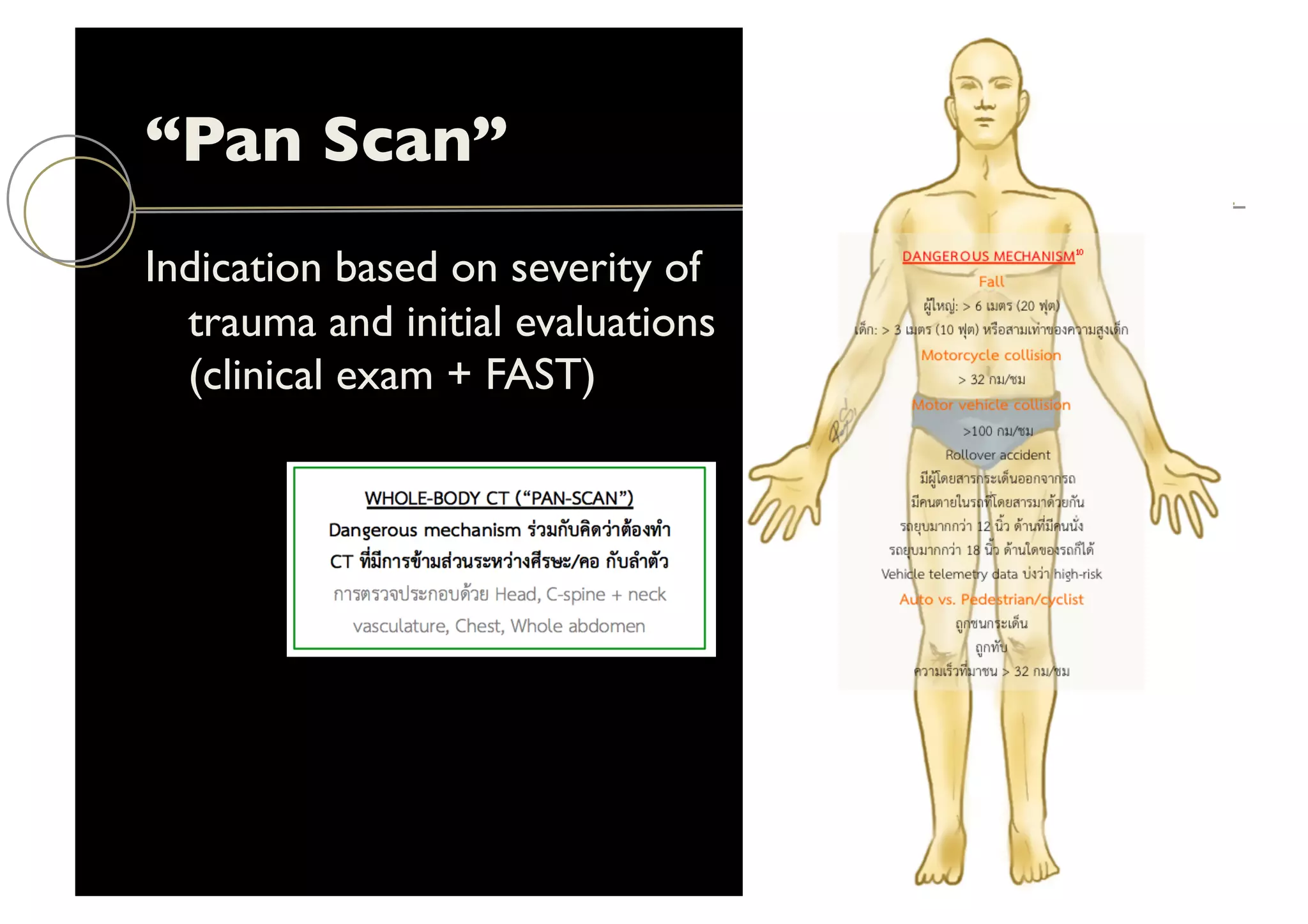
The document presents an update on imaging techniques in emergency radiology, particularly focusing on pan-scan CT for trauma assessment and CTA for active bleeding. It highlights the efficacy of pan-scan CT in high-severity trauma cases, the predictive value of the CTA spot sign in cases of primary intracerebral hemorrhage, and the role of multiphase CTA in evaluating collateral circulation for acute stroke management. Recommendations for trauma protocols and the importance of accurate diagnosis in bleeding sources are emphasized.
















![Can We Predict Hematoma
Expansion?
“CTA spot sign”
Intrahematoma contrast following CTA
Represents site of active extravasation in early ICH
Spot sign growth =
[spot vol (delayed) – spot vol (initial)]
elapsed time
Dowlatshahi D, et al. Stroke 2014;45:277
Image credit: smh.com.au](https://image.slidesharecdn.com/handout20151007kkuemergencyctupdates-151006173353-lva1-app6891/75/Emergency-CT-Updates-18-2048.jpg)