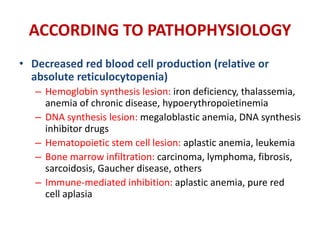
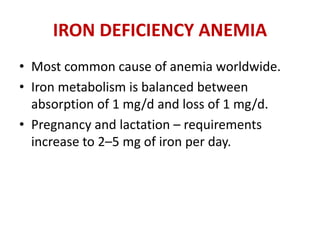
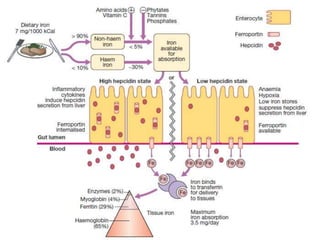
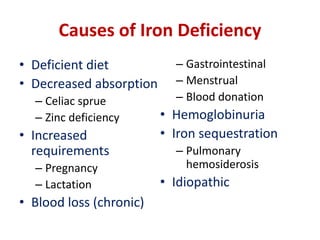
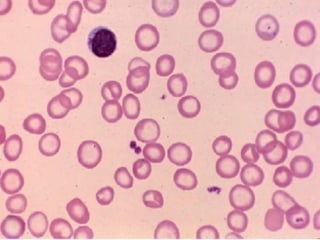
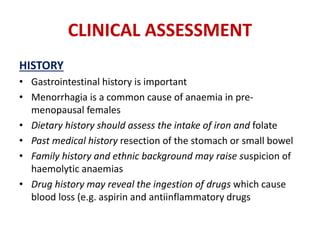
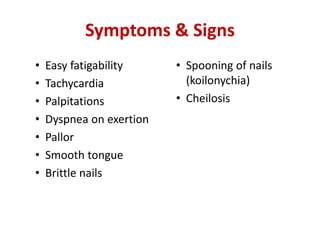
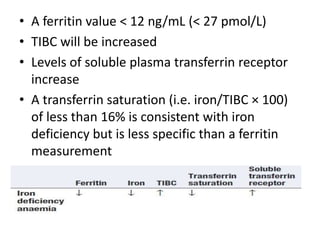
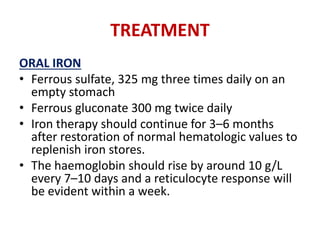
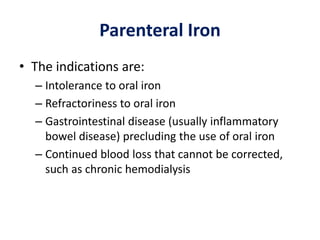
Iron deficiency anemia is the most common type of anemia worldwide. It occurs when iron levels in the body are low, preventing adequate hemoglobin production. Common causes include deficient diet, blood loss from menstruation or gastrointestinal issues, and increased needs during pregnancy or lactation. Symptoms include fatigue, palpitations, and pale skin. Diagnosis involves blood tests showing low ferritin, increased total iron-binding capacity, and transferrin saturation below 16%. Treatment focuses on oral iron supplementation, but parenteral iron may be used if oral iron is not tolerated or absorption is impaired.