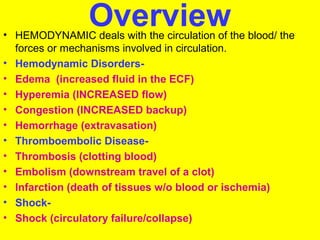
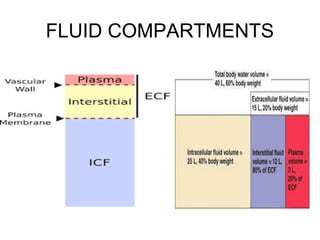
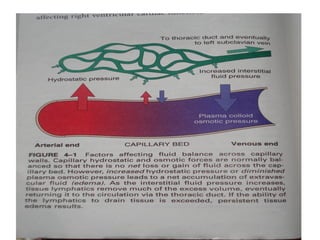
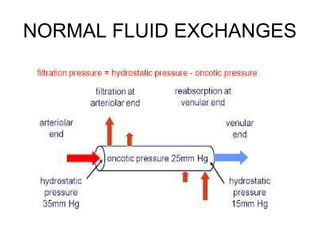
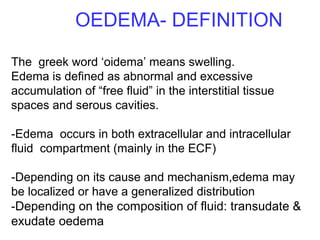
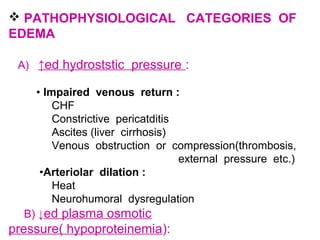
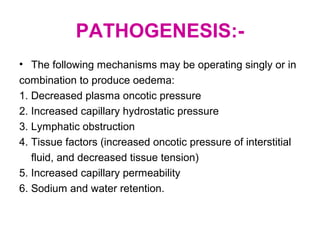
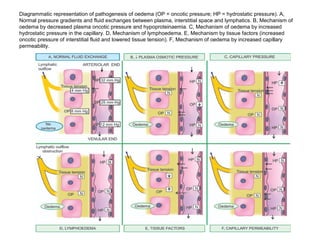
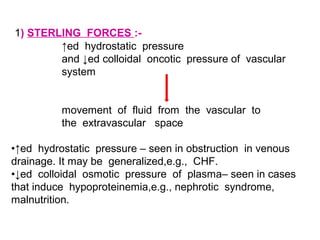
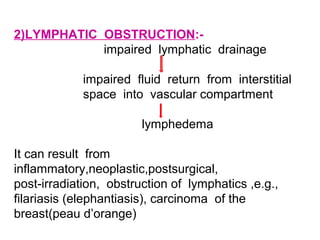
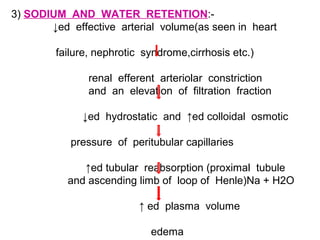
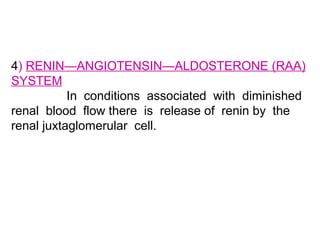
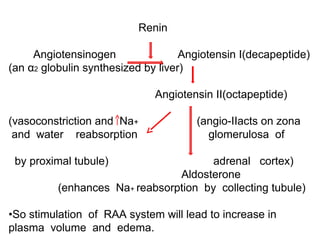
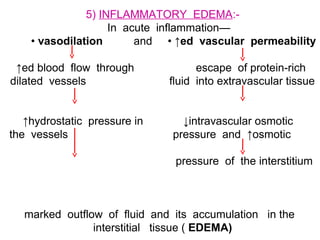
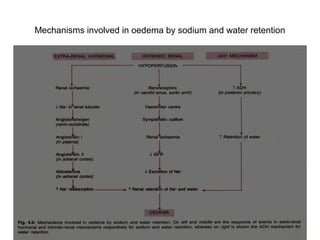
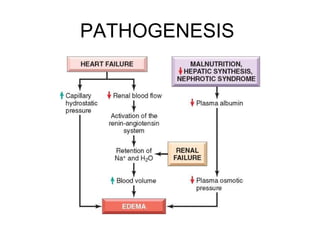
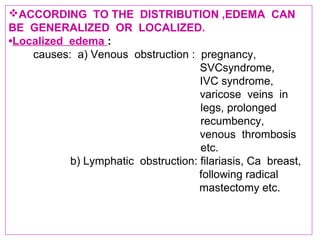
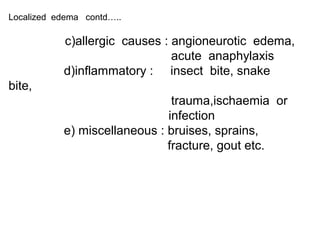
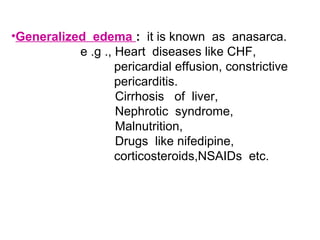
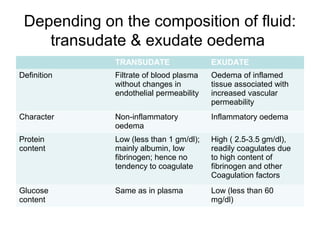
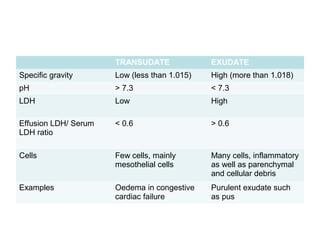
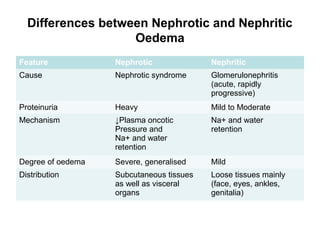
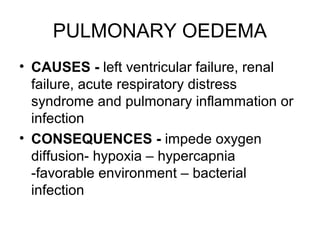
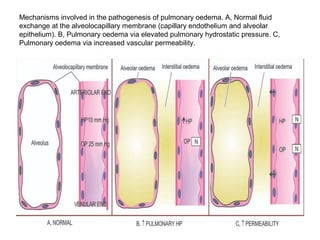
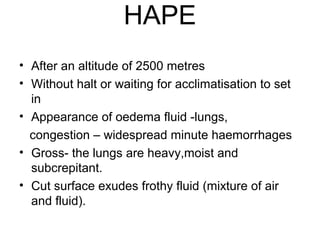
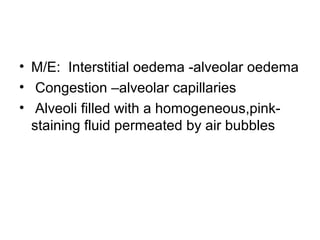
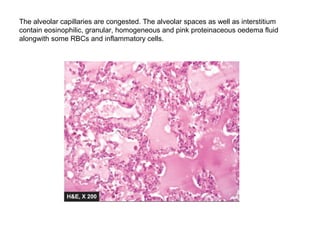
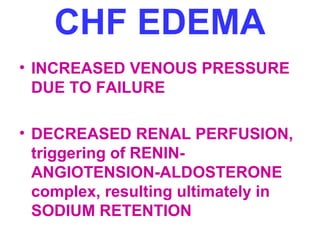
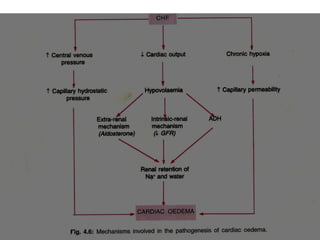
This document summarizes hemodynamic disorders and edema. It defines edema as abnormal excessive accumulation of fluid in tissues and serous cavities. Edema can be localized or generalized depending on its cause and distribution. The key mechanisms of edema formation are increased hydrostatic pressure, decreased plasma oncotic pressure, lymphatic obstruction, and sodium and water retention. Specific types of edema like pulmonary edema, cerebral edema, hepatic edema, and renal edema are also discussed. The document compares the characteristics of transudate and exudate fluids and provides diagrams to illustrate the pathogenesis of different types of edema.