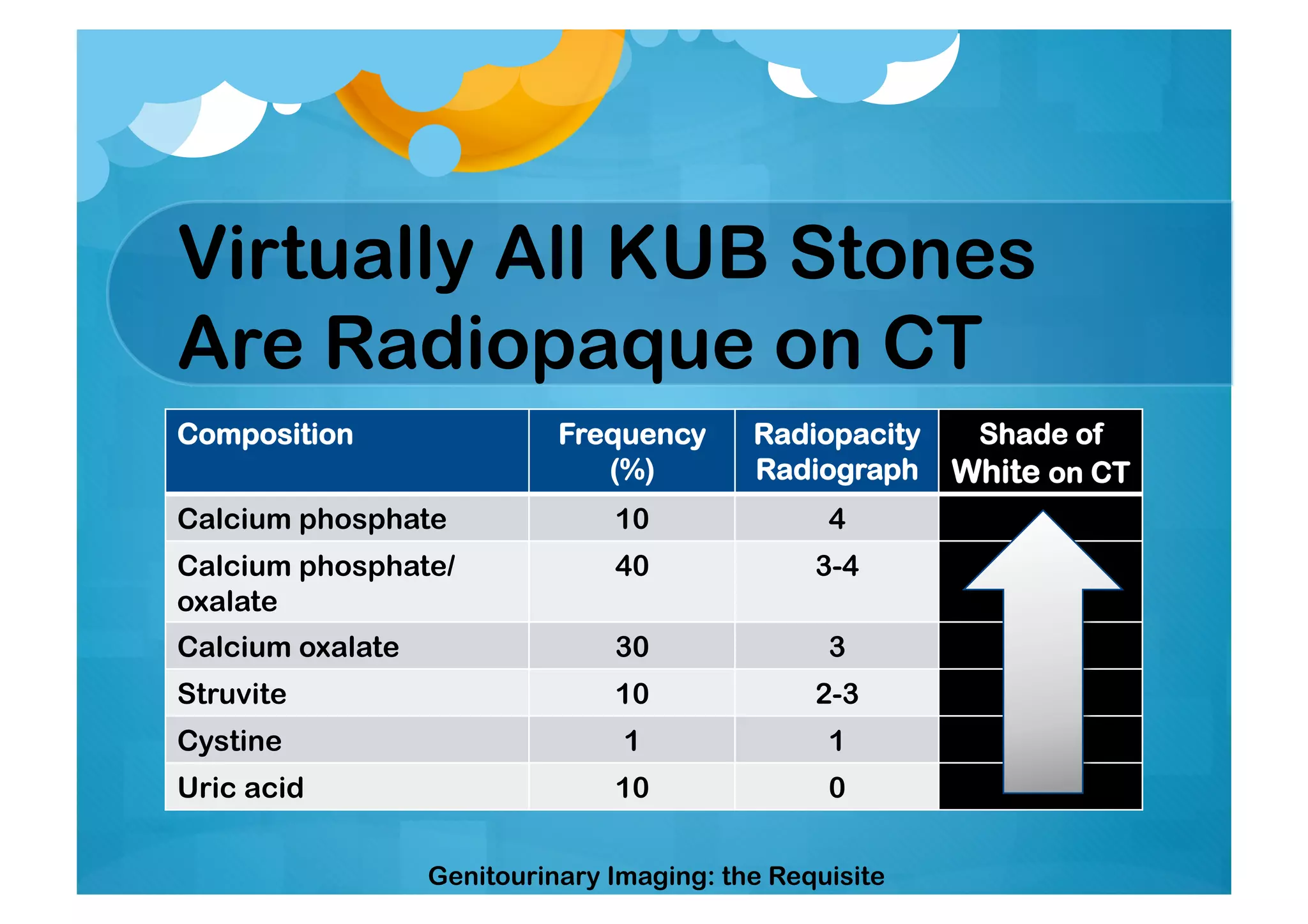
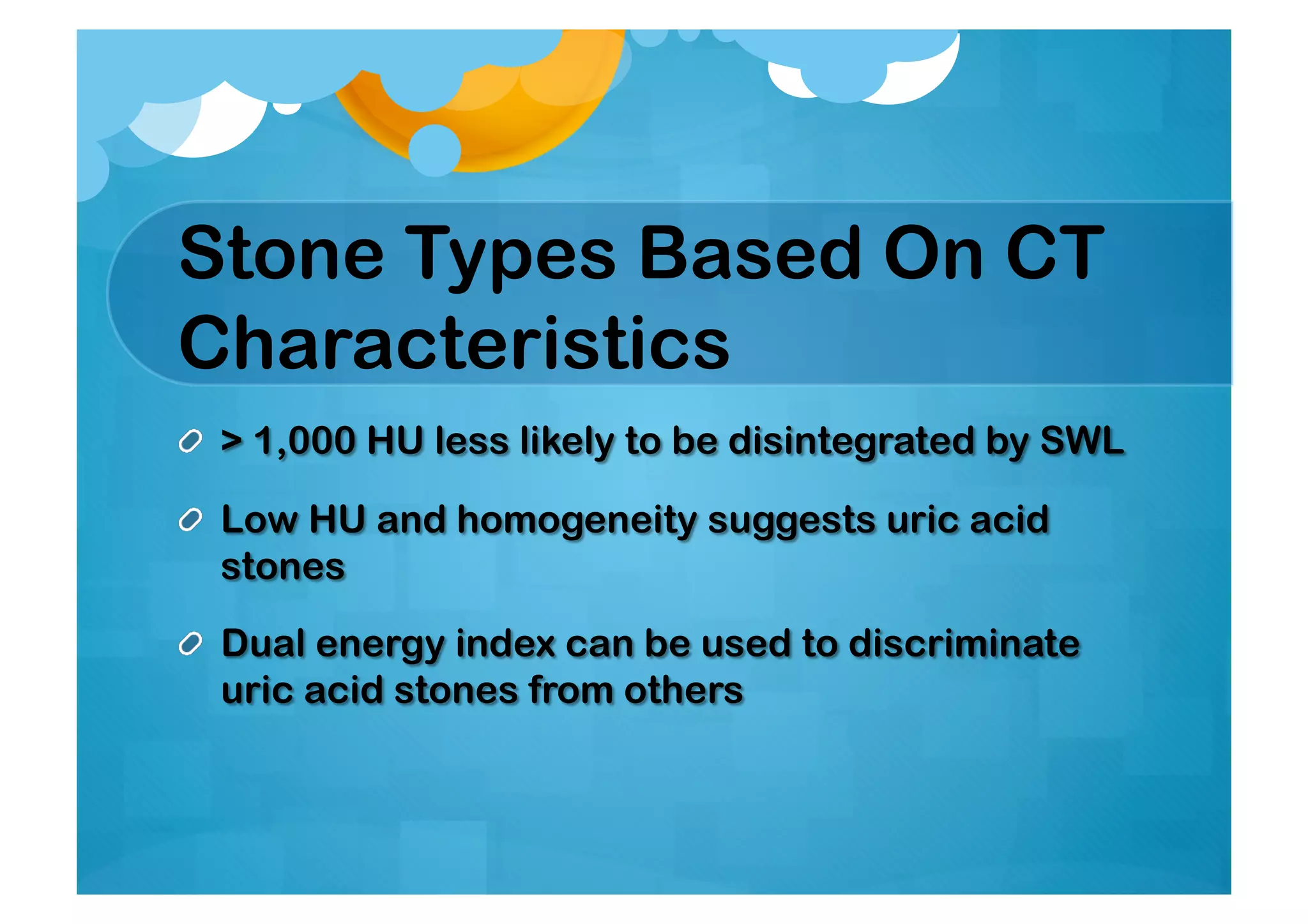
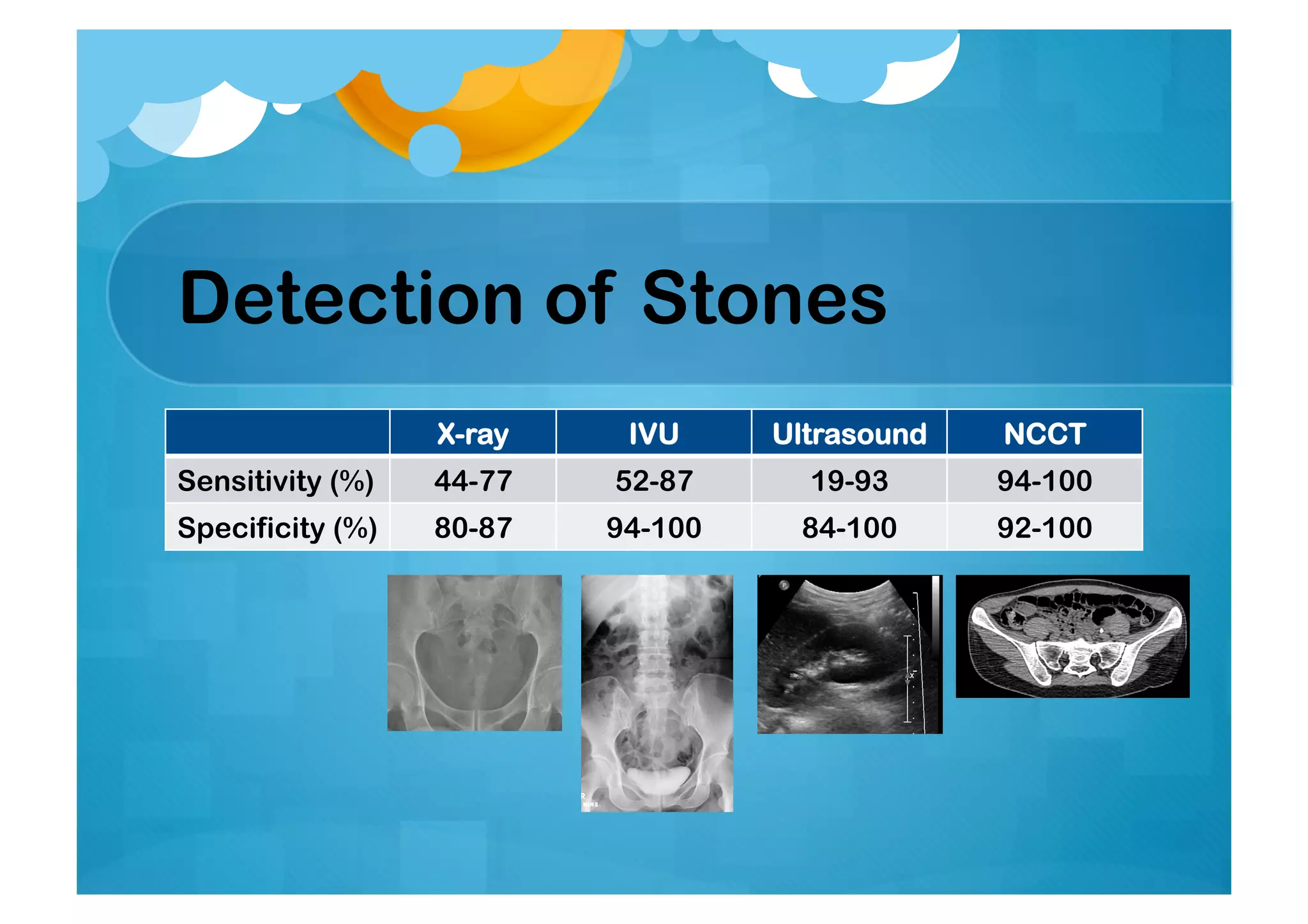
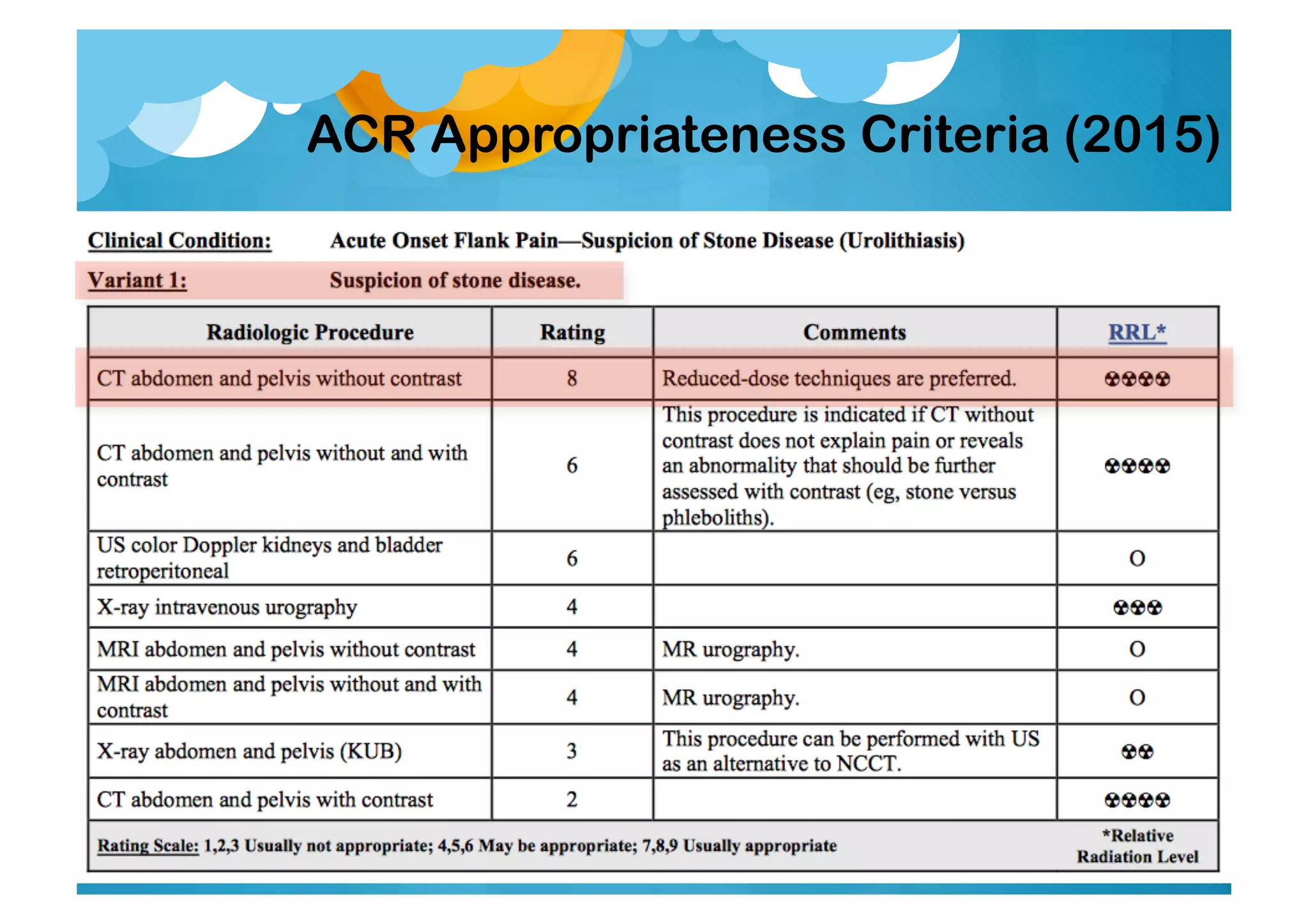
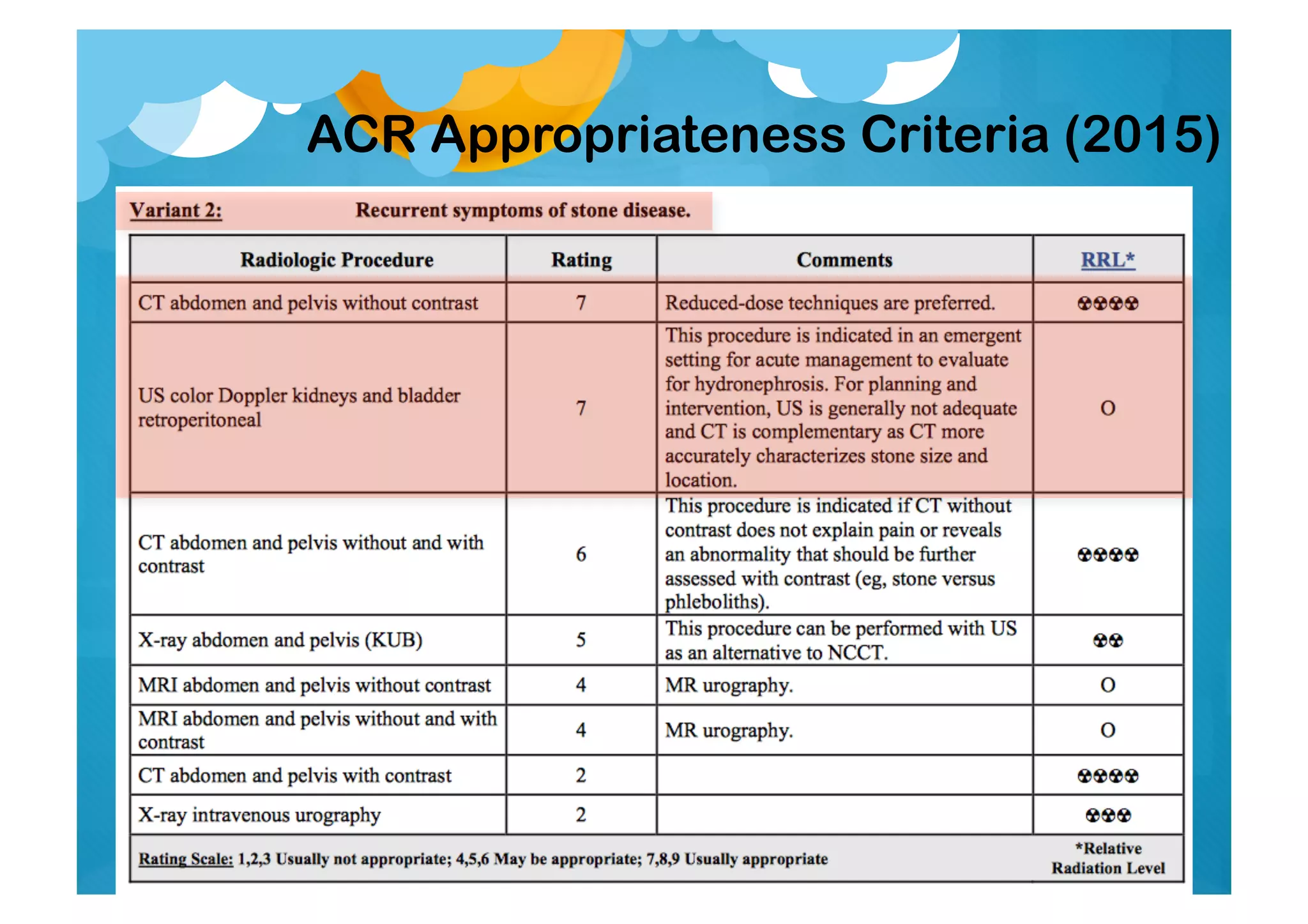
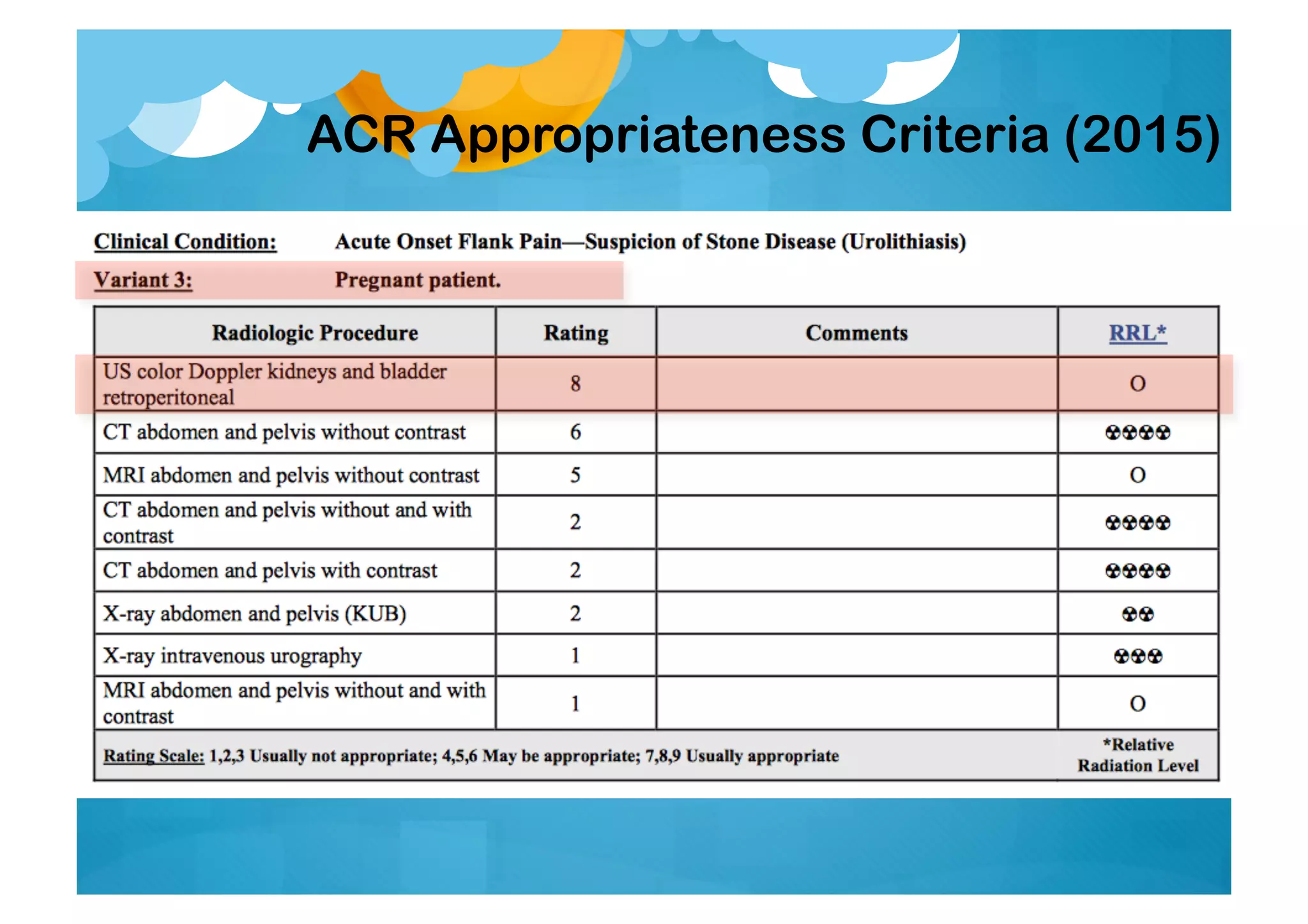
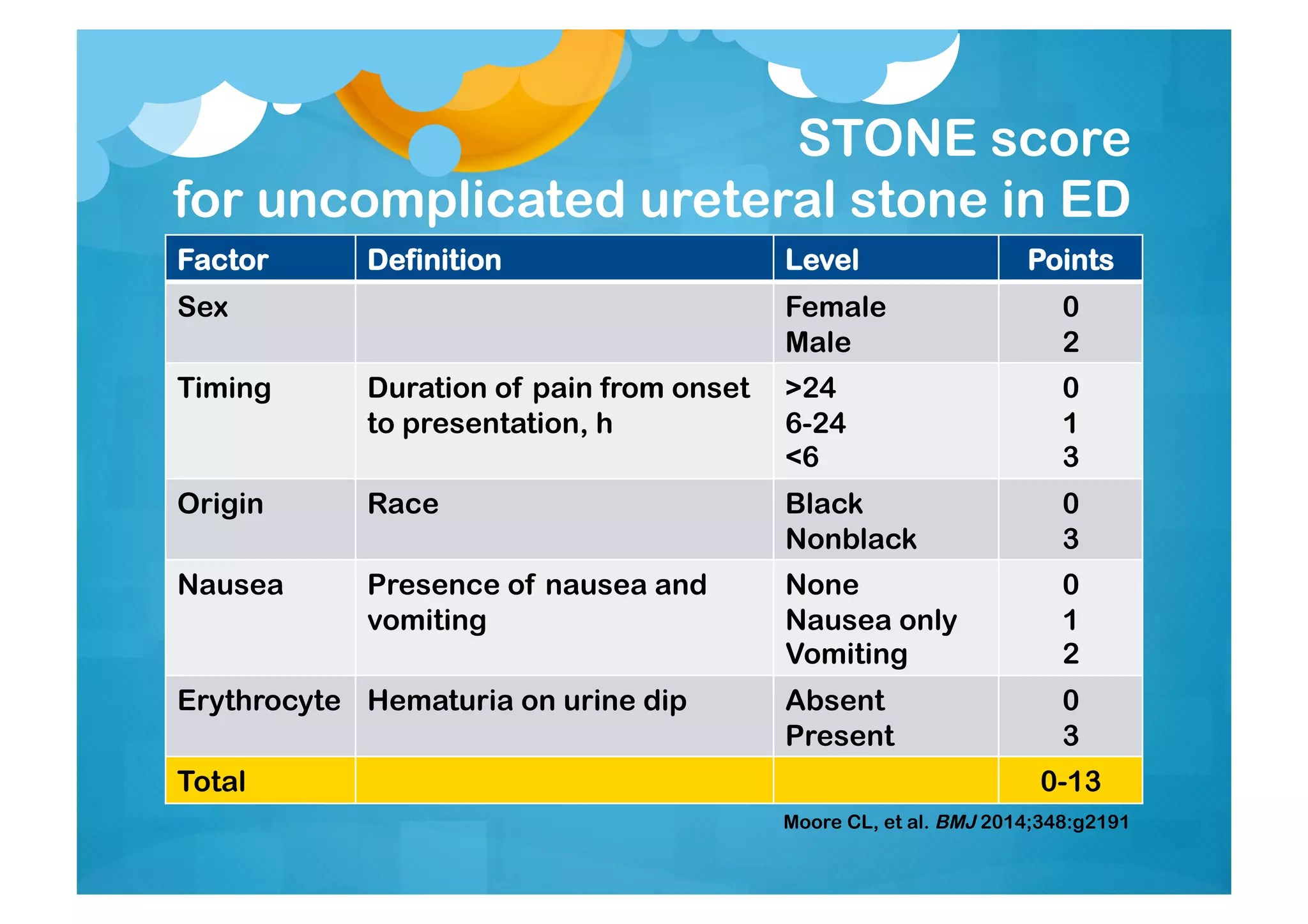
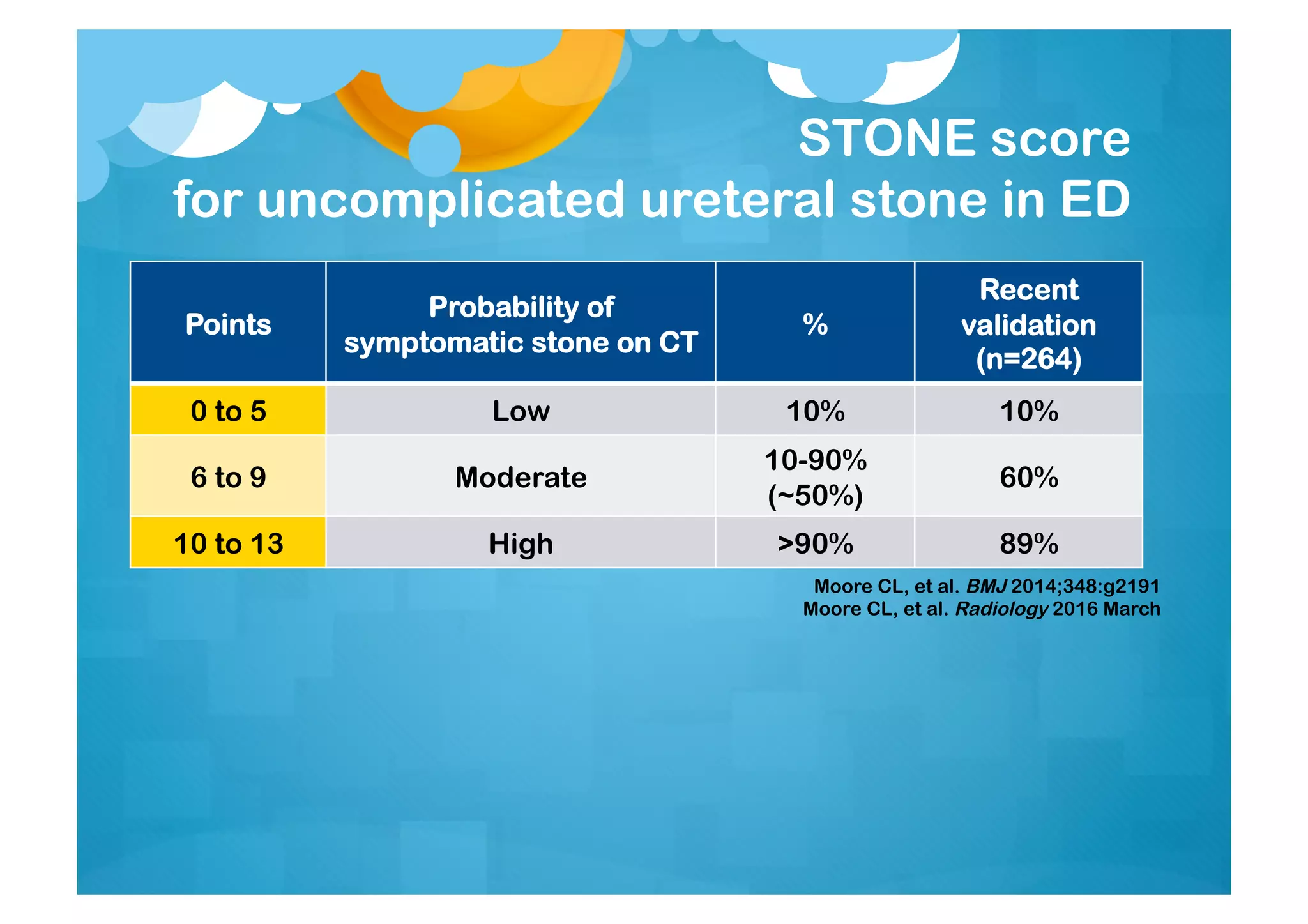
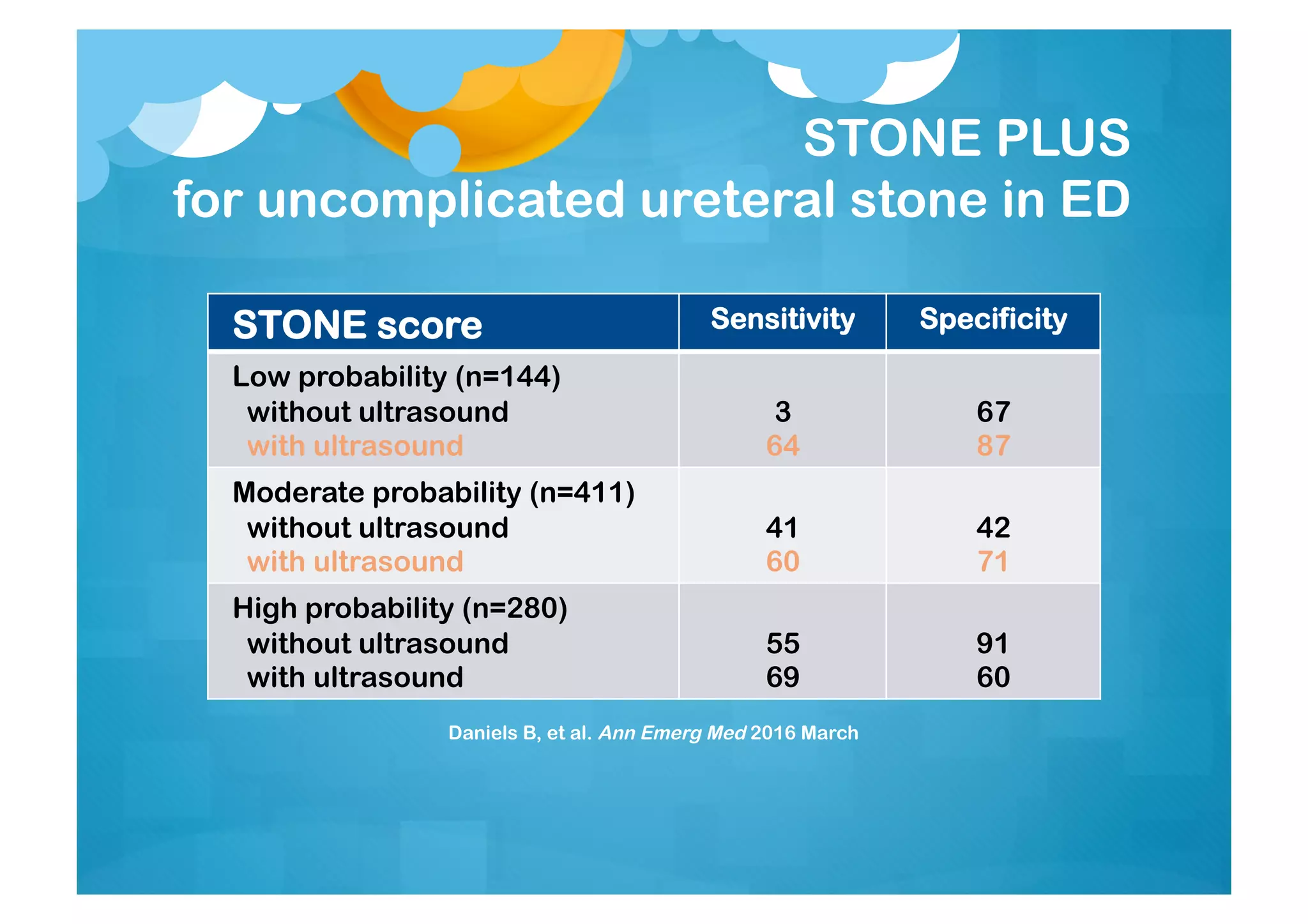
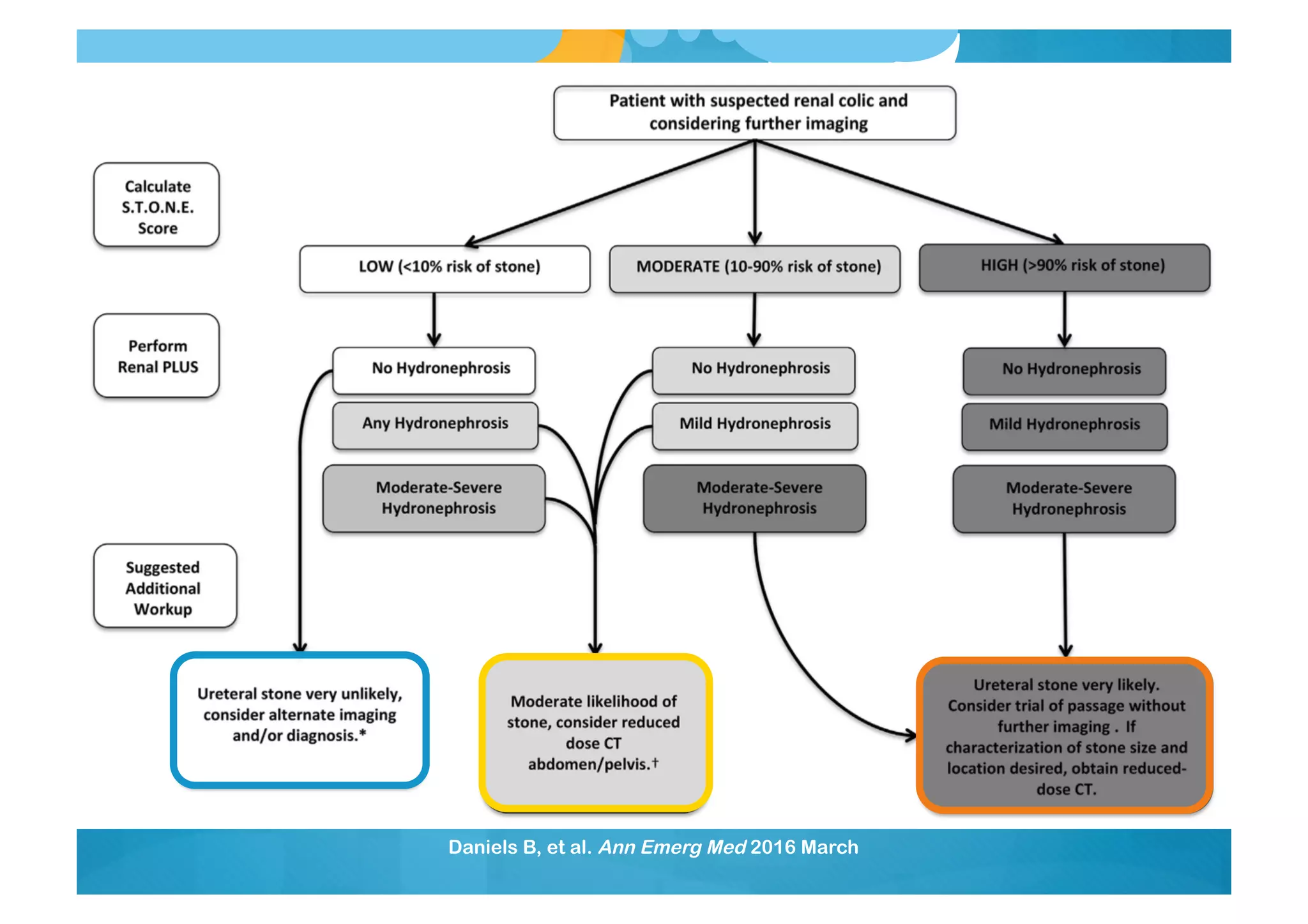
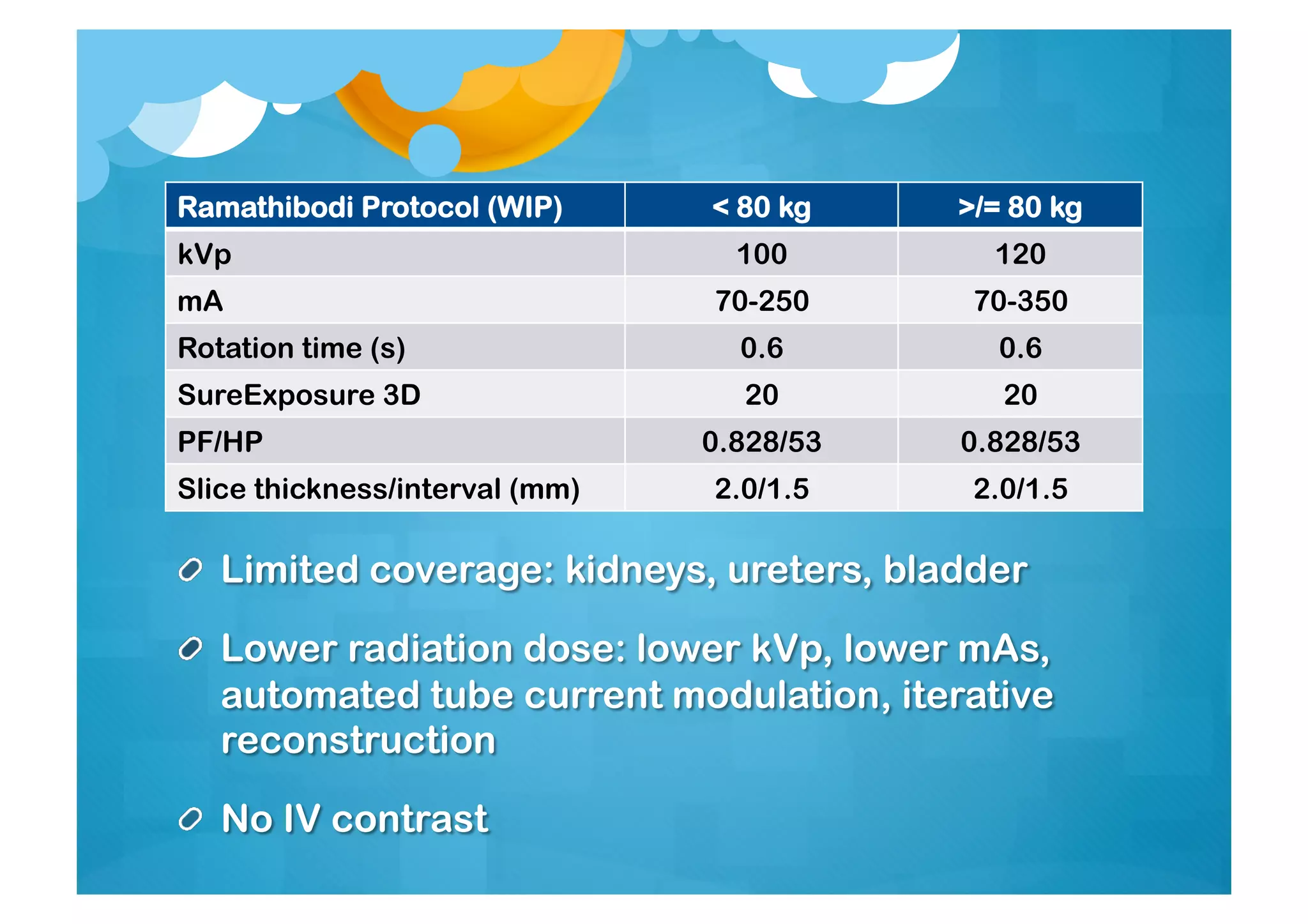
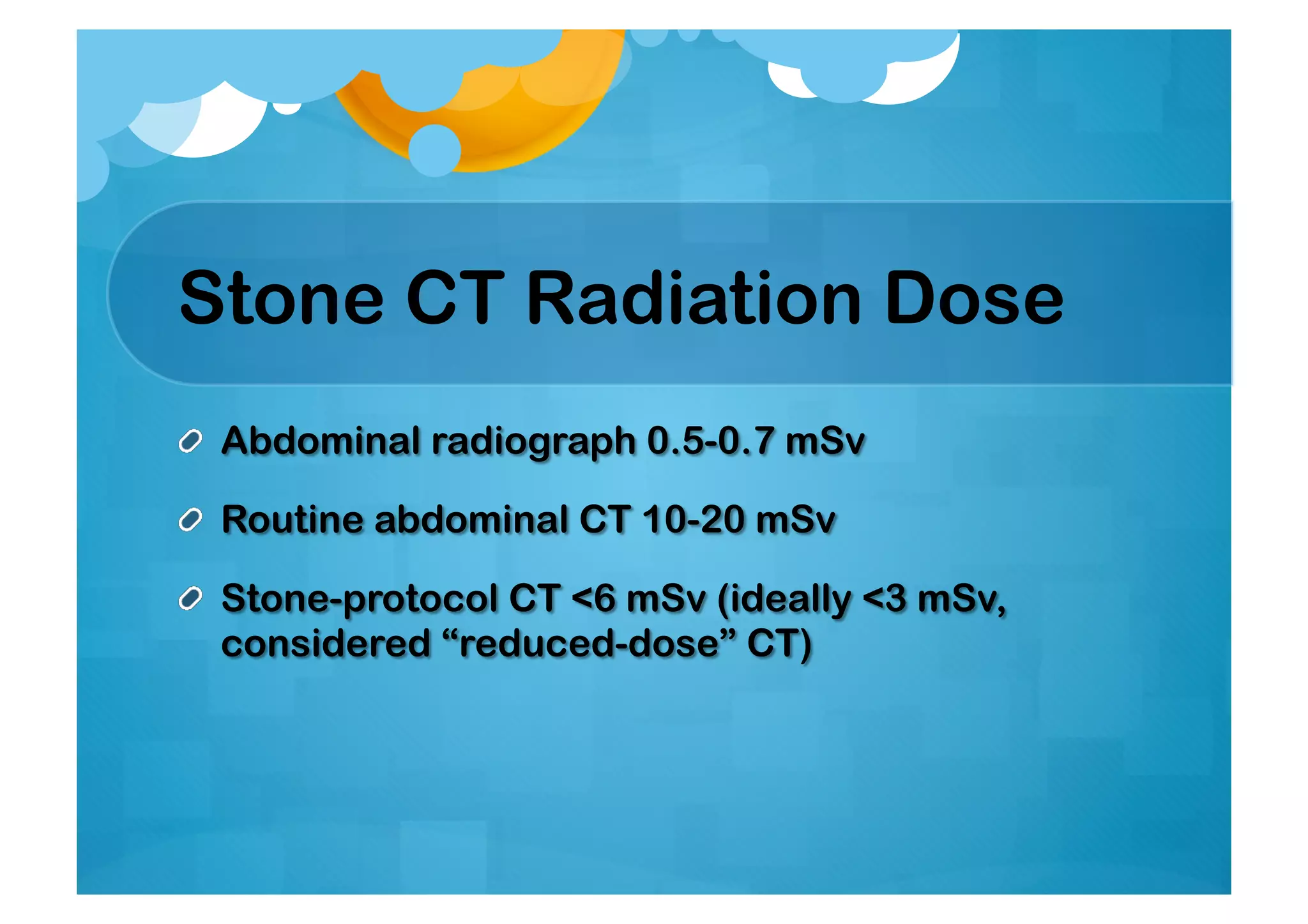
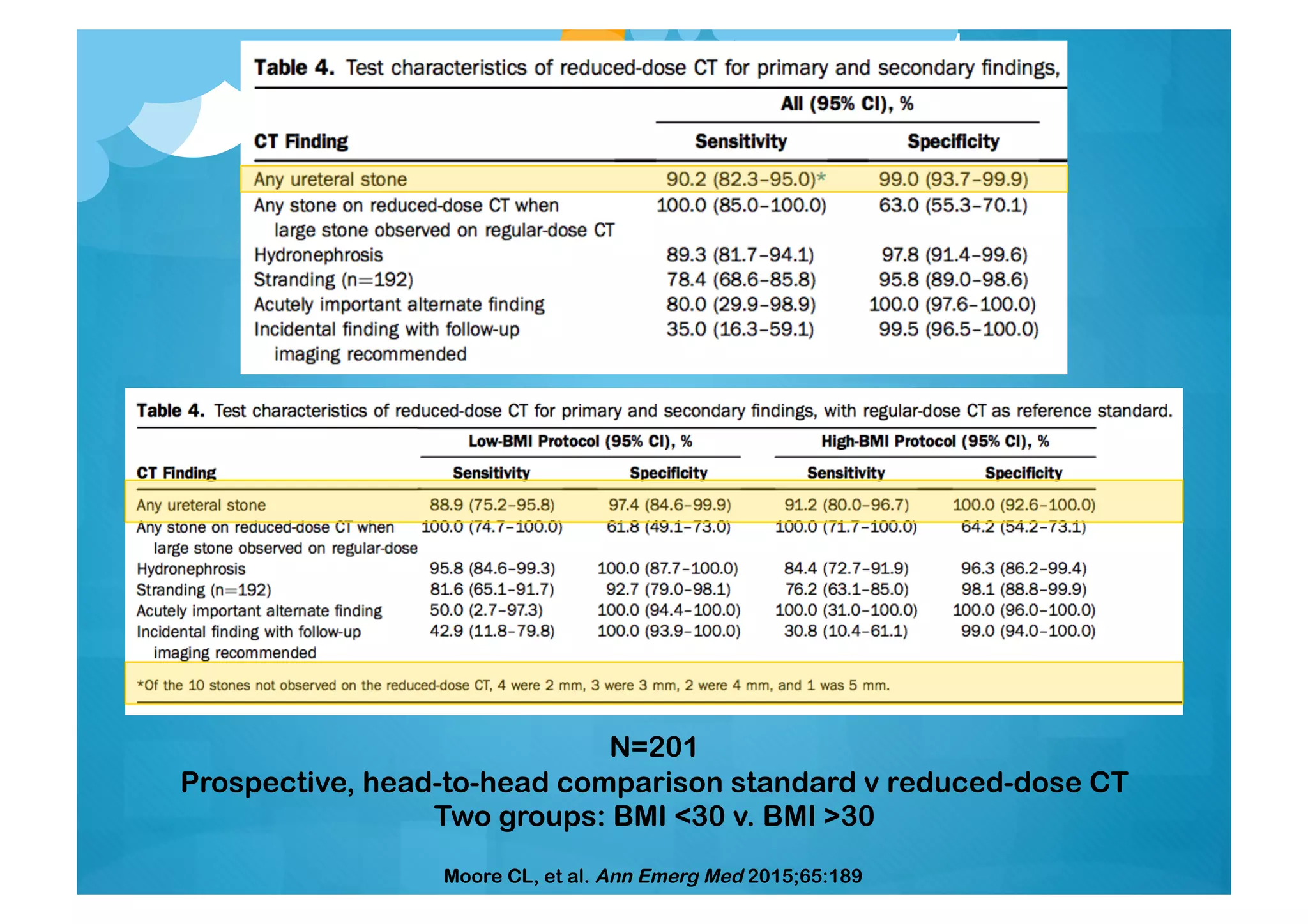
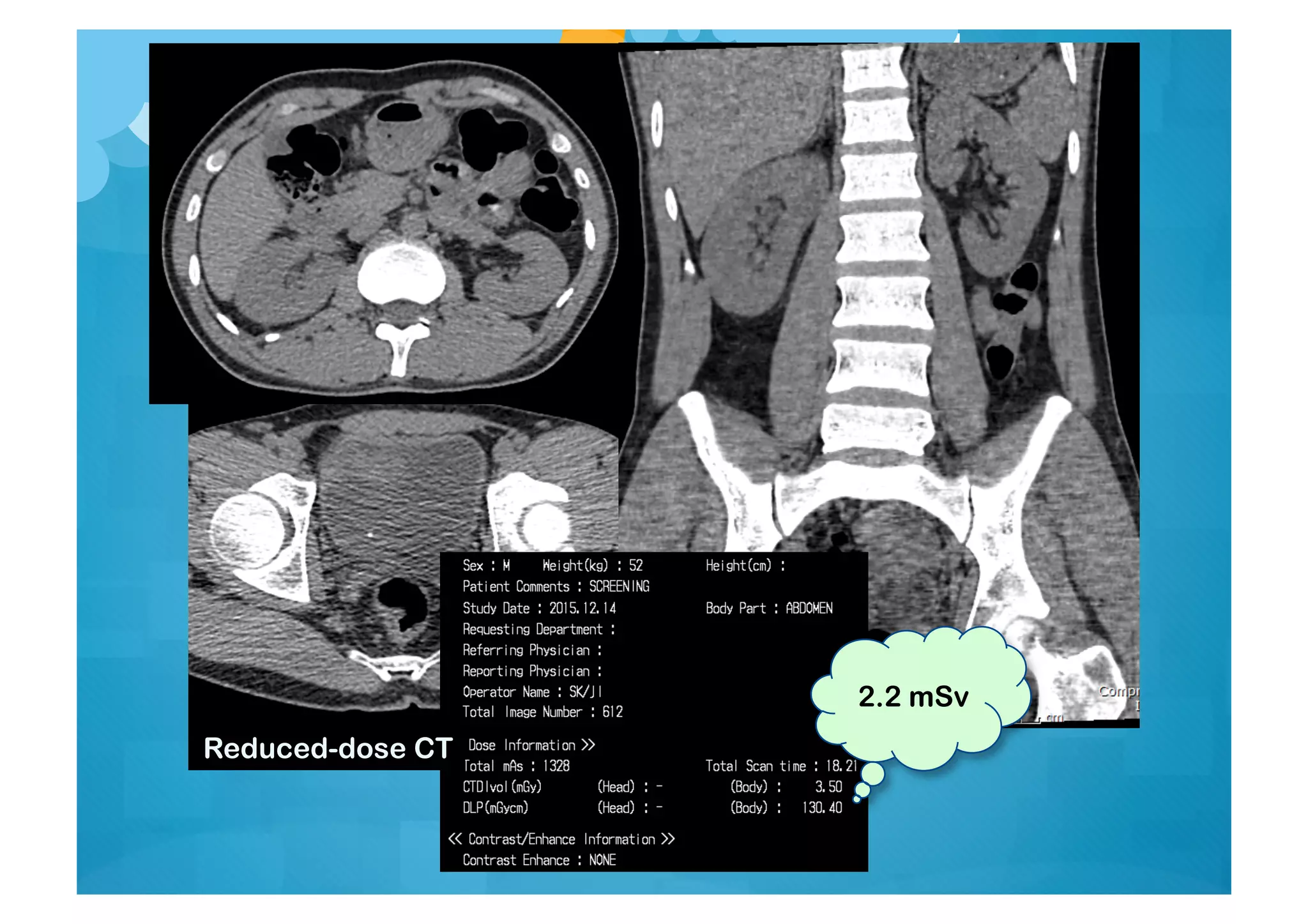
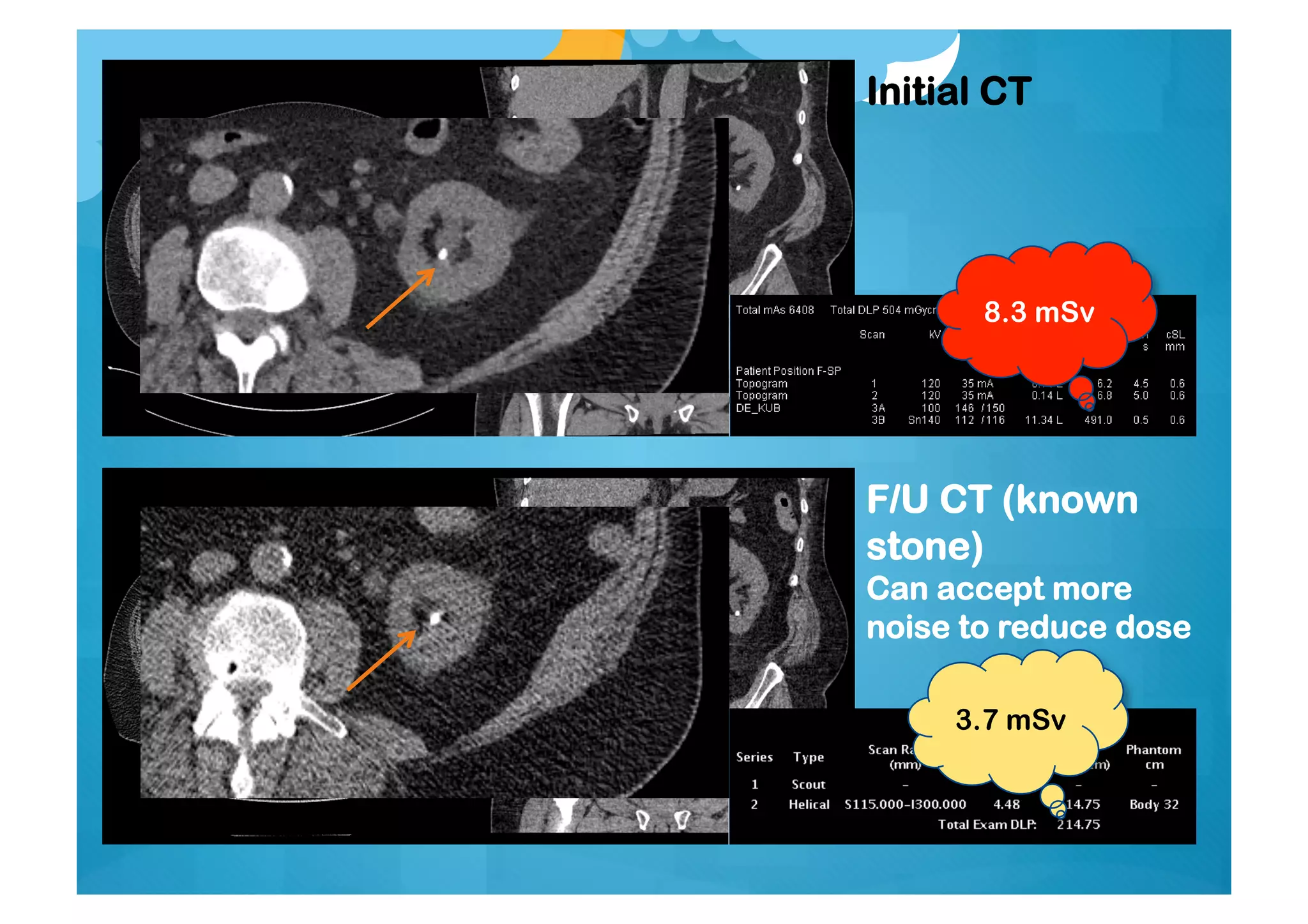
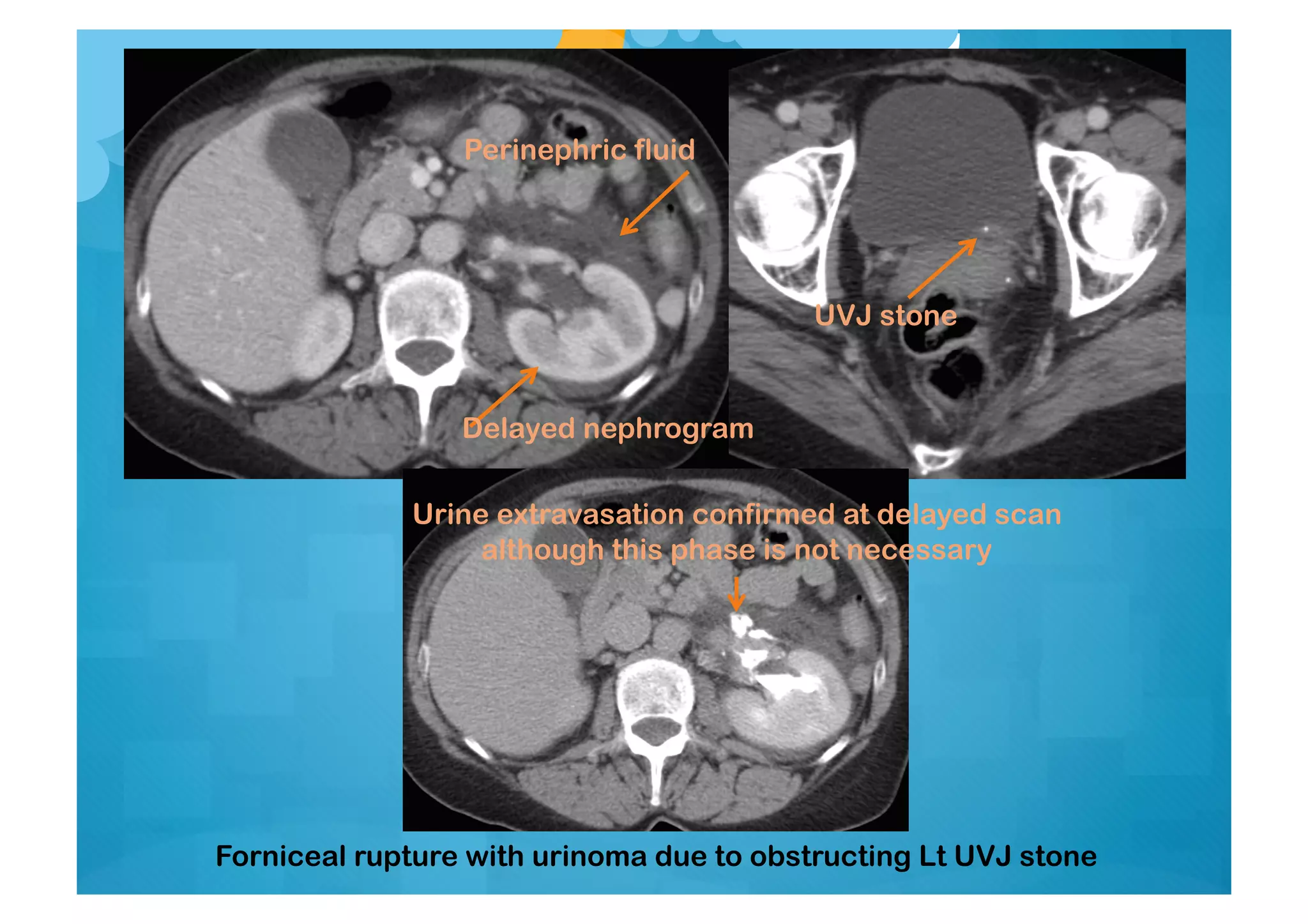
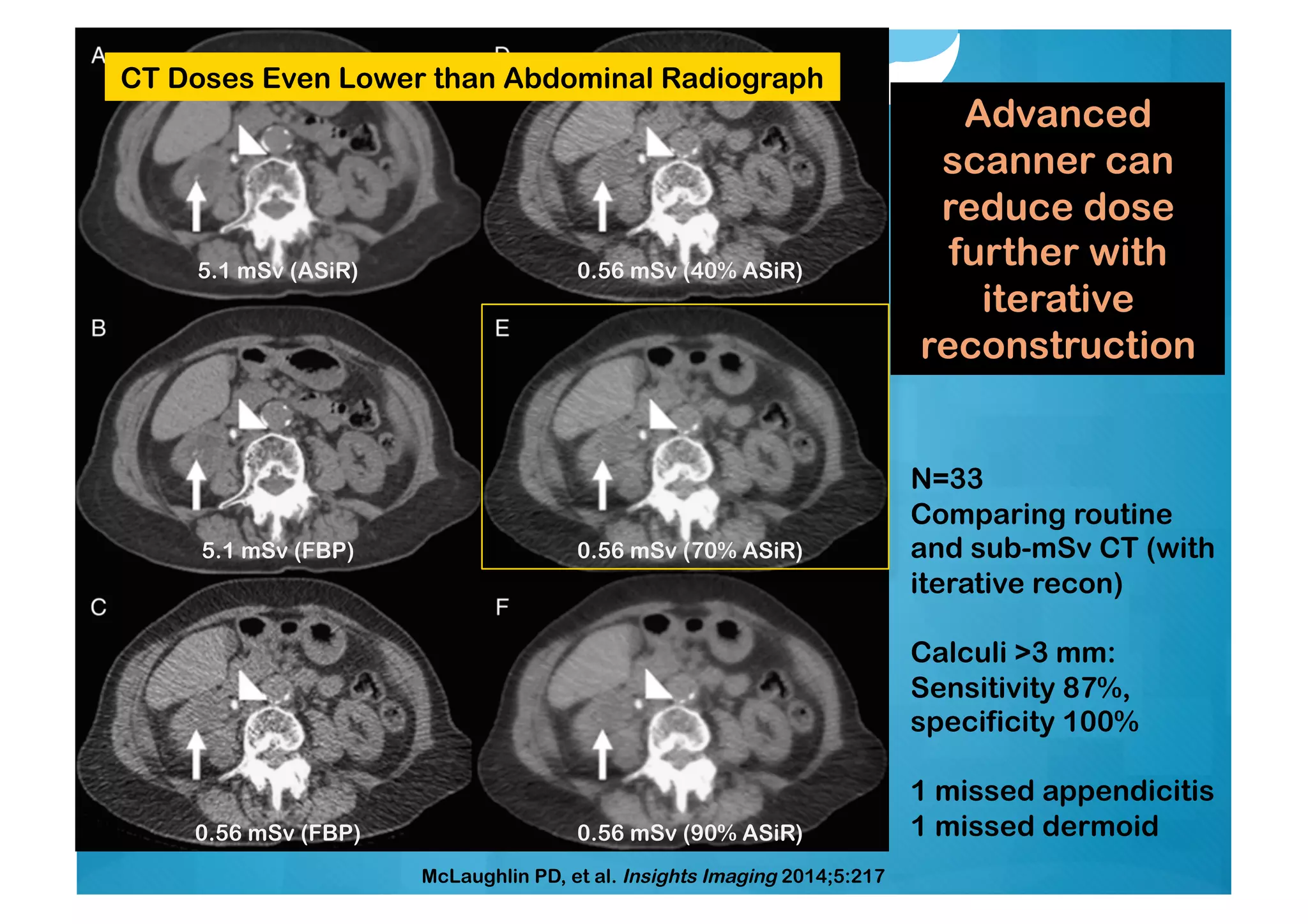
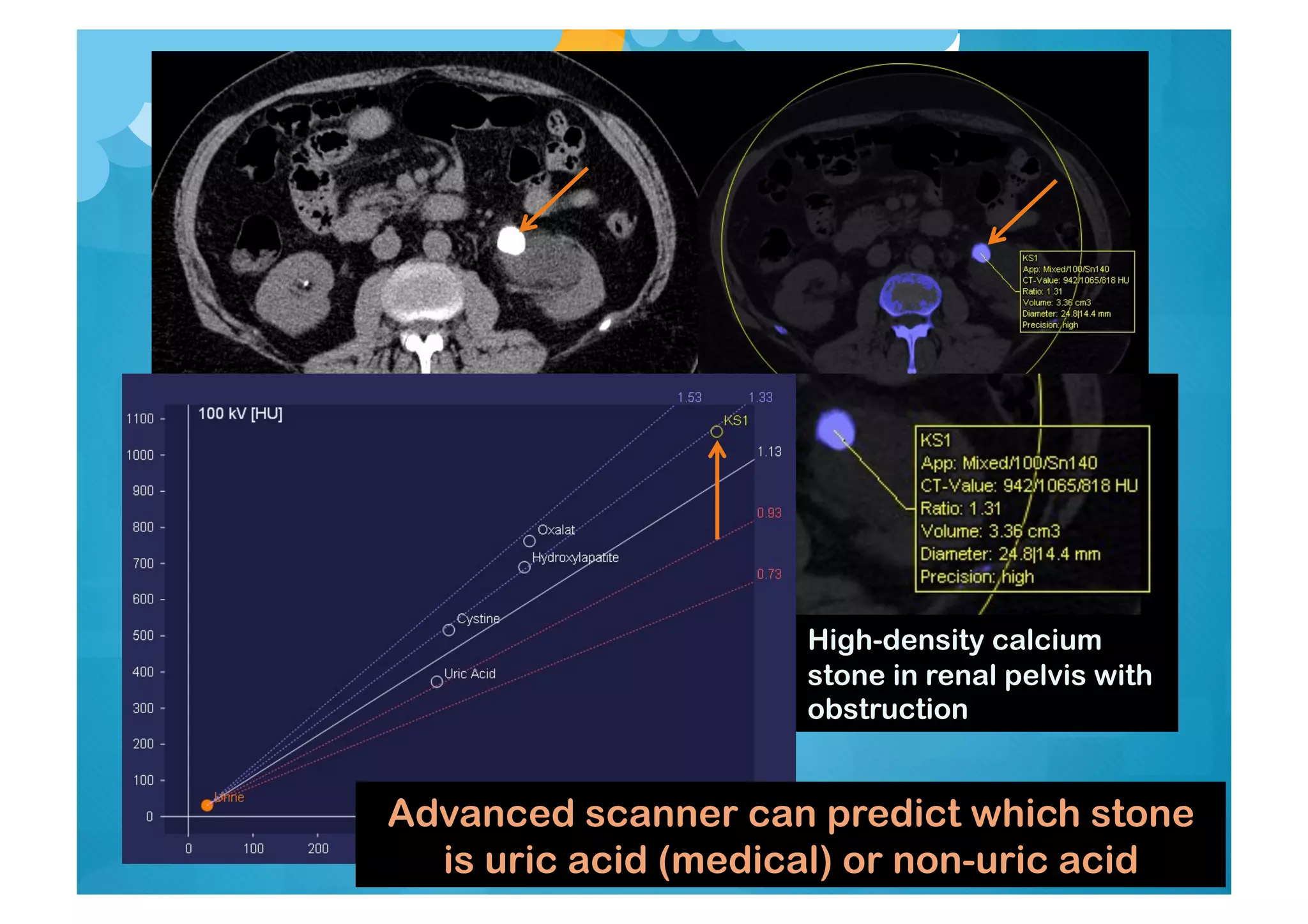
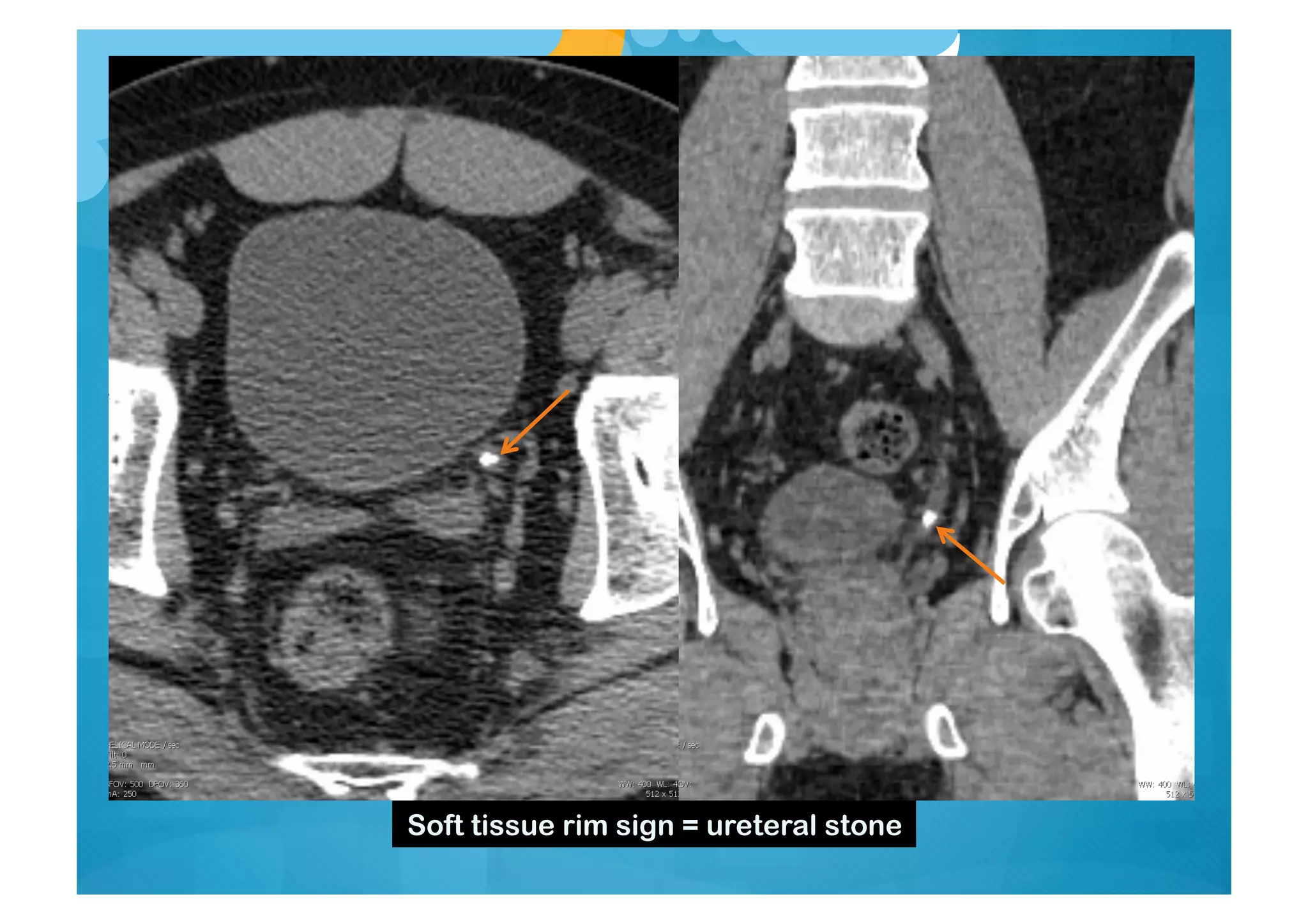
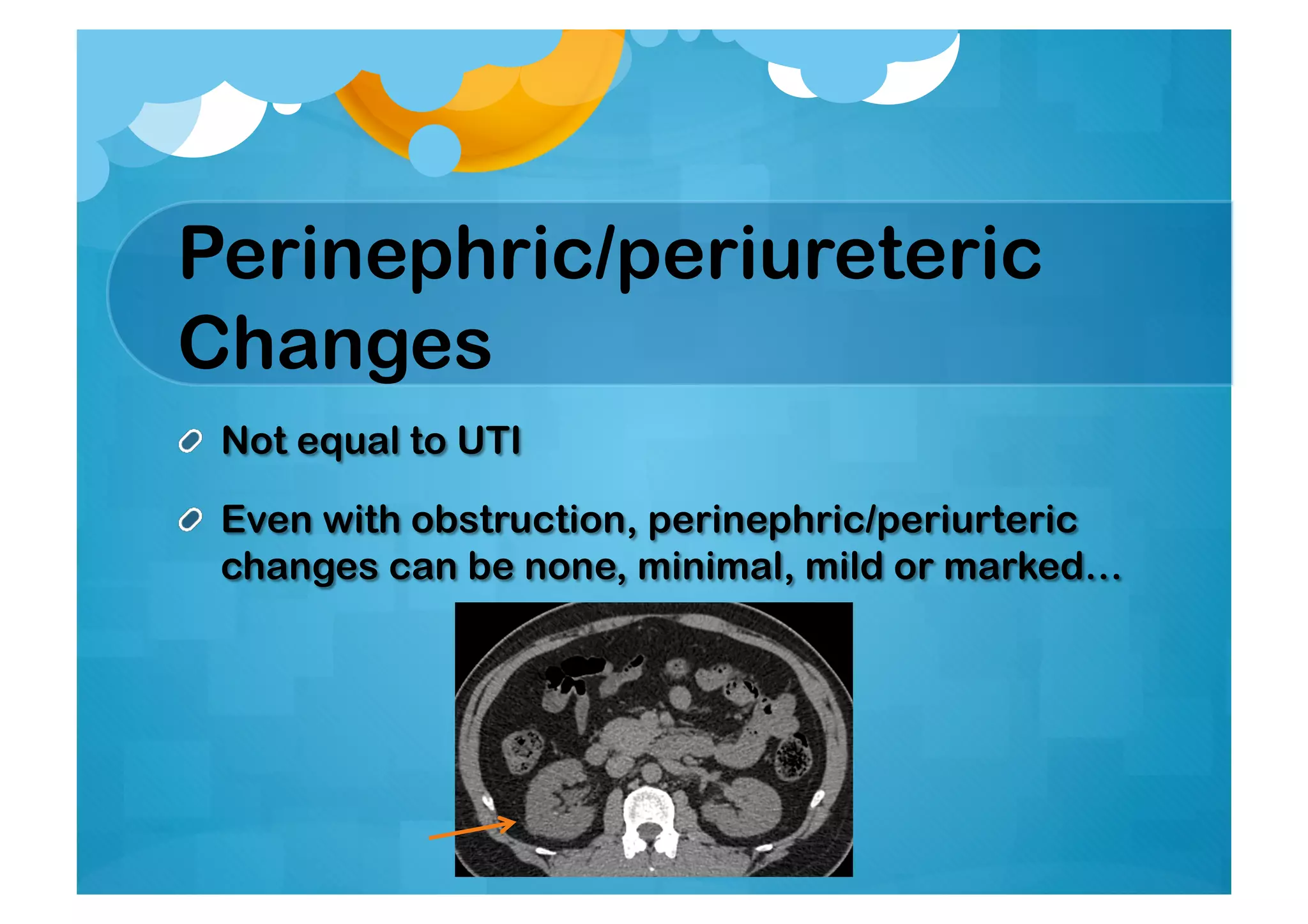
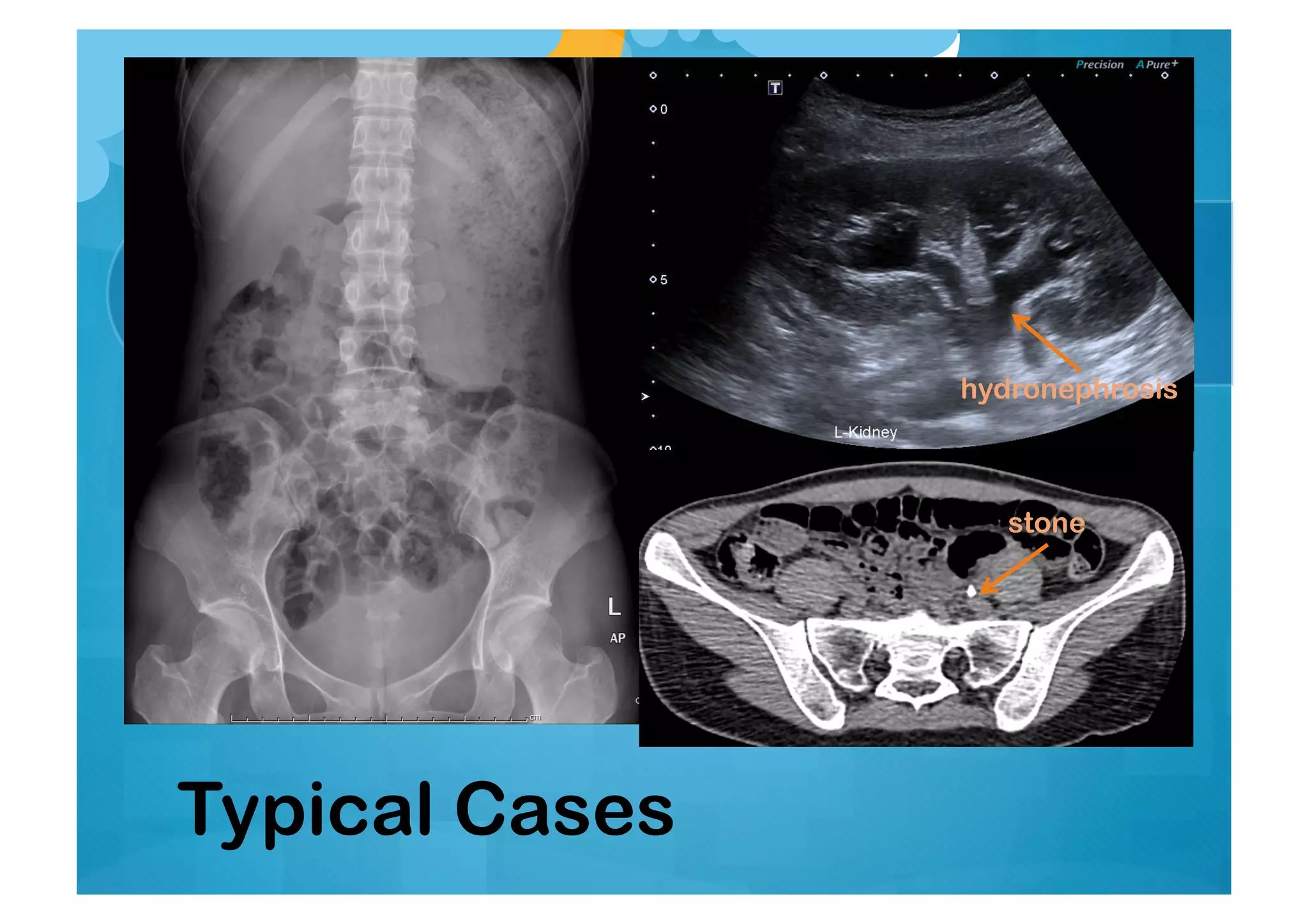
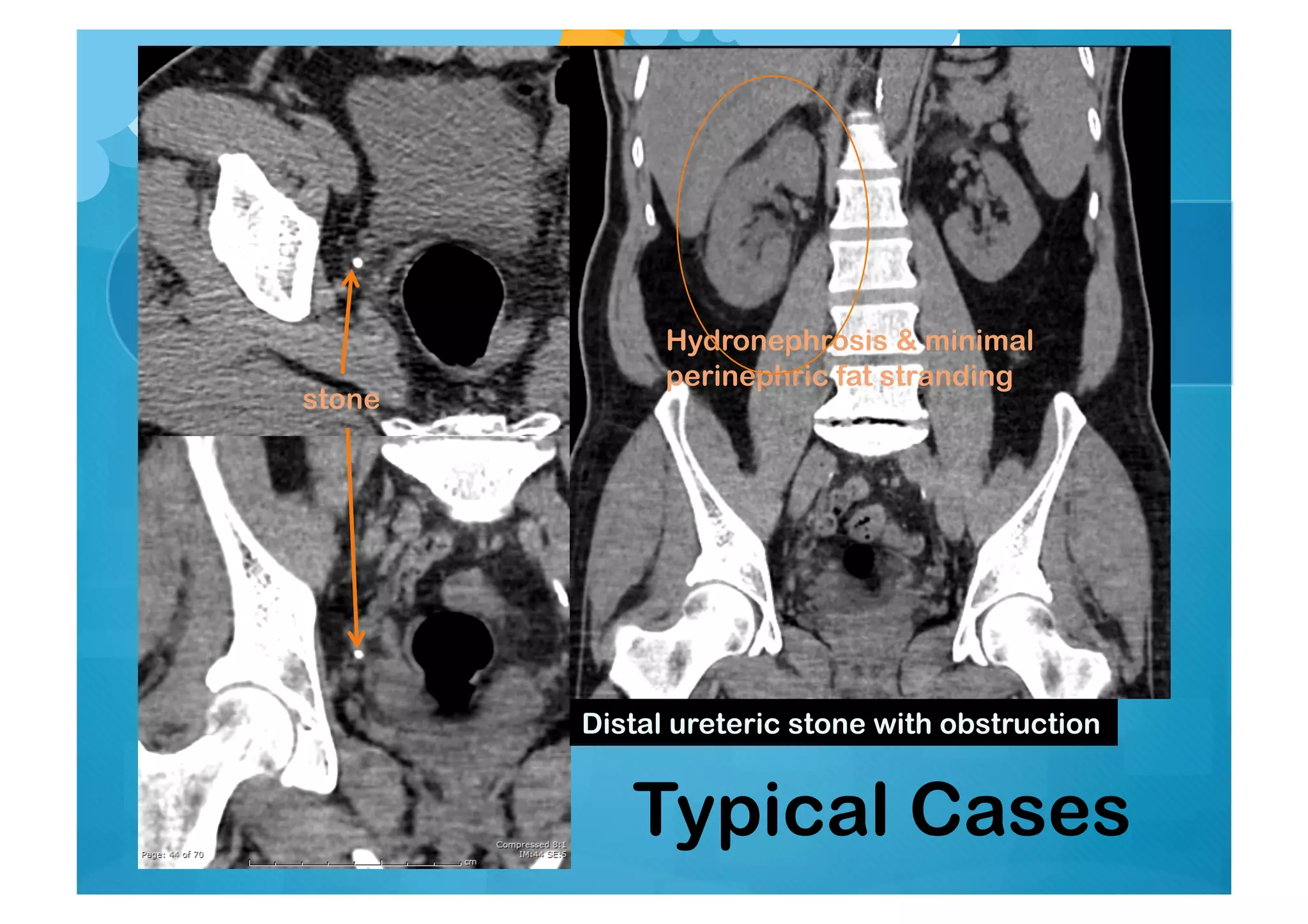
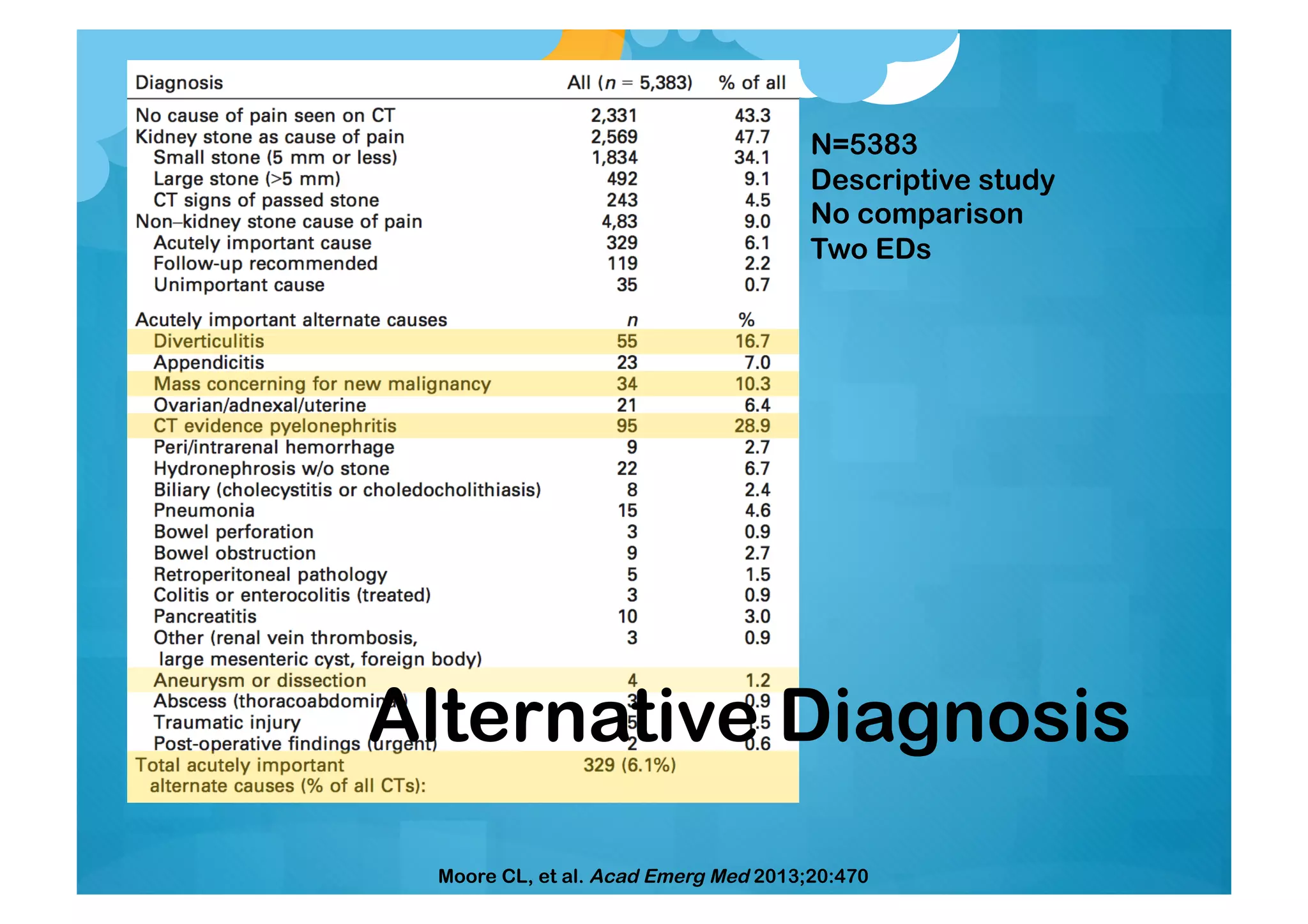
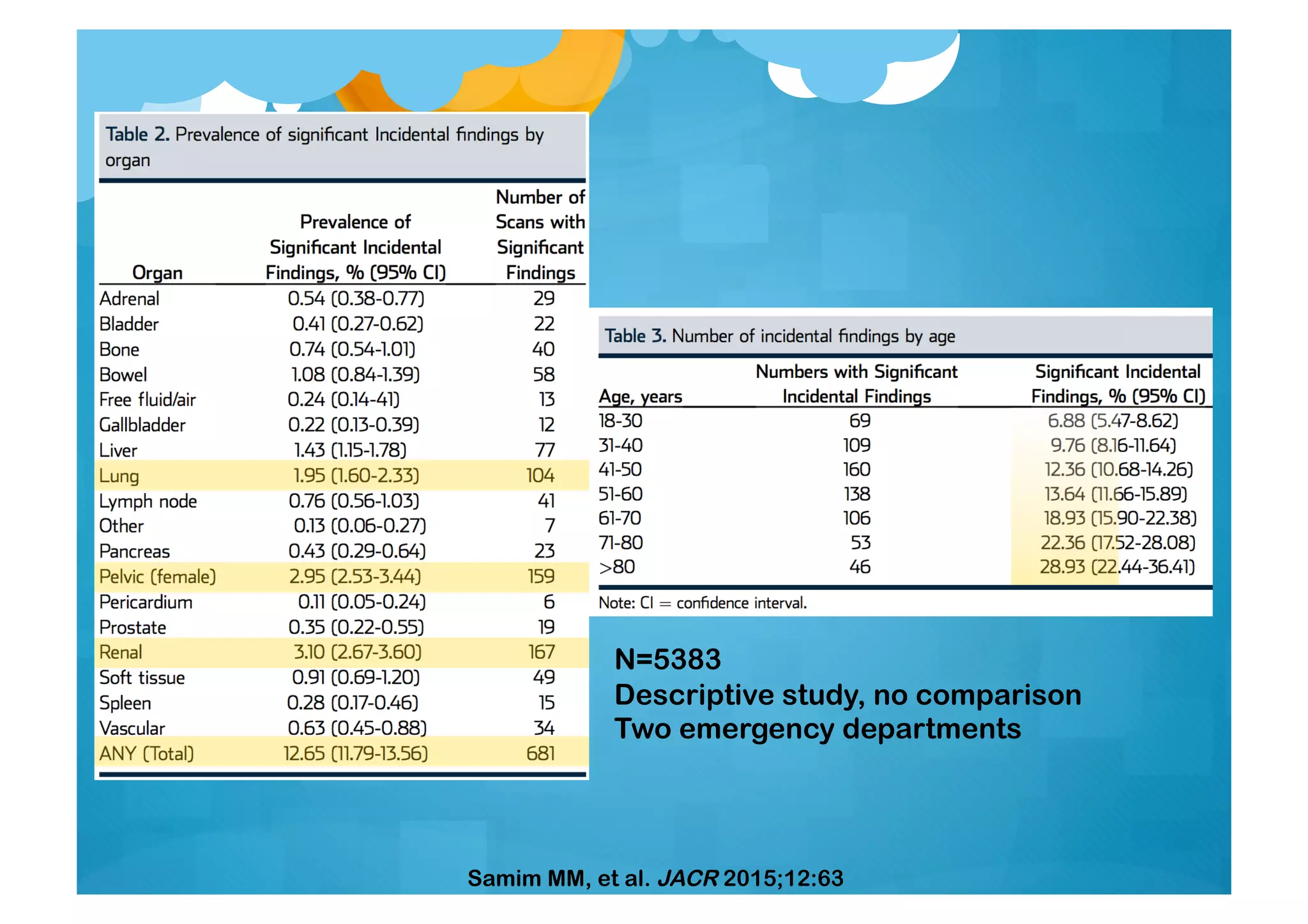
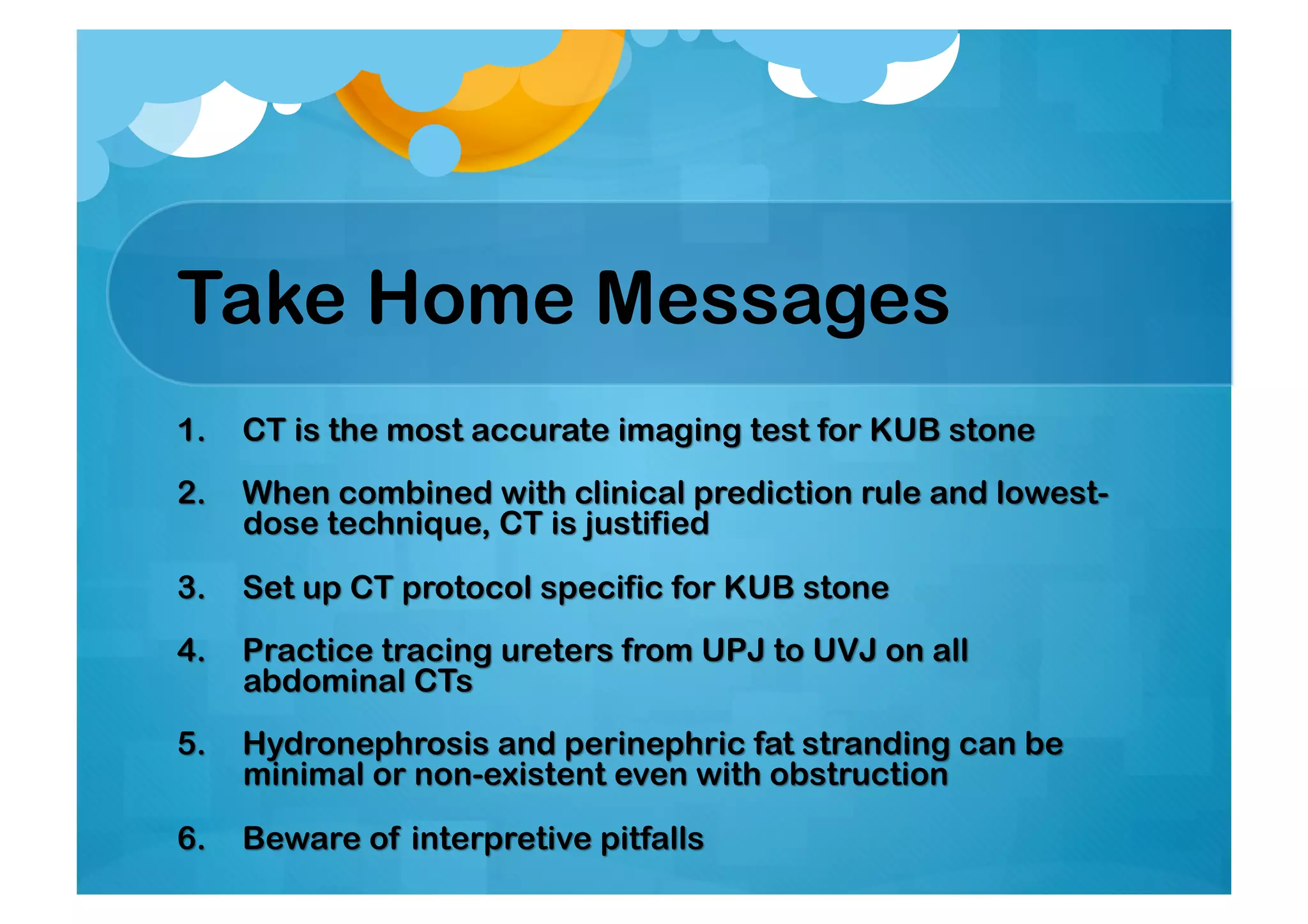
The document discusses the CT stone protocol, focusing on the reasons for using non-contrast CT for detecting kidney stones, the sensitivity and specificity of various imaging methods, and diagnostic strategies for assessing uncomplicated ureteral stones. It highlights the importance of stone composition, detection methods, and a proposed stone score to evaluate the probability of symptomatic stones. Additionally, it addresses radiation doses associated with CT scans and the interpretation of the imaging findings related to stone formation.