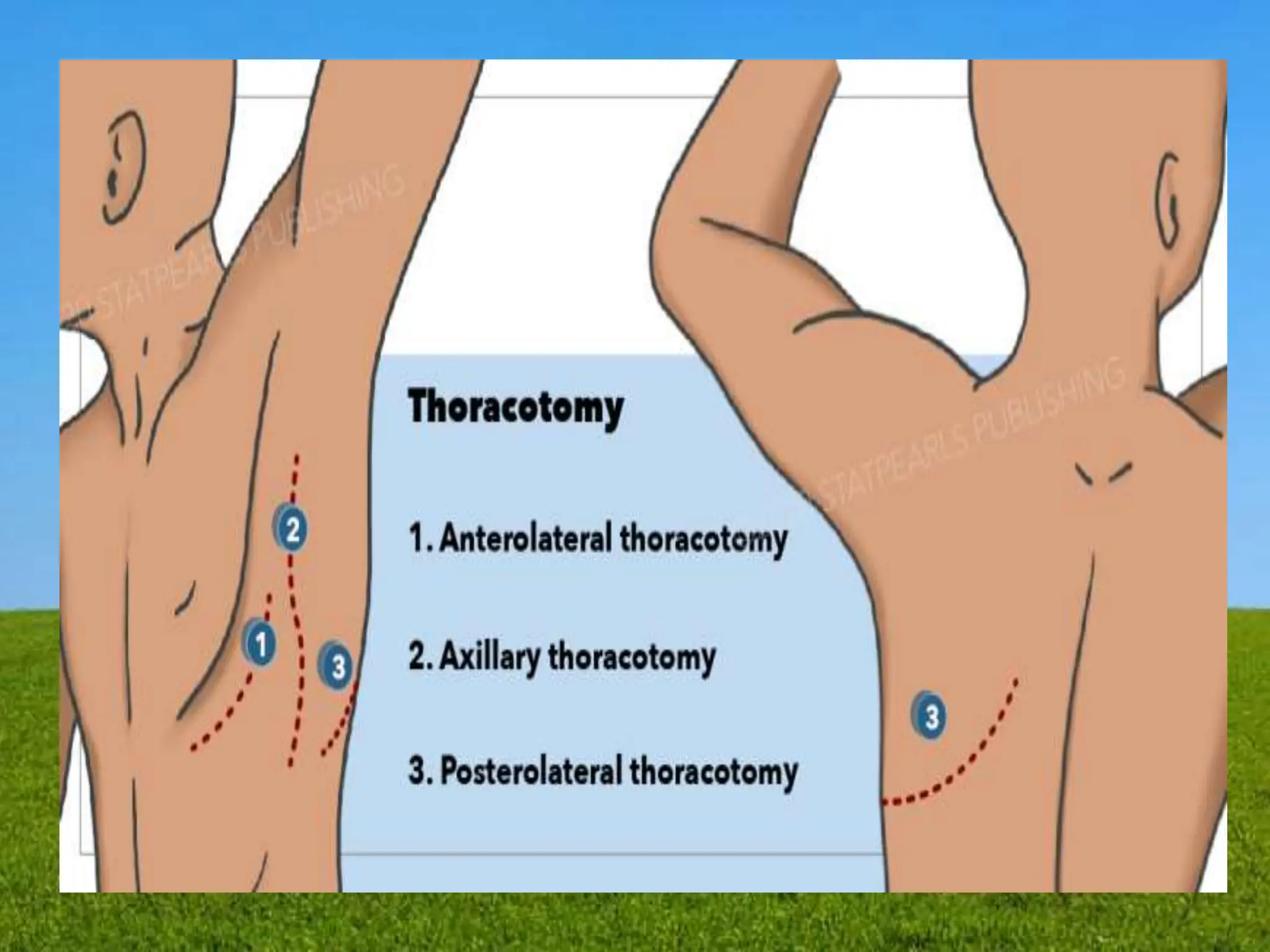
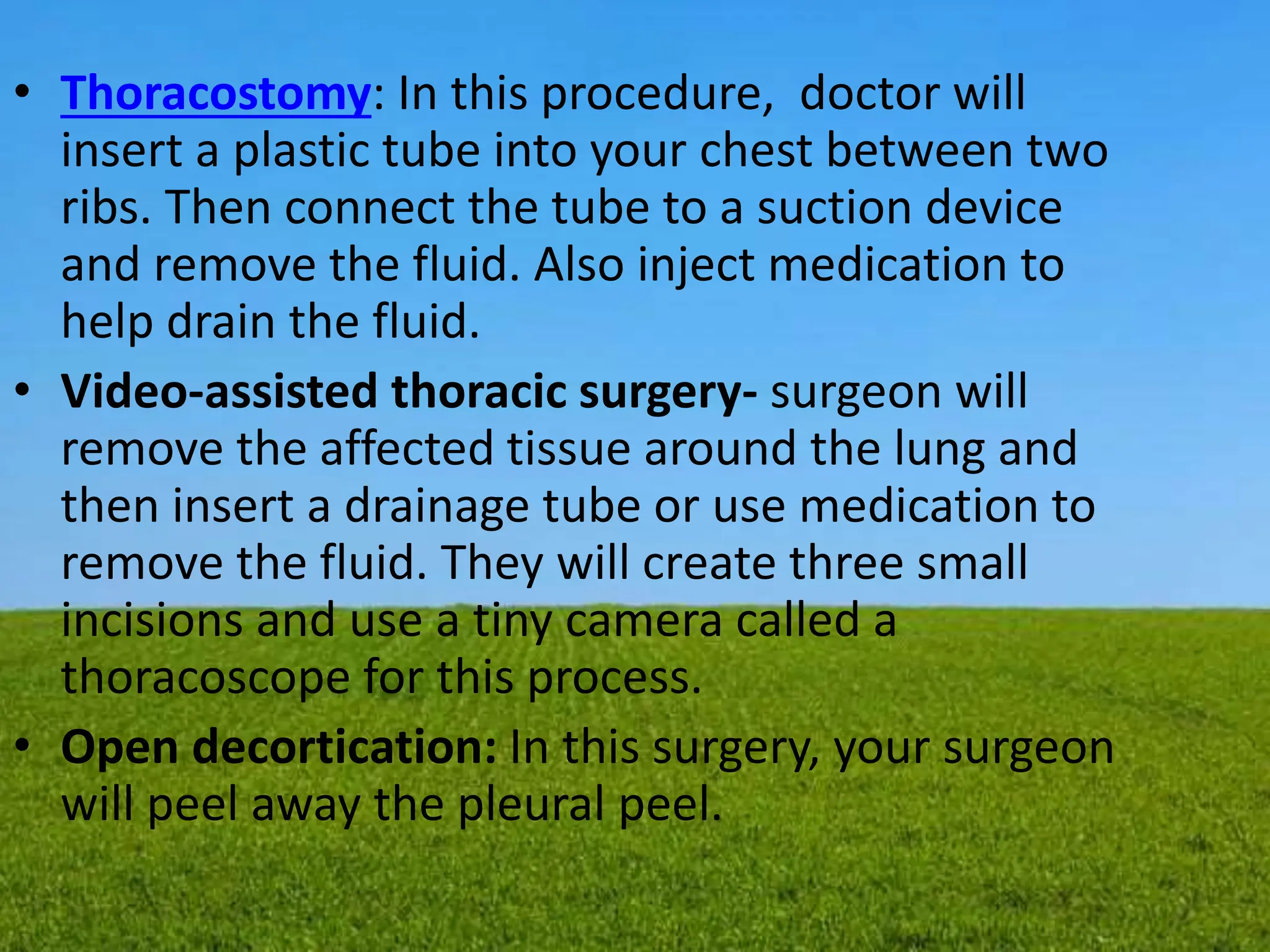
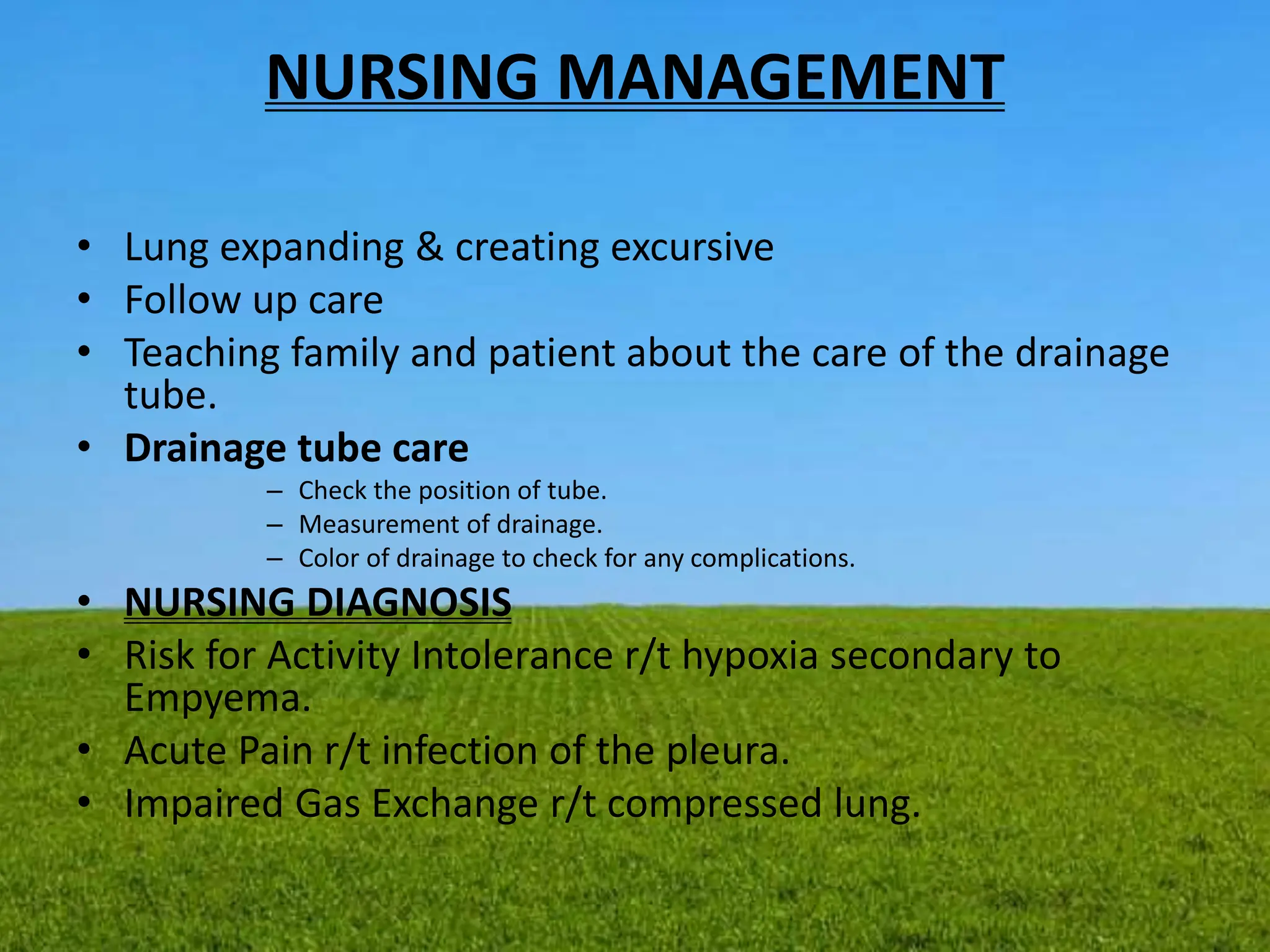
Empyema, also known as pyothorax, is the accumulation of pus in the pleural space, often following pneumonia and requiring drainage via needle or surgery. The condition has two stages: simple empyema, which is characterized by free-flowing pus, and complex empyema, where loculated infections lead to severe complications. Management includes drainage, antibiotics, and potential surgical interventions, with careful monitoring of symptoms to prevent serious complications like sepsis or pneumothorax.