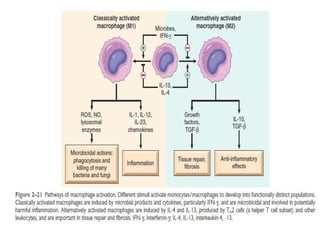
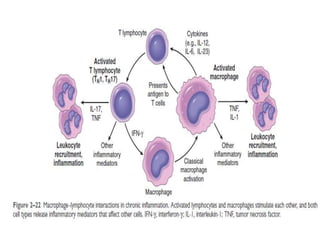
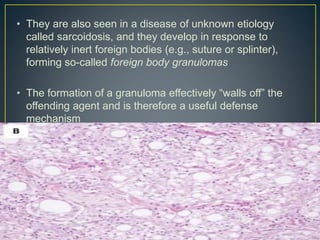
Chronic inflammation is characterized by prolonged inflammation lasting weeks to years, involving simultaneous tissue injury, healing through fibrosis, and continuing inflammation. It is driven by infiltration of mononuclear cells like macrophages, lymphocytes, and plasma cells, along with tissue destruction by their inflammatory products and repair through angiogenesis and fibrosis. Chronic inflammation can result from acute inflammation that is not resolved or from persistent infections, immune-mediated diseases, prolonged toxic exposures, or recurrent injury interrupting the healing process. The dominant cells in chronic inflammation are macrophages and lymphocytes, which secrete cytokines and antibodies driving further inflammation in many autoimmune and chronic diseases.