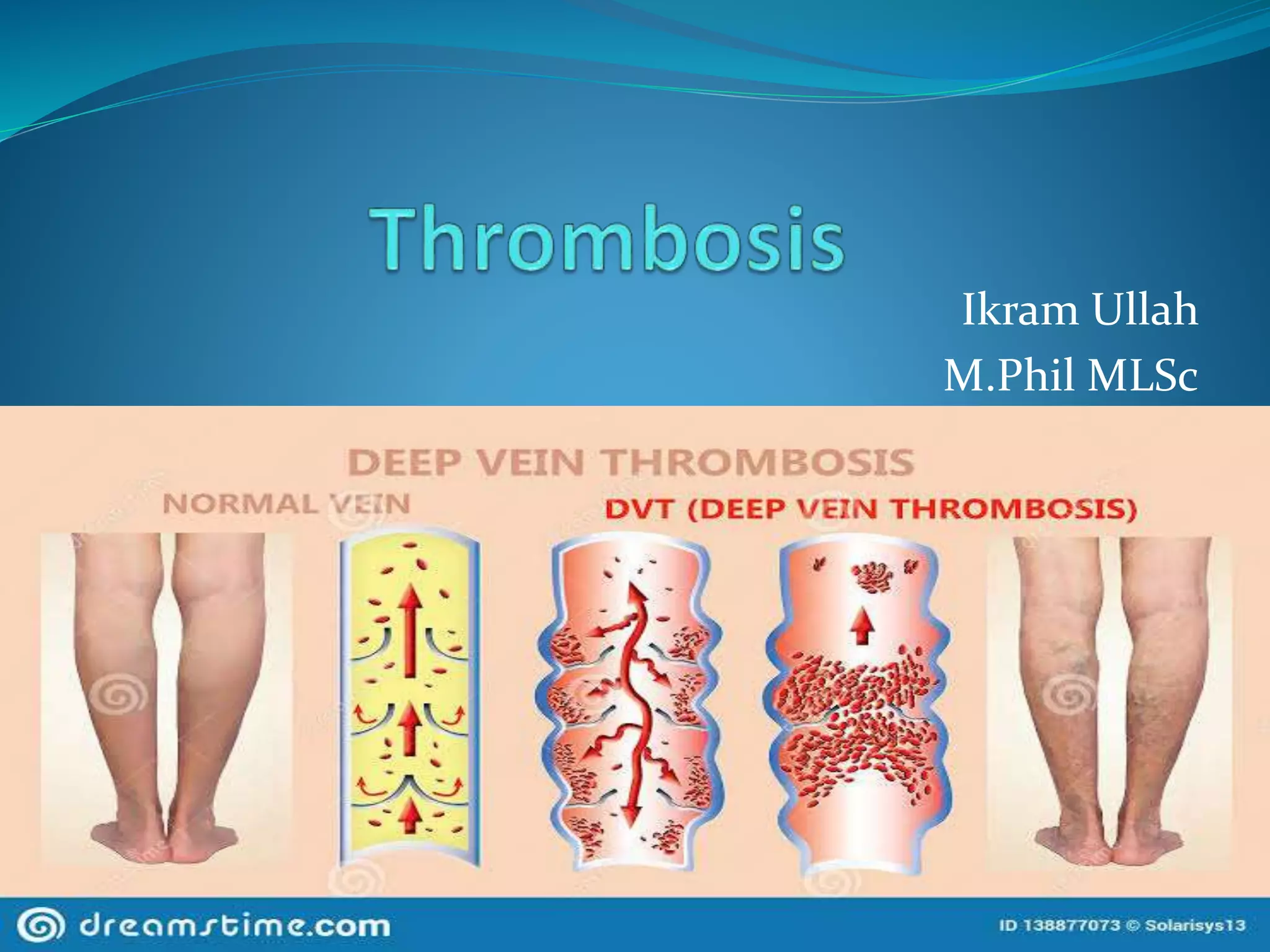
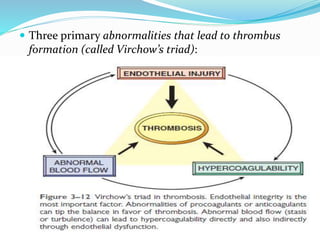
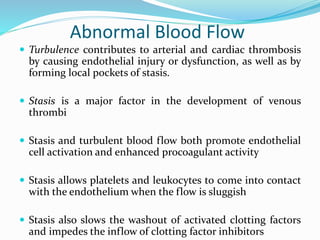
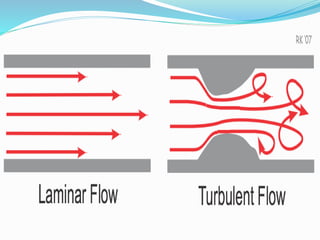
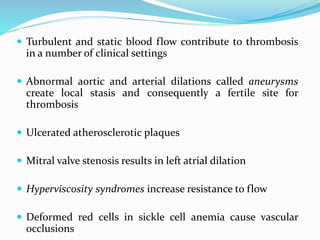
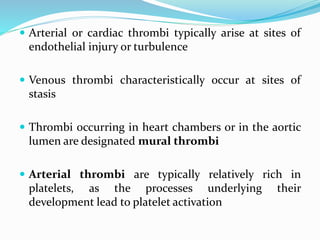
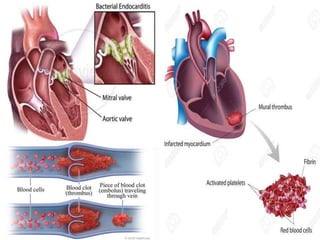
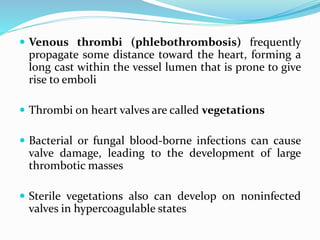
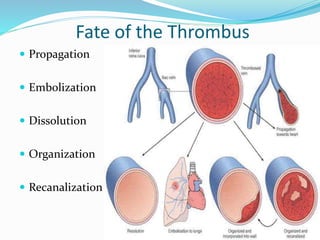
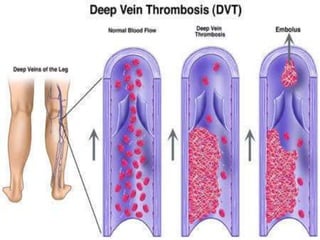
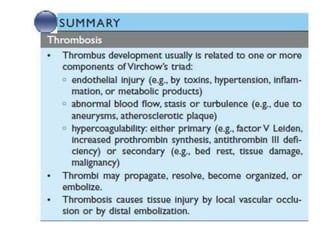
Thrombosis is the formation of a blood clot within blood vessels. A thrombus is a blood clot that forms at the site of endothelial injury or abnormal blood flow and can cause vascular obstruction. Virchow's triad describes the three main factors that contribute to thrombus formation: endothelial injury, abnormal blood flow, and hypercoagulability. Thrombi form in different locations depending on the underlying cause, and can propagate and embolize, becoming potentially life-threatening.