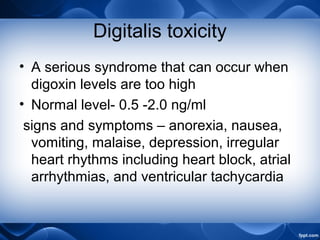
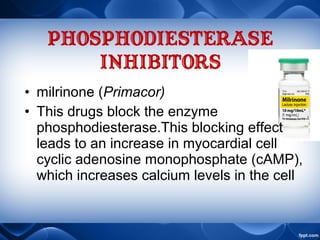
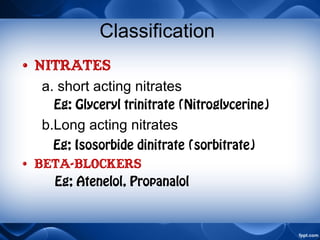
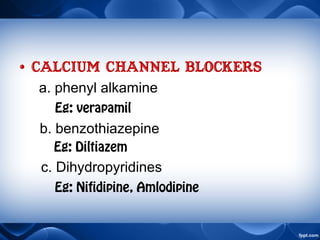
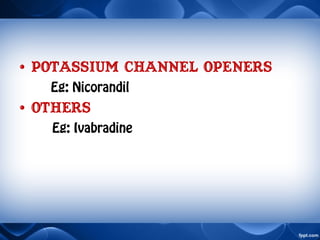
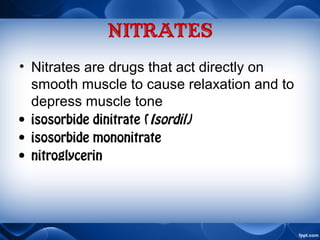
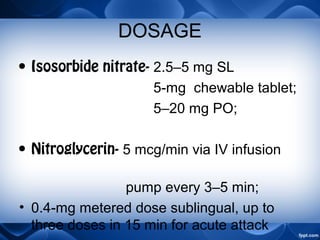
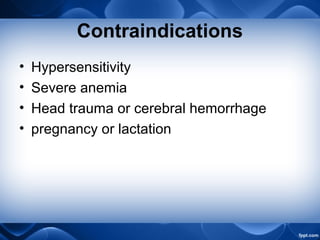
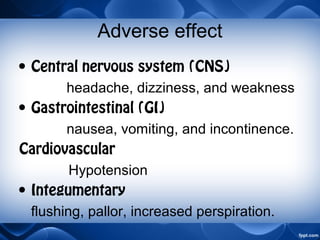
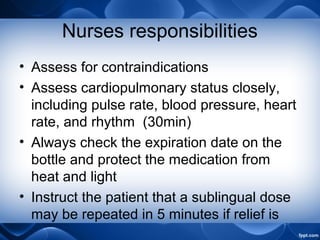
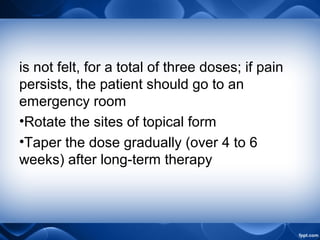
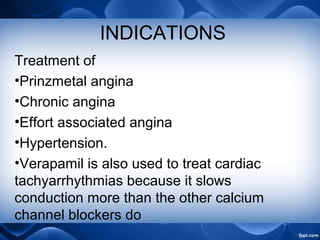
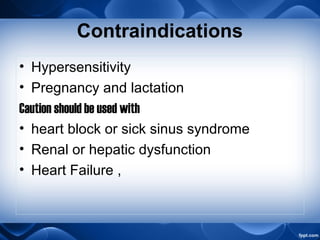
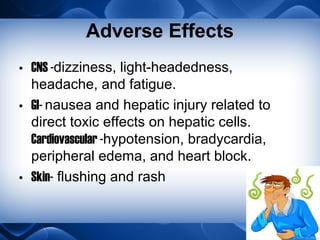
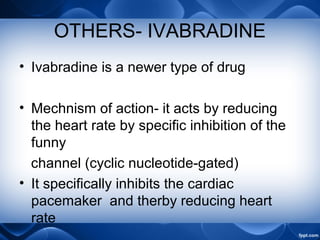
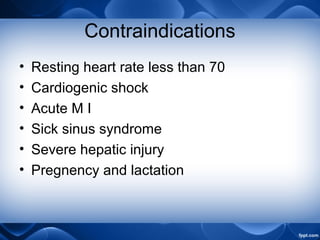
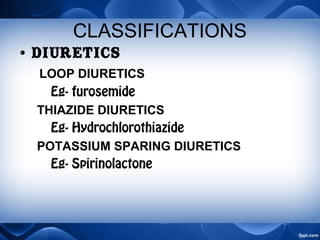
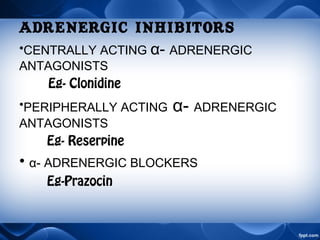
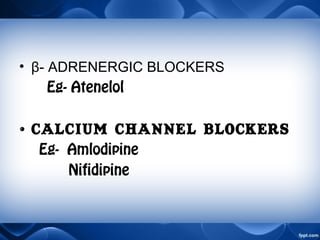
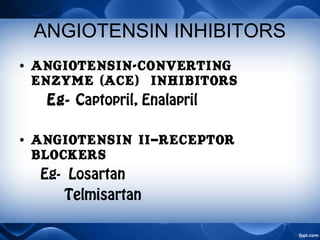
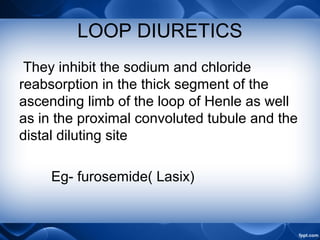
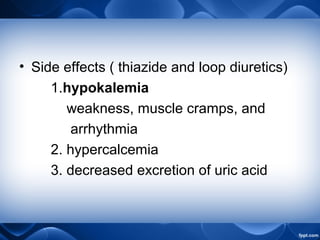
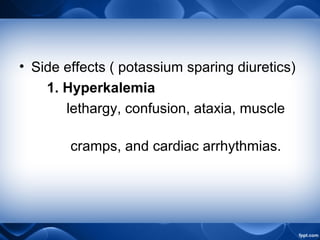
This document discusses various drugs used to treat cardiovascular conditions like heart failure and hypertension. It covers different classes of drugs like cardiotonics, antianginals, and antihypertensives. Cardiotonics like digoxin and milrinone work by increasing calcium levels in heart muscle to boost contraction and output. Antianginal drugs like nitrates, beta-blockers, and calcium channel blockers aim to restore the heart's oxygen supply-demand balance. Antihypertensive drug classes discussed are diuretics, adrenergic inhibitors, angiotensin inhibitors, and direct vasodilators. Specific drugs, their mechanisms, indications, dosages and nursing considerations are provided for each class.