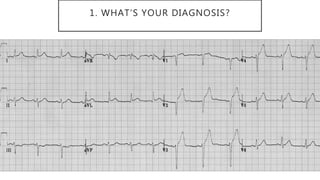
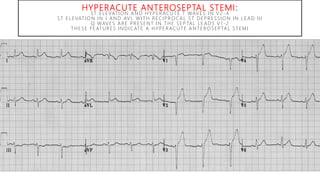
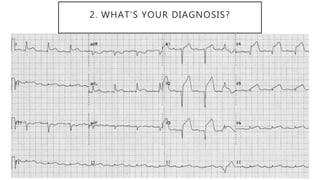
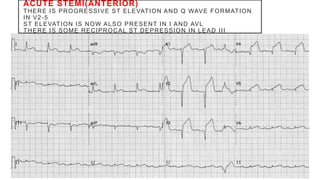
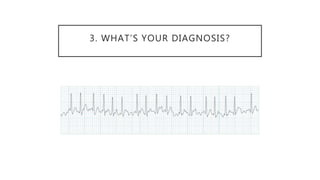
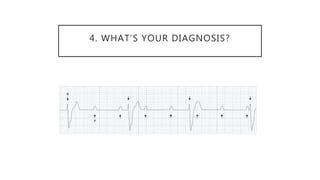
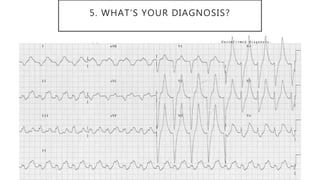
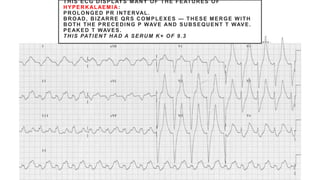
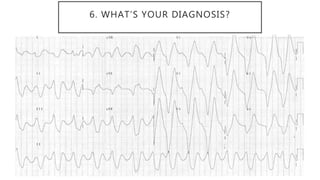
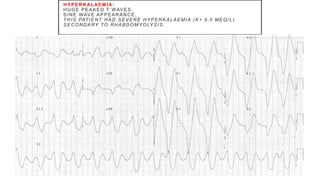
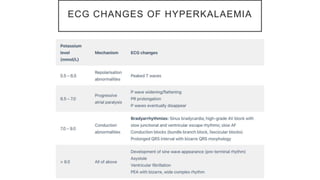
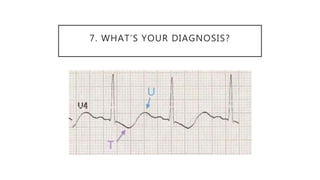
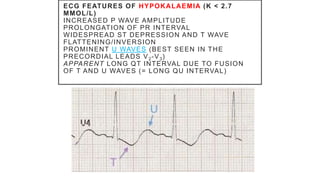
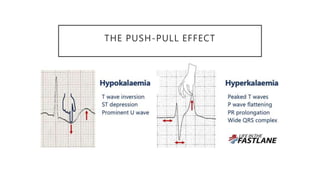
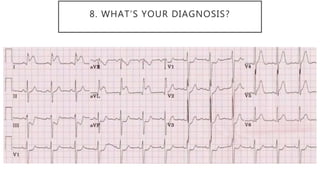
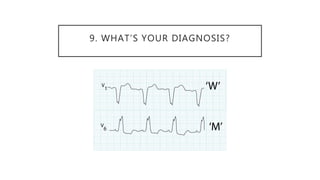
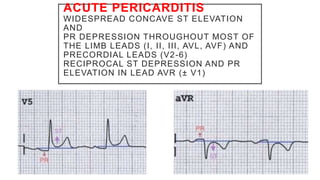
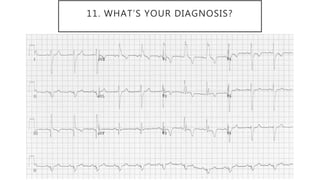
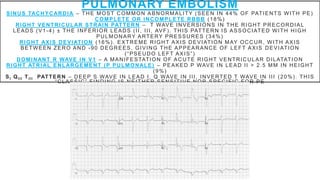
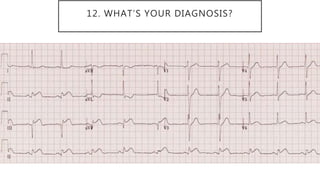
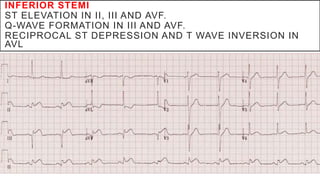
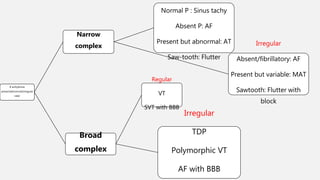
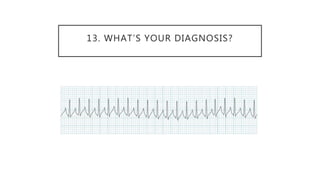
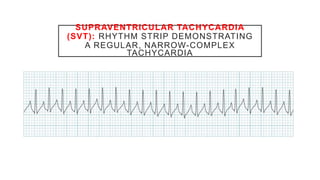
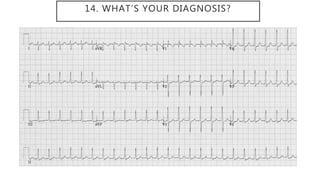
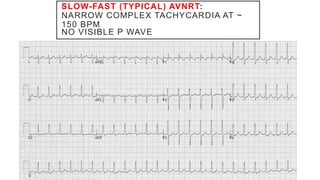
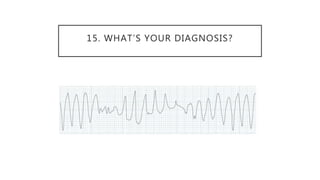
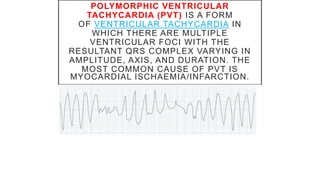
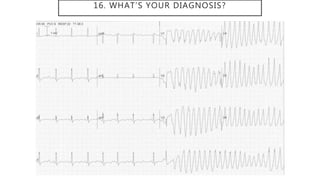
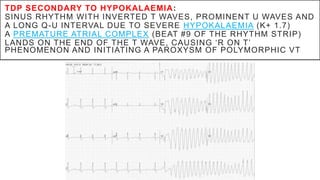
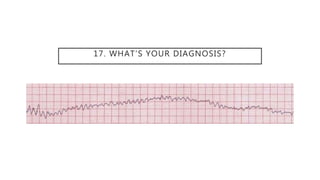
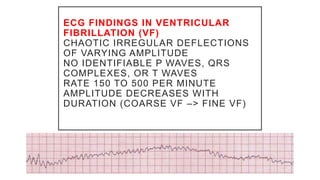
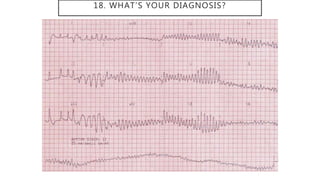
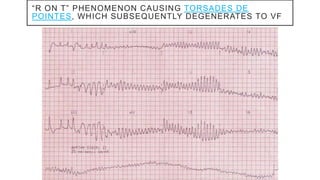
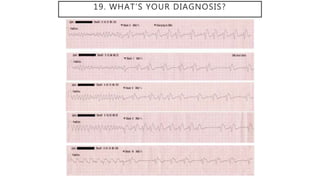
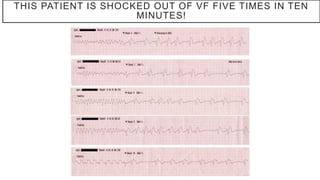
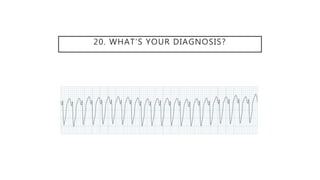
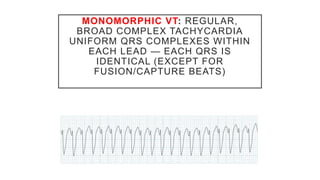
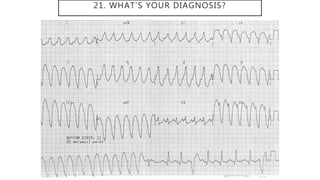
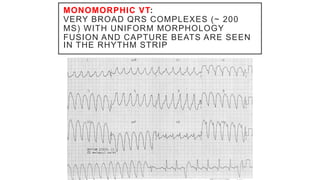
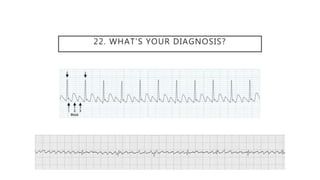
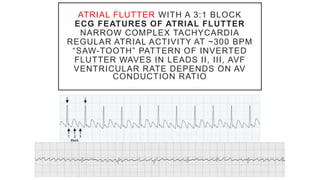
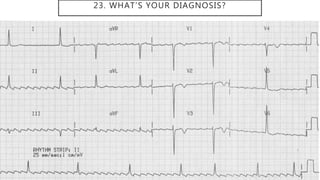
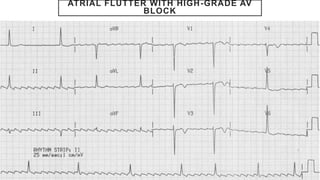
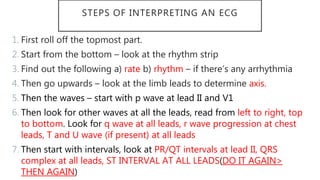
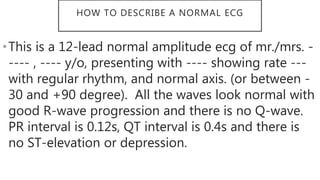
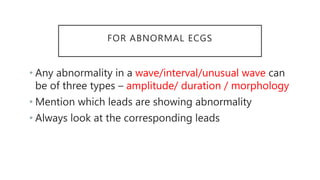
The document outlines various ECG diagnoses, including hyperacute ST elevation myocardial infarction (STEMI), atrial fibrillation, complete heart block, and hyperkalaemia, highlighting specific ECG features for each condition. It also discusses arrhythmias like supraventricular tachycardia and torsades de pointes, emphasizing the importance of ECG interpretation. A systematic approach to reading ECGs is provided, along with guidelines for normal and abnormal ECG descriptions.