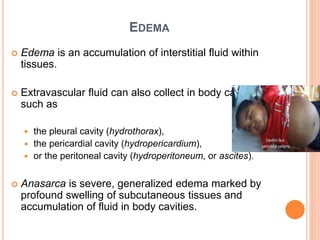
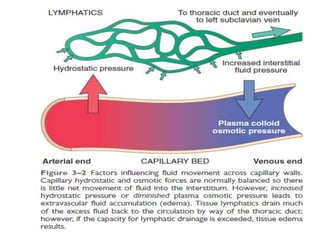
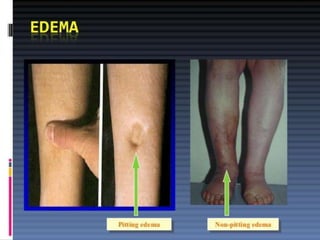
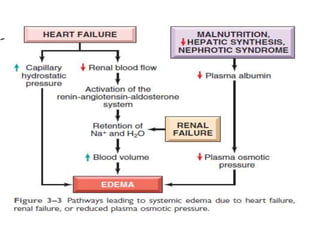
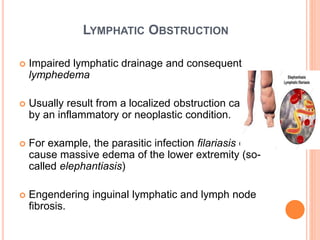
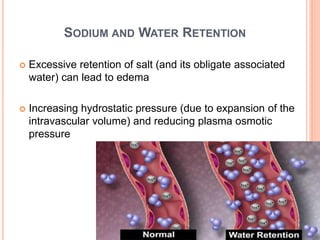
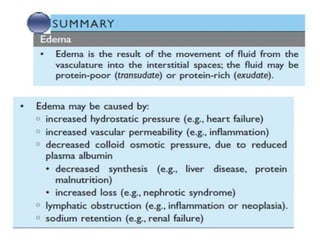
Edema is the accumulation of fluid in the interstitial spaces of tissues. It occurs when there is increased hydrostatic pressure forcing fluid out of blood vessels or decreased plasma oncotic pressure pulling fluid back into blood vessels. The two main types of edema fluid are transudate, which is low in protein, and exudate, which is high in protein due to increased vascular permeability. Common causes of edema include increased venous pressure from conditions like heart failure or DVT, reduced plasma proteins from liver or kidney disease, lymphatic obstruction, sodium and water retention by the kidneys, and increased vascular permeability during inflammation.