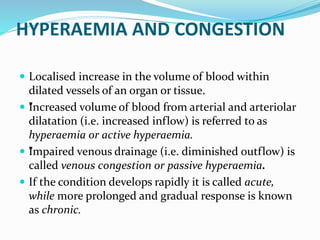
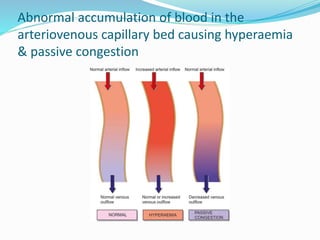
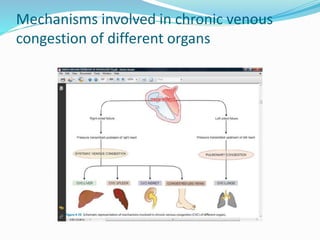
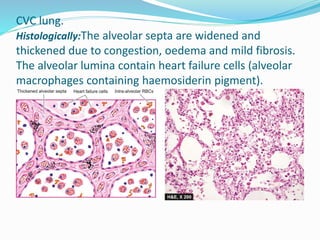
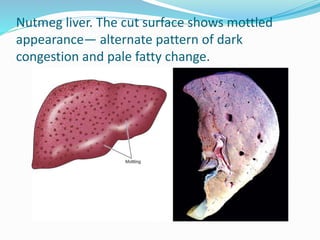
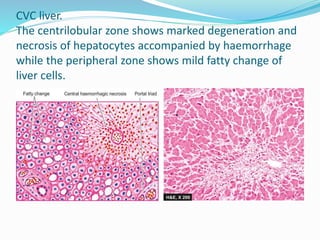
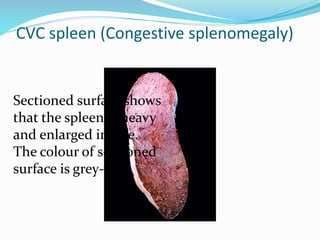
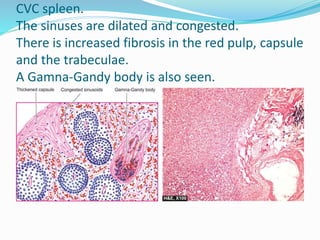
This document discusses chronic venous congestion (CVC) and its effects on various organs. It describes how CVC results in localized blood volume increase within dilated vessels. It then summarizes the gross and microscopic findings of CVC in the lungs, liver, spleen, and kidneys. The lungs show brown induration and thickened alveolar septa. The liver has a nutmeg appearance and centrilobular necrosis. The spleen exhibits congestion and fibrosis. The kidneys demonstrate mild degenerative changes. Hemorrhage and its causes, effects based on amount/speed of blood loss are also outlined.