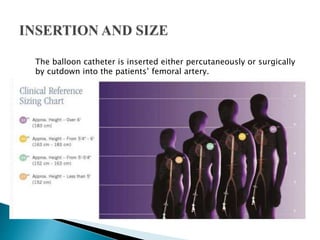
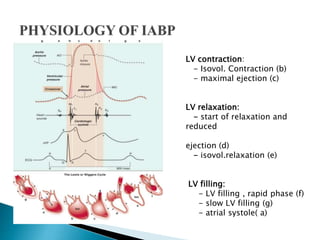
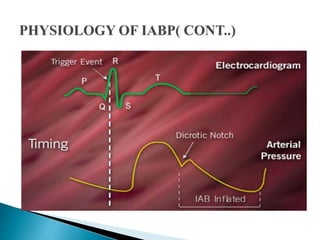
The document summarizes information about the intra-aortic balloon pump (IABP), which is a circulatory assist device used to support the left ventricle through counterpulsation. It describes how the IABP works by inflating and deflating a balloon catheter timed to the cardiac cycle to displace aortic blood. It provides details on patient criteria, device set-up, monitoring, complications, and weaning from the IABP.
![JOHNY WILBERT, M.SC[N]
LECTURER,
APOLLO INSTITUTE OF HOSPITAL
MANAGEMENT AND ALLIED SCIENCE](https://image.slidesharecdn.com/iabpnew-180620194231/85/IABP-1-320.jpg)